Should primary tumor be resected for non-small cell lung cancer with malignant pleural disease unexpectedly found during operation?—a systemic review and meta-analysis
Introduction
Non-small cell lung cancer (NSCLC) with malignant pleural disease (MPD) including malignant pleural effusion (MPE) and malignant pleural nodules (MPN) is considered to have poor outcomes, which happens on 1–7% of NSCLC patients (1-4). According to The International Association for the Study of Lung Cancer (IASLC) staging project, the median survival time (MST) and the 5-year survival rate of patients with malignant pleural disease were 8 months and 2%, respectively (2). Thus, in the seventh edition of the Union for International Cancer Control (UICC) lung cancer staging system, NSCLC with malignant pleural disease was clarified as stage IV (M1a) (5). Due to its poor prognosis, NSCLC with MPD is generally regarded as a contraindication for surgery, and this part of patients are usually treated by systemic chemotherapy (3,6).
However, in clinical practice, despite advances in diagnostic imaging techniques in recent years (7), malignant pleural disease cannot always be detected before surgery and are sometimes found during operation. Among them, whether to undergo surgical resection of the primary tumor or not is still controversial. A few studies have been published while their findings were inconclusive (8-12). Yet no randomized controlled trial has been performed to assess the role of primary tumor resection in NSCLC patients with MPD first detected during surgery.
Therefore, the purpose of this meta-analysis was to clarify whether or not the surgical removal of the primary tumor should be taken and further investigate the other prognostic factors among NSCLC patients with MPD first detected during surgery and those who undertook primary tumor resection.
Methods
Search strategy
We searched articles published in the PubMed, Embase and Web of Science update to May. 11, 2016 by using the following search terms: lung cancer, lung carcinoma or lung neoplasm, pleural, pleural dissemination, pleural seeding, pleural spread or pleural carcinomatosis, and surgical resection, pulmonary resection or primary tumor resection. References of related studies were identified manually for potential eligible studies.
Inclusion and exclusion criteria
Studies met the following criteria were included in our meta-analysis: (I) studies recruited NSCLC patients with MPD first detected during surgery; (II) investigated the surgical benefits of pulmonary resection and/or assessed other prognostic factors of NSCLC patients with MPD first detected during surgery; (III) hazard ratio (HR) with 95% confidence interval (95% CI) was available in univariate or multivariate analyses with Cox proportional hazards model or could be estimated by Parmar’s method (13) for primary tumor resection or other prognostic factors. Articles were excluded from the present study if they: (I) were conference literatures; (II) recruited patients with contralateral lung metastasis or distant metastasis; (III) included patients who were diagnosed as NSCLC with MPD before operation. Two trained reviewers browsed abstracts and selected articles based on the inclusion and exclusion criteria, and any disagreement was solved by discussion.
Data extraction
Data were extracted independently by the two reviewers with standard extraction table. The two reviewers got coherent conclusion after discussion, and information are extracted as follows: the first author, publication year, ethnicity, source of patients, type of studies, number of patients included, HR with 95% CI for primary tumor resection or other prognostic factors.
Statistical analysis
HR and 95% CI were applied to evaluate the survival influence of primary tumor resection and prognostic role of potential factors, and the P value <0.05 meant that the results had statistical significance. It should be noted that when the author did both univariate and multivariate analysis on prognostic factors, we included the outcomes carried out by multivariate analysis in our meta-analysis. We further conducted subgroup analysis stratified by analysis method and ethnicity. All statistical analyses were calculated on Stata 12.0 (STATA Corporation, College Station, TX, USA).
Results
Studies characteristics
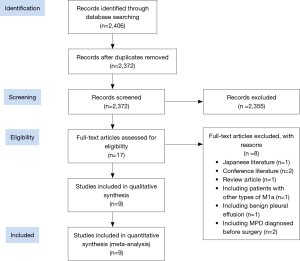
There were mostly 2,406 citations from the PubMed, Embase and Web of Science. The majority of the articles were excluded after screening the titles and abstracts. Seventeen papers in total were left, the full texts of which were further studied in detail. Finally, nine papers met the inclusion and exclusion criteria and were included in the present study (Figure 1). All of the nine included original articles published between 2001 and 2015 were retrospective analyses. Eight researches studied on Asian and five of them came from Japanese research institutions. Only one research from Georges Pompidou European Hospital and Cedre Surgical Center was about Caucasian. Further information of the studies is shown in Table 1.
