Surgical treatment of active infective endocarditis: A single center experience
Resident Internal Medicine, Jersey City Medical Center, NJ, USA
|
Original Article
Surgical treatment of active infective endocarditis: A single center experience
Resident Internal Medicine, Jersey City Medical Center, NJ, USA
|
|
Abstract
Objective: This study was undertaken to examine the outcomes of surgery for active infective endocarditis.
Methods: Fifty consecutive patients underwent surgery for active infective endocarditis in a tertiary care center between January 2000 and June 2003. Modified Duke Criteria was used to include the patients in the study.
Results: Mean age of the patients was 55.72 years (range 18-89 years). Underlying heart disease was the most common cause of acute infection, accounting for 30 % of all the cases. 16 % patients had a recent dental procedure and 10 % had a recent surgical procedure. The most common infective organism was staphylococcus aureus (24%), followed by streptococcus viridians (20%). The most common indications for surgery were congestive heart failure (CHF) (52%), embolic phenomenon (18%) and septic shock (10%). Most common postoperative complication was respiratory failure (30%) followed by renal failure (24%) pacemaker implantation 22%; stroke 18%, bleeding 16% and GI bleeding 2 %. Seven out of 50 patients died during hospital course that accounts for 14% of the motility rate.
Conclusion: Surgery for endocarditis continues to be challenging and associated with high operative mortality and morbidity. Age, shock, prosthetic valve endocarditis, impaired ventricular function, and recurrent infections adversely affect long-term survival.
Key words
active infective endocarditis; surgery
J Thorac Dis 2010;2:129-133. DOI: 10.3978/j.issn.2072-1439.2010.02.03.3
|
|
Introduction
Appropriate antibiotic therapy is the most important component
in the treatment of patients with infective endocarditis
(1). Depending on how promptly the disease is diagnosed
and appropriate antibiotics are started, the virulence of the
microorganism, and whether the infected valve is native or
prosthetic, surgery may become indispensable to save the patient’
s life and eradicate the infection. Timing of surgery is crucial
for patients for whom medical therapy fails. Delaying surgical
treatment often increases the probability of complications and
also operative mortality and morbidity. The notion that less
virulent microorganisms, such as Streptococcus viridans, always
respond to antibiotics alone is erroneous, because these bacteria can cause extensive damage to a heart valve and surrounding
tissues if inadequately treated (2). Certain cases of infective
endocarditis are deemed inoperable because of multiorgan
failure or extensive cerebral damage from septic emboli, and
these patients die of the disease. This study is a retrospective
review of a single center experience with surgery for active
infective endocarditis.
|
|
Methods
Between January 2000 and June 2003, 50 patients underwent
surgery for native valve infective endocarditis in a tertiary care
medical center. Modified Duke’s clinical Criteria were used to
include the patients in this study.
All Patients were diagnosed with native valve endocarditis
based on clinical findings, blood cultures, echocardiography,
cultures and intraoperative findings. No case of Prosthetic valve
endocarditis was included.
Preexisting conditions including congenital heart disease
(bicuspid aortic valve, Coactation of aorta, ventricular septal
defect) and acquired heart disease (rheumatic heart disease),
as well as previous invasive procedures including dental,
gynecological etc were taken in to account as potential causes of
increased susceptibility in patients.
|
|
Results
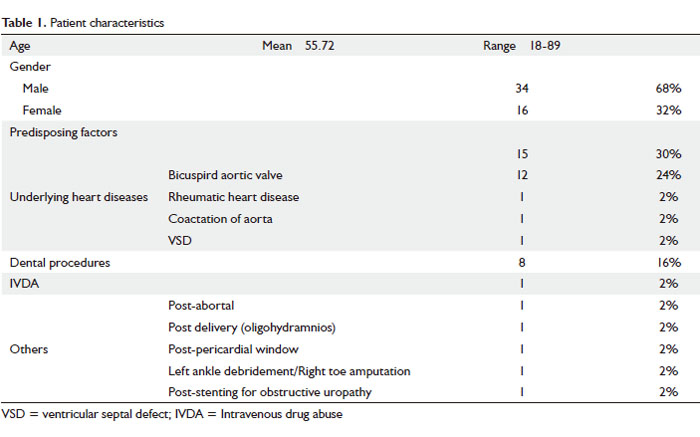
Mean age of the patients was 55.72 years (range 18-89 years).
68 % of the patients were male and 32 % were female. Statistical
analysis of the risk factors revealed that underlying heart disease
was the most common cause of acute infection, accounting for
30 % of all the cases. 16 % patients had a recent dental procedure
and 10 % had a recent surgical procedure.
