QT dispersion as a predictor for arrhythmias in patients with acute ST elevation myocardial infarction
Jersey City Medical Center, Mount Sinai School of Medicine, Jersey City, New jersey 07002, USA.
|
Original Article
QT dispersion as a predictor for arrhythmias in patients with acute ST elevation myocardial infarction
Jersey City Medical Center, Mount Sinai School of Medicine, Jersey City, New jersey 07002, USA.
|
|
Abstract
Aims and Objectives: To study the effect of Heart Rate Variability (HRV) and QT dispersion (QTd) in patients presenting
with Acute ST elevation myocardial infarction (STEMI).
Methods: This is a retrospective study conducted on patients admitted with the diagnosis of acute ST elevation
myocardial infarction. In all 100 patients with acute myocardial infarction in one year were subjected to a complete
evaluation in terms of history and examination. Besides routine investigations standard 12 lead ECG was evaluated
in all cases on admission, after 4 hrs, 24 hrs, 48 hrs and on discharge.
Results: The most common presenting symptoms were chest pain (88%) and dyspnea (50%). Tachycardia was seen
in 56% while congestive heart failure was present in 29% patients. Patients who died had a higher QTd in comparison
to patients who survived.
Conclusion: Markers of autonomic regulation of heart like QTd provides valuable information about the future
course of events in a patient following acute STEMI which can be utilized to plan the future course of management
in patients especially predisposed to adverse and catastrophic outcomes.
Key words
acute ST elevation myocardial infarction, QT dispersion
J Thorac Dis 2010;2:86-88. DOI: 10.3978/j.issn.2072-1439.2010.02.02.006
|
|
Introduction
Coronary heart disease (CHD) has plagued mankind
since time immemorial. With the passage of time
contribution of CHD to the global disease burden has been
increasing by leaps and bounds (1). Acute Myocardial
infarction (AMI) represents one end of the spectrum of
CHD. About 50% of deaths due to AMI occurs within 1
hr of the event and are mainly attributable to arrhythmias;
late causes of death include electromechanical dissociation,
cardiac rupture, cardiogenic shock etc. Full understanding
and recognition of these changes is still lacking but
several investigators suggest that the early and long
term prognosis of the patient after AMI is determined
by the alterations in the level and kind of autonomic
control to the heart (2, 3). Experimental evidence of the
association between propensity for lethal arrhythmias and
either enhanced sympathetic or reduced Vagal activity has led to development of quantitative and qualitative
markers of autonomic activity. QT dispersion (QTd)
has been suggested as one such marker of automatic
tone of the heart. QT dispersion ref lects differences
in the local myocardial repolarization and hence the
electrophysiological environment. Clinical interest in
QTd on the surface ECG is based on the observation that
regional heterogeneity of action potential in adjacent
cardiac muscle tissue can initiate and sustain ventricular
arrhythmias especially in vulnerable myocardium like that
in ischemic heart disease (IHD) (4,5).
|
|
Material and methods
This was a retrospective study on the patients admitted
with the diagnosis of acute ST elevation myocardial
infarction in the last four years. One year records were
obtained for the patients of ST segmented elevated acute
myocardial infarction. The records of all the patients were
subjected to a complete evaluation in terms of history and
examination and then for results of further specialized
investigations.
Patients were included in the study if they fulfilled all of
the following criteria:
• History suggestive of acute coronary syndrome
within the preceding 48 hrs of admission.
• ST segment and T wave changes typical of myocardial
infarction.
• Positive cardiac markers: cardiac troponin T or CPK
– MB
Patients were excluded from the study if they had any of
the following:
• Presentation after 48 hrs.
• Prior ECG showing QRS duration > 120 msec (LBBB
or RBBB)
• Previously on drugs affecting QRS interval or heart
rate variability
• Diagnosed case of conditions affecting QT dispersion
or heart rate variability: Diabetes, CHF, valvular heart
disease,
• Non-ST elevation Myocardial Infarction.
The standard 12 lead standard EKG were evaluated for
all the cases on admission, after 4 hrs, 24 hrs, 48 hrs and
on 7th day of admission on ECG strips running at speed
of 25 mm/sec and at a setting of 1mv=10mm. QT interval
was measured manually from the onset of QRS complex to
the end of T wave. The end of T wave was considered the
point of return to the isoelectric line. EKGs in which the
QT interval was not measurable in more than 8 leads were
excluded from the study. If “U” waves were present then
QT interval was taken from the beginning of QRS complex
to the lowest point between T and U wave.