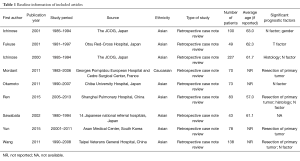
Full table
Pooled results
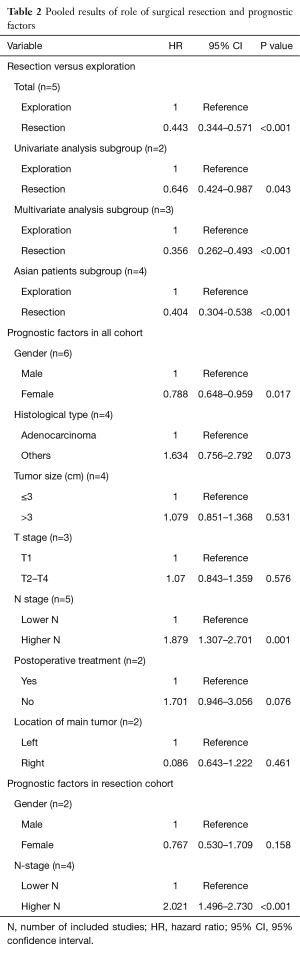
Five studies with totally 376 patients performed the comparison of resection group with exploration group. When compared to exploration group, resection of primary tumor was significantly associated with better survival (HR =0.443; 95% CI: 0.344–0.571; P<0.001) (Figure 2).
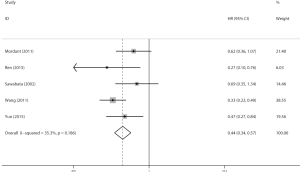
In subgroup analysis, the survival benefit of primary tumor resection was proved by both univariate and multivariate analysis, especially multivariate analysis (HR =0.359; 95% CI: 0.262–0.493; P<0.001). In addition, when stratified by ethnicity, resection group showed an advantage over exploration group on overall survival among Asian (HR =0.404; 95% CI: 0.304–0.538; P<0.001) (Table 2). The detailed extracted data were presented in Table 3.
Full table
Full table
As for other prognostic factors for NSCLC patients with MPD first found during operation (all cohort), female (HR =0.788; 95% CI: 0.648–0.959; P=0.017) and higher N stage (HR =1.879; 95% CI: 1.307–2.701; P=0.001) (Figure 3) were significantly associated with survival. However, we did not indicate any association between survival and histological type, size of primary tumor, T stage, postoperative treatment and location of primary tumor (Table 2).
Besides, we further investigated the prognostic factors for NSCLC patients with MPD first found during operation which performed primary tumor resection (resection cohort) (Table 4). Higher N-stage suggested poorer survival after primary tumor resection (HR =2.021; 95% CI: 1.496–2.730; P<0.001) (Figure 3) while no statistical difference was detected between male and female patients (HR =0.767; 95%: 0.530–1.709; P=0.158) (Table 2).
Full table
Discussion
We did the present systemic review and meta-analysis to evaluate whether surgical resection of primary tumor was beneficial to NSCLC patients with MPD that were first detected during operation, as well as other factors which affected prognosis. After statistical analysis, we found that surgical removal of primary tumor had a lower risk of death compared to exploration only among these participants with the HR of 0.443 according to meta-analysis.
Moreover, as reported by Ichinose et al. (14), the HR (95% CI) on N1–3 versus N0 was 0.541 (0.343–0.853; P=0.008), which demonstrated that no lymph node metastases was a beneficial prognostic factor. While based on studies of Wang et al. (15) as well as Iida et al. (16), MPD patients without mediastinal nodal metastases had a better survival. In this meta-analysis, we got an outcome that higher N-stage suffered a higher risk in NSCLC patients with MPD first detected during surgery. More importantly, we achieved the same conclusion in the resection group.
With rapid development in diagnostic imaging techniques, such as brain magnetic resonance imaging (MRI), computed tomography (CT), bone scan and especially application for positron emission tomography-CT (PET-CT), it became more effective and accurate to detect malignant pleural disease preoperatively (17). Therefore, patients from recent studies were likely to be at better condition than previous ones, who might have less MPE or/and less pleural disseminations. On the other hand, patients in 1980s or 1990s probably be misdiagnosed as without MPD before surgery because of lack of imaging protocols (18).