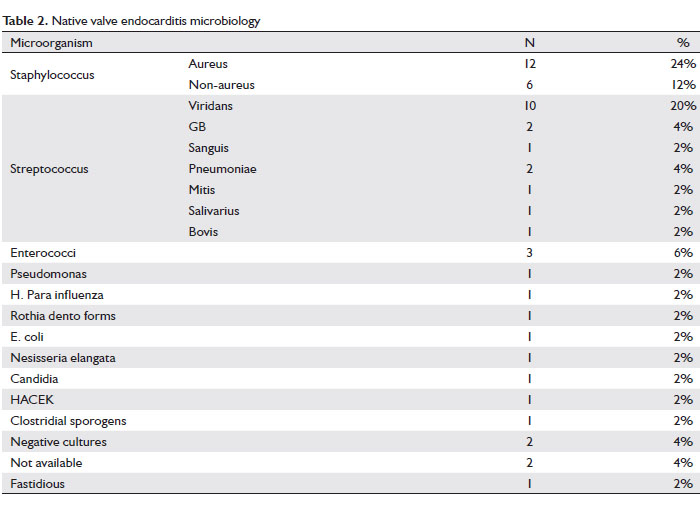
Microorganisms
Table 3 shows the incidence of all infective organisms. The
most common infective organism was staphylococcus aureus
(24%), followed by streptococcus viridians (20%). 1 patient
grew HACEK organism. Negative cultures were found in 4%
patients.
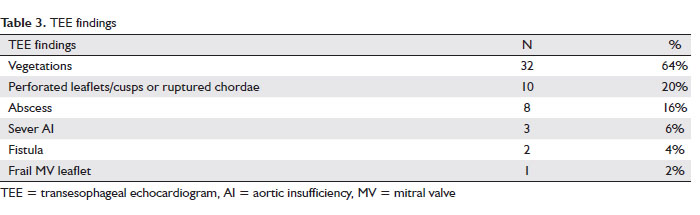
Trans-esophageal echocardiogram (TEE)
TEE revealed the presence of vegetations in 32 patients (64%),
perforated leaflet or ruptured in chorda tendinae in 10 patients
(20%) and an abscess in 8 patients (16%).
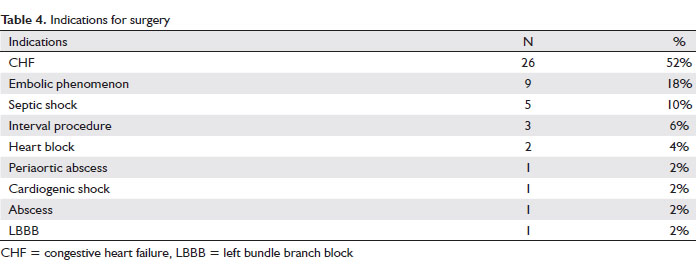
Indication for surgery
The most common indications for surgery were congestive heart
failure (CHF) (52%), embolic phenomenon (18%) and septic
shock (10%). The other indications for surgery were interval
procedure (6%), heart block (4%), para-aortic abscess (2%),
cardiogenic shock (25), abscess (2%), LBBB (2%) and past history of endocarditis (2%).
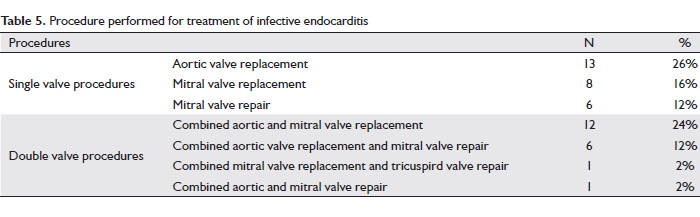
Surgical procedures performed
Table 5 shows surgical procedures performed. The surgical
procedures performed include both single valve and double
valve operations. Single valve procedures included MVr 12%,
MVR 16%, AVR 30%, MV debridment only 2% and concomitant
CABG in 20% of the patients. Double valve operations included
AVR/MVR 24%, AVR/MVr 12%, AVr/MVr 2%, MVR/TVr 2 %
and with commitment CABG in 0%.
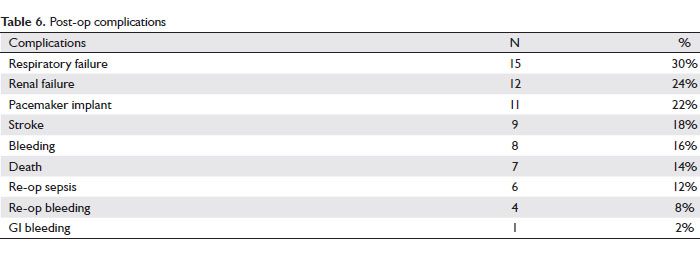
Postoperative complications
Table 6 shows postoperative complications. Most common
postoperative complication was respiratory failure (30 %)
followed by renal failure (24%) pacemaker implantation 22%;
stroke 18%, bleeding 16% and GI bleeding 2 %. 4 patients (20
%) underwent re-operation including 12 % for sepsis and 8 % for
bleeding. Seven out of 50 patients died during hospital course
that accounts for 14% of the motility rate.
      |
|
Discussion
This report describes outcomes of surgery for active infective
endocarditis in a cohort of patients during a three-year interval.
Although, we are aware of a few patients with disease deemed
inoperable during this period, their number was very small.
The operative mortality and morbidity in this report probably reflect an accurate risk of surgery in patients with active infective
endocarditis in a large tertiary care hospital.
Although cardiac surgery is necessary in less than a third
of patients who have infective endocarditis of native valves
and fewer than half of those with prosthetic valves (3-6), a
multidisciplinary approach is necessary to treat these patients
and must involve at least specialists in infectious