QT correction was deduced using Bazett’s formula i.e.
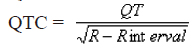 QT dispersion was calculated as, QTd = QTmax – QTmin
We then observed the disease course in these patients.
The important prospective of this study was to determine if
QTd measurement early in the course of presentation, has
any prognostic effect.
Statistical Analysis was done using Student ΄t΄ test for
unpaired samples to compare the differences between two
groups. Paired ΄t΄ test was used to check the significance of
difference between observed values within the same group.
|
|
Results
The most common presenting symptoms were chest
pain (88%) and dyspnea (50%). Tachycardia was seen in
56% of the patients while congestive heart failure was
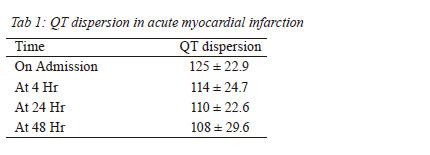
present in 29% patients (Fig 1). During QTd analysis the
maximum dispersion that occurred on admission was 124.5
± 22.9 ms, which declined progressively with time to 110
± 22.6 ms after 24 hours and 94.3 ± 16.3 ms on discharge
(Table 1 & Fig. 2). The maximum QT dispersion was
172 ms and minimum was 94 ms in the study group on
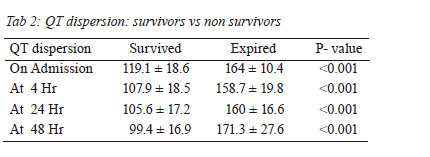
admission. The patients with any arrhythmic event during
hospital stay were found to have QT dispersion of 164±10.4 ms at admission. On the other hand, Patients without
any arrhythmic event were found to have QT dispersion of
119.1 ± 18.6 ms at admission. While comparing these two
groups P value was found to be < 0.001 (Table 2 & Fig. 3).
No event occurred after 48 hours.
  |
|
Discussion
The primary finding of this study is that measurement of QTd early in patients with STEMI is a useful prognostic
factor; its analysis can predict patients at higher risk of
adverse outcomes. The mean age of study subjects was
53.5 ± 10.0 years. The maximum number of cases was ≥ 50
years (72%); within this group the incidence was highest
in 51-60 years (36%). An interesting finding was that none
of the patients was more than 75 years of age. Females
constituted around 30% of patients with the maximum
number lying in 51-60 year age group however their ratio
with males increased progressively with age to reach a
value of 1:1 after 70 years.
The most common complaint in patients diagnosed with
STEMI has usually been chest pain. Its incidence was 96%
in the study of Richman (6). Other common presentation
during various studies had been diaphoresis, nausea,
dyspnea, and light-headedness (6,7). In our study the
incidence of chest pain was slightly less at 88% followed by
dyspnea in 50%. Vomiting was seen in 40% of patients and
profuse sweating episode in 38%.
In the present study mean QT dispersion was highest
on the day of admission (124.5±22.9 ms) and it declined
progressively to 110±22.6 after 24 hrs and to 94.3±16.7
on seventh day of admission. Patients of anterior wall
MI had significantly greater QTd than non-anterior wall
MI (on admission 137.3±16.6 versus 101.8±13.1 p<0.001).
This difference was maintained throughout the course
of hospital stay of the patients. Similar results had been
obtained by other authors in their studies (8,9,10), though
these studies evaluated QT dispersion after 12 hours
of admission, unlike ours where we evaluated QTd on
admission and subsequently at 4 hours, 24 hrs, 48 hrs and
on the 7th day of admission.
In conclusion, it can be said that markers of autonomic
regulation of heart like QTd provides valuable information
about the future course of events in a patient following
acute ST elevation MI and it can be utilized to tailor the
pace and course of management in patients especially
predisposed to adverse and catastrophic outcomes. Moreover a strict regulation of autonomic tone in such
patients may improve the prognosis in such patients.
|
|
References
Cite this article as: Aziz F, Doddi S, Alok A, Penupolu S, Singh V, Benz M, Abed M. QT dispersion as a predictor for arrhythmias in patients with acute ST elevation myocardial infarction. J Thorac Dis 2010;2(2):86-88. doi: 10.3978/j.issn.2072-1439.2010.02.02.006
|