Meanwhile, it has changed constantly both in therapeutic management and operative procedures of NSCLC. More than decade ago, thoracic surgeon undertaken thoracotomy including lobectomy, pneumonectomy and pleuropneumonectomy on MPD patients, while limited resection was barely adopted. Reyes et al. reported profitable results of pleuropneumonectomy in ten patients with MPE diagnosed initially for the first time in 1991 (19). Even if Sugarbaker et al. (20) proved that pleuropneumonectomy to be a safe choice for cancers involves an ipsilateral pleura, it was still relevant to a perioperative mortality of 4.6%. Until the first application of video-assisted thoracic surgery (VATS) lobectomy in early 1990s (21,22), more and more evidence demonstrated that VATS lobectomy might be an alternative approach, which concerning with less intraoperative bleeding, less trauma, reduced postoperative pain, shorter hospitalization days (23-29), and these aspects all improved survival indirectly. Consequently, the survival outcomes of VATS were still to be explored. In addition, Ichinose and his colleagues (30) did another study in 2000 and gathered data on 227 MPD patients treated surgically from 21 institutions registered in the Japan Clinical Oncology Group (the JCOG), and they suggested that no macroscopic residual tumors were prognostic factors for better outcomes. However, since there was few data about it, we didn’t get any conclusion about the optimal surgical approach and excision range in the meta-analysis.
On the other hand, Go et al. found that postoperative chemotherapy might improve prognosis (31), but the present study indicated no statistical significance of it. The possible reason might be insufficient data. And as different chemotherapy regimens were applied in the various studies with different results, further researches might be needed to clarify the association between different chemotherapy regimens and survival of MPD unexpectedly found during surgery. Besides, since the sensibility of tyrosine kinase inhibitors (TKIs) to epithelial growth factor receptor (EGFR) mutations was discovered, the clinical strategies of NSCLC have changed a lot (32-34). It is an independent predictor of overall survival and progression-free survival in patients with NSCLC with EGFR mutations who are treated with TKIs (32).
Furthermore, Kim and his colleagues showed a longer MST in MPD patients if no pleural effusion was found (38 vs. 13 months; P<0.001) (35). However, Okamoto et al. considered that there was no benefit in MPE patients without nodules compared to MPN patients with or without effusion (11). Moreover, a review from Fiorelli A and Santini M in 2013 considered that there was no evidence strong enough to support surgery over conservative therapy in lung cancer patients with MPE found at operation (36). As mentioned above, the grouping situation of MPD was different in various studies, it was hard for us to draw a unified conclusion that what kind of MPD suffered a higher risk and in what situation should surgical treatment be contraindicated. So it could be an issue in future research.
Our study also had some limitations. It should be mentioned that there were no randomized controlled trials in our study, and all articles included in were retrospective studies. Thus, because of the distinct inclusion and exclusion criteria of variant original studies, there were possibly some selection biases. The long periods of follow-up were different among included studies and some follow-up data were derived from description of patient, and it probably led to information bias. All these bias may cause deviation to the results. As described before, Asian were put as the object of study in 8 of 9 researches, so the outcomes of our meta-analysis might be more applied to Asians. In addition, we put forward a general conception of lower N-stage and higher N-stage, which was a relative conception like N0 versus N1/2 or N0/1 versus N2. Still more prospective analysis should be done to discuss the relationship between N-staging and survival in resected NSCLC patients with no evidence of MPD preoperatively.
Conclusions
The present systemic review and meta-analysis showed that surgical resection of primary tumor was appropriate for NSCLC patients with malignant pleural disease first detected during surgery. Among this group of patients, female and lower N-stage were independent favorable prognostic factors. And for patients who were treated surgically, lower N-stage also showed a better survival.
