Vanishing lung mass in a patient with asthma
Introduction
Hypersensitivity to the fungus, Aspergillus fumigatus is the underlying pathogenic mechanism leading to Allergic bronchopulmonary aspergillosis (ABPA). The usual presentation is history of long standing asthma, fleeting pulmonary opacities and bronchiectasis. The estimated prevalence of ABPA is about 1% to 2% in patients with bronchial asthma and 2% to 15% in patients with cystic fibrosis (1).
The most commonly used criteria for diagnosis of ABPA are the Rosenberg-Patterson criteria (2-4) and include 8 major and 3 minor criteria. The major criteria can be remembered by the mnemonic ARTEPICS (4). These include asthma, roentgenographic evidence of fleeting pulmonary opacities, skin test positive for aspergillus (Type 1 reaction), eosinophilia, precipitating antibodies (IgG) against aspergillus in the serum, elevated serum IgE levels (>1,000 IU/mL), central bronchiectasis and elevated serum Aspergillus fumigatus - specific IgG and IgE. The minor criteria include presence of Aspergillus in sputum, expectoration of brownish black mucus plugs and delayed skin reaction to Aspergillus antigen (type III reaction).
If 6 out of the 8 major criteria are met, the diagnosis of ABPA is almost certain. Based on radiological findings, the disease is classified as ABPA-S (serologic) or ABPA-CB (central bronchiectasis) respectively depending on the absence or presence of bronchiectasis or as ABPA-S (mild), ABPA-CB (moderate), and ABPA-CB-ORF (other radiologic findings) (4).
The radiologic manifestations of ABPA are protean. The common radiographic findings include lobar or segmental collapse, focal areas of consolidation, finger in glove opacities representing mucoid impaction and bronchiectasis (4). Pulmonary masses are very uncommonly reported. We hereby report a case of ABPA presenting with a symptomatic lung mass which was successfully managed with conservative medical treatment. We also perform a review of all the cases of ABPA presenting as a lung mass, reported previously.
Case report
A 51 year old, never smoker female patient presented with progressively worsening dry cough and shortness of breath of 20 days duration. The patient also complained of dull aching left lower chest pain. There was history of streaky hemoptysis for the last three months and low grade fever for 15 days. There was history of seasonal exacerbations of cough associated with wheezing since the last 20 years. There was no history of expectoration of brownish black mucus plugs or loss of weight or appetite.
On general physical examination, the patient had respiratory rate of 16/min without any use of accessory muscles of respiration. Breath sounds were reduced in intensity over the left infrascapular and axillary areas. Expiratory polyphonic rhonchi were audible over bilateral lung fields. Examination of rest of the organ systems was normal.
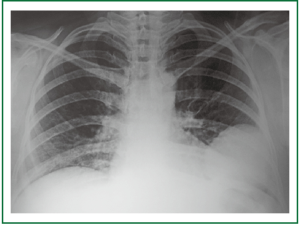
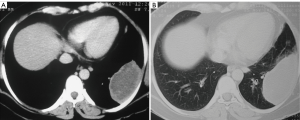
Chest radiograph showed a large well defined rounded mass like opacity in the left lower zone (Figure 1). In addition a cystic lucency was visible in the left perihilar area. Computed tomographic (CT) examination of the thorax was performed on which the mediastinal window sections demonstrated a large (7.5 cm × 3.5 cm) peripherally situated pleural based mass in the left lower lobe (Figure 2A). The mass had thick peripheral walls and large areas of central necrosis. Medially, the lesion was seen to be reaching up to the hilum of the left lung. Lung window sections demonstrated focal areas of bronchiectasis adjacent to the mass (Figure 2B).
In view of the presence of a large left lower lobe mass lesion, hemoptysis, chest pain and recent worsening of symptoms, a possibility of bronchogenic carcinoma was considered and CT guided fine needle aspiration cytology (FNAC) procedure was planned. However, in view of the presence of history of long standing asthma, fleeting radiological opacities and presence of bronchiectasis, investigations were also requested for underlying ABPA. Serum IgE levels were found to be markedly elevated 8,434 IU/mL) and markedly elevated titres of Aspergillus fumigatus specific IgE (Patient’s value 73.3 kUA/L - Normal value <0.1 kUA/L) were present. Absolute eosinophil count was elevated (600 cells/mm3). Spirometry demonstrated a mild obstructive defect. Flexible bronchoscopic examination revealed normal bronchial anatomy with no endobronchial obstruction.
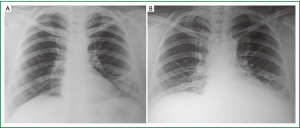
With these considerations, a diagnosis of ABPA- CB (Allergic bronchopulmonary aspergillosis - central bronchiectasis) was made and it was decided not to undertake the FNAC procedure. The patient was started on treatment with Prednisolone and Itraconazole. A chest radiograph obtained one month later demonstrated significant resolution of the left lower lobe mass lesion (Figure 3A). Itraconazole was discontinued at 2 months. Radiograph obtained four months later demonstrated complete disappearance of the mass and a thin walled cystic lucency was seen on the corresponding site (Figure 3B). The patient was completely asymptomatic at the fourth month follow up. Prednisolone was subsequently tapered off over the next one month. The serum IgE level reduced on follow up and the patient was advised to follow up with serum IgE levels and chest radiograph at six weekly intervals.