Acknowledgements
Funding: This work was supported by the Key Science and Technology Program of Sichuan Province, China (Grant number 2013SZ0005, 2014SZ0148 to Dr. Lunxu Liu).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Sugiura S, Ando Y, Minami H, et al. Prognostic value of pleural effusion in patients with non-small cell lung cancer. Clin Cancer Res 1997;3:47-50. [PubMed]
- Goldstraw P, Crowley J, Chansky K, et al. The IASLC Lung Cancer Staging Project: proposals for the revision of the TNM stage groupings in the forthcoming (seventh) edition of the TNM Classification of malignant tumours. J Thorac Oncol 2007;2:706-14. [Crossref] [PubMed]
- Jett JR, Scott WJ, Rivera MP, et al. Guidelines on treatment of stage IIIB non-small cell lung cancer. Chest 2003;123:221S-225S. [Crossref] [PubMed]
- Postmus PE, Brambilla E, Chansky K, et al. The IASLC Lung Cancer Staging Project: proposals for revision of the M descriptors in the forthcoming (seventh) edition of the TNM classification of lung cancer. J Thorac Oncol 2007;2:686-93. [Crossref] [PubMed]
- Webber C, Gospodarowicz M, Sobin LH, et al. Improving the TNM classification: findings from a 10-year continuous literature review. Int J Cancer 2014;135:371-8. [Crossref] [PubMed]
- Pfister DG, Johnson DH, Azzoli CG, et al. American Society of Clinical Oncology treatment of unresectable non-small-cell lung cancer guideline: update 2003. J Clin Oncol 2004;22:330-53. Akulian J, Feller-Kopman D. The past, current and future of diagnosis and management of pleural disease. J Thorac Dis 2015;7:S329-38. [PubMed]
- Akulian J, Feller-Kopman D. The past, current and future of diagnosis and management of pleural disease. J Thorac Dis 2015;7:S329-38. [PubMed]
- Shimizu J, Oda M, Morita K, et al. Comparison of pleuropneumonectomy and limited surgery for lung cancer with pleural dissemination. J Surg Oncol 1996;61:1-6. [Crossref] [PubMed]
- Sawabata N, Matsumura A, Motohiro A, et al. Malignant minor pleural effusion detected on thoracotomy for patients with non-small cell lung cancer: is tumor resection beneficial for prognosis? Ann Thorac Surg 2002;73:412-5. [Crossref] [PubMed]
- Yun JK, Kim MA, Choi CM, et al. Surgical Outcomes after Pulmonary Resection for Non-Small Cell Lung Cancer with Localized Pleural Seeding First Detected during Surgery. Thorac Cardiovasc Surg 2015. [Epub ahead of print]. [Crossref] [PubMed]
- Okamoto T, Iwata T, Mizobuchi T, et al. Pulmonary resection for lung cancer with malignant pleural disease first detected at thoracotomy. Eur J Cardiothorac Surg 2012;41:25-30. [PubMed]
- Ren YJ, She YL, Dai CY, et al. Primary tumour resection showed survival benefits for non-small-cell lung cancers with unexpected malignant pleural dissemination. Interact Cardiovasc Thorac Surg 2016;22:321-6. [Crossref] [PubMed]
- Parmar MK, Torri V, Stewart L. Extracting summary statistics to perform meta-analyses of the published literature for survival endpoints. Stat Med 1998;17:2815-34. [Crossref] [PubMed]
- Ichinose Y, Tsuchiya R, Koike T, et al. Prognosis of resected non-small cell lung cancer patients with carcinomatous pleuritis of minimal disease. Lung Cancer 2001;32:55-60. [Crossref] [PubMed]
- Wang BY, Wu YC, Hung JJ, et al. Prognosis of non-small-cell lung cancer with unexpected pleural spread at thoracotomy. J Surg Res 2011;169:e1-5. [Crossref] [PubMed]
- Iida T, Shiba M, Yoshino I, et al. Surgical Intervention for Non-Small-Cell Lung Cancer Patients with Pleural Carcinomatosis: Results From the Japanese Lung Cancer Registry in 2004. J Thorac Oncol 2015;10:1076-82. [Crossref] [PubMed]
- Akaogi E, Mitsui K, Onizuka M, et al. Pleural dissemination in non-small cell lung cancer: results of radiological evaluation and surgical treatment. J Surg Oncol 1994;57:33-9. [Crossref] [PubMed]
- Rami-Porta R, Crowley JJ, Goldstraw P. The revised TNM staging system for lung cancer. Ann Thorac Cardiovasc Surg 2009;15:4-9. [PubMed]
- Reyes L, Parvez Z, Regal AM, et al. Neoadjuvant chemotherapy and operations in the treatment of lung cancer with pleural effusion. J Thorac Cardiovasc Surg 1991;101:946-7. [PubMed]
- Sugarbaker DJ, Tilleman TR, Swanson SJ, et al. The role of extrapleural pneumonectomy in the management of pleural cancers. J Clin Oncol;2009:27:abstr 7577.
- Walker WS, Carnochan FM, Pugh GC. Thoracoscopic pulmonary lobectomy. Early operative experience and preliminary clinical results. J Thorac Cardiovasc Surg 1993;106:1111-7. [PubMed]
- Kirby TJ, Mack MJ, Landreneau RJ, et al. Initial experience with video-assisted thoracoscopic lobectomy. Ann Thorac Surg 1993;56:1248-52; discussion 1252-3. [Crossref] [PubMed]
- Onaitis MW, Petersen RP, Balderson SS, et al. Thoracoscopic lobectomy is a safe and versatile procedure: experience with 500 consecutive patients. Ann Surg 2006;244:420-5. [PubMed]
- McKenna RJ Jr, Houck W, Fuller CB. Video-assisted thoracic surgery lobectomy: experience with 1,100 cases. Ann Thorac Surg 2006;81:421-5; discussion 425-6. [Crossref] [PubMed]
- Yan TD, Black D, Bannon PG, et al. Systematic review and meta-analysis of randomized and nonrandomized trials on safety and efficacy of video-assisted thoracic surgery lobectomy for early-stage non-small-cell lung cancer. J Clin Oncol 2009;27:2553-62. [Crossref] [PubMed]
- Cao C, Manganas C, Ang SC, et al. A meta-analysis of unmatched and matched patients comparing video-assisted thoracoscopic lobectomy and conventional open lobectomy. Ann Cardiothorac Surg 2012;1:16-23. [PubMed]
- Chen FF, Zhang D, Wang YL, et al. Video-assisted thoracoscopic surgery lobectomy versus open lobectomy in patients with clinical stage I non-small cell lung cancer: a meta-analysis. Eur J Surg Oncol 2013;39:957-63. [Crossref] [PubMed]
- Taioli E, Lee DS, Lesser M, et al. Long-term survival in video-assisted thoracoscopic lobectomy vs open lobectomy in lung-cancer patients: a meta-analysis. Eur J Cardiothorac Surg 2013;44:591-7. [Crossref] [PubMed]
- Park BJ, Yang HX, Woo KM, et al. Minimally invasive (robotic assisted thoracic surgery and video-assisted thoracic surgery) lobectomy for the treatment of locally advanced non-small cell lung cancer. J Thorac Dis 2016;8:S406-13. [Crossref] [PubMed]
- Ichinose Y, Tsuchiya R, Koike T, et al. The prognosis of patients with non-small cell lung cancer found to have carcinomatous pleuritis at thoracotomy. Surg Today 2000;30:1062-6. [Crossref] [PubMed]
- Go T, Misaki N, Matsuura N, et al. Role of surgery in multi-modality treatment for carcinomatous pleuritis in patients with non-small cell lung cancer. Surg Today 2015;45:197-202. [Crossref] [PubMed]
- Lynch TJ, Bell DW, Sordella R, et al. Activating mutations in the epidermal growth factor receptor underlying responsiveness of non-small-cell lung cancer to gefitinib. N Engl J Med 2004;350:2129-39. [Crossref] [PubMed]
- Paez JG, Jänne PA, Lee JC, et al. EGFR mutations in lung cancer: correlation with clinical response to gefitinib therapy. Science 2004;304:1497-500. [Crossref] [PubMed]
- Pao W, Miller V, Zakowski M, et al. EGF receptor gene mutations are common in lung cancers from "never smokers" and are associated with sensitivity of tumors to gefitinib and erlotinib. Proc Natl Acad Sci U S A 2004;101:13306-11. [Crossref] [PubMed]
- Kim YK, Lee HY, Lee KS, et al. Dry pleural dissemination in non-small cell lung cancer: prognostic and diagnostic implications. Radiology 2011;260:568-74. [Crossref] [PubMed]
- Fiorelli A, Santini M. In lung cancer patients where a malignant pleural effusion is found at operation could resection ever still be justified? Interact Cardiovasc Thorac Surg 2013;17:407-12. [Crossref] [PubMed]