Discussion
Involvement of the respiratory system with Aspergillus can be broadly classified into three main types. These include saprophytic (aspergilloma), allergic [allergic aspergillus sinusitis, allergic bronchopulmonary aspergillosis (ABPA), and hypersensitivity pneumonitis] and invasive (airway invasive aspergillosis, chronic necrotizing pulmonary aspergillosis, and invasive aspergillosis) (4).
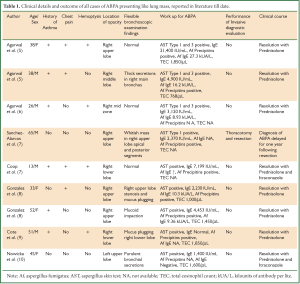
Patients with ABPA can have diverse radiological manifestations. Presence of pulmonary masses is an uncommon radiological manifestation. To the best of our knowledge, 9 cases of ABPA presenting as a lung mass have been previously reported. Although it appears coincidental, in 8 out of the 9 cases the mass was right sided. In 6 out of the 9 cases, flexible bronchoscopic examination demonstrated the presence of mucoid secretions in the bronchial segments corresponding to the mass lesion.
The clinical characteristics of ABPA patients presenting with lung mass, reported previously are described in Table 1.
Full table
It is important to note that ABPA can very well be diagnosed in patients without history of asthma. Out of the previously reported 9 cases of lung masses in patient with ABPA, 3 patients had no preceding history of asthma. This is particularly important because in these patients, presence of a lung mass can lead to strong consideration of lung cancer as a diagnostic possibility and lead to invasive diagnostic procedures to establish an accurate diagnosis. Sanchez-Alarcos et al. (6) reported a 65 year old male smoker patient without any history of asthma, who underwent right upper lobectomy due to the presence of radiological appearance of a lung mass. Even though, histopathological examination of the excised tissue demonstrated bronchial dilatations and mucoid obstruction with eosinophilic inflammation, the diagnosis of ABPA was delayed for one year following surgery.
Cope et al. highlighted that whenever a possible diagnosis of invasive aspergillosis is considered in an immunocompetent patient with asthma, ABPA should be considered as the first possibility and managed accordingly prior to instituting aggressive clinical management on the lines of invasive aspergillosis (7).
The various mechanisms described responsible for the imaging manifestation of lung masses in ABPA include- bronchial plugging with mucus leading to distal accumulation of secretions (5,6,8,9), presence of large non obstructed bronchoceles (mucus-filled dilated bronchi) (5,7) and probable inflammatory eosinophilic organizing pneumonia leading to pseudotumor like appearance (5).
The mechanism responsible for the presence of lung mass in our patient is the presence of a large reversible non obstructed bronchocele. Presence of reversible bronchoceles has been described as an almost pathognomonic feature of ABPA (11). We performed a flexible bronchoscopic examination which showed normal bronchial anatomy without any evidence of bronchial obstruction. The appearance of a large cystic lucency in the corresponding area after the resolution of the opacity confirms the same.
Although the presence of high attenuation mucus (HAM) has been described as a specific CT feature in ABPA (4), the same was not present in our patient. In fact the central contents of the mass appeared as low attenuation, like a necrotic centre. It is important to note that the appearance of high attenuation mucus is due to the presence of calcium salts and indicates long standing mucus accumulation (5). In our patient, the quick disappearance of the mass after initiation of treatment indicates an acute event which dramatically responded to treatment. Our patient had an excellent response to treatment with Prednisolone and Itraconazole, as has been described with previously reported cases.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Greenberger PA. Clinical aspects of allergic bronchopulmonary aspergillosis. Front Biosci 2003;8:s119-27.
- Rosenberg M, Patterson R, Mintzer R, et al. Clinical and immunologic criteria for the diagnosis of allergic bronchopulmonary aspergillosis. Ann Intern Med 1977;86:405-14.
- Patterson R, Greenberger PA, Halwig JM, et al. Allergic bronchopulmonary aspergillosis. Natural history and classification of early disease by serologic and roentgenographic studies. Arch Intern Med 1986;146:916-8.
- Agarwal R. Allergic bronchopulmonary aspergillosis. Chest 2009;135:805-26.
- Agarwal R, Srinivas R, Agarwal AN, et al. Pulmonary masses in allergic bronchopulmonary aspergillosis: mechanistic explanations. Respir Care 2008;53:1744-8.
- Sánchez-Alarcos JM, Martínez-Cruz R, Ortega L, et al. ABPA mimicking bronchogenic cancer. Allergy 2001;56:80-1.
- Coop C, England RW, Quinn JM. Allergic bronchopulmonary aspergillosis masquerading as invasive pulmonary aspergillosis. Allergy Asthma Proc 2004;25:263-6.
- Otero González I, Montero Martínez C, Blanco Aparicio M, et al. Pseudotumoral allergic bronchopulmonary aspergillosis. Arch Bronconeumol 2000;36:351-3.
- Cote CG, Cicchelli R, Hassoun PM. Hemoptysis and a lung mass in a 51-year-old patient with asthma. Chest 1998;114:1465-8.
- Nowicka U, Wiatr E, Jakubowska L, et al. Allergic bronchopulmonary aspergillosis mimicking lung cancer in patients without bronchial asthma--case report. Pneumonol Alergol Pol 2012;80:77-81.
- Lemire P, Trepanier A, Hebert G. Bronchocele and blocked bronchiectasis. Am J Roentgenol Radium Ther Nucl Med 1970;110:687-93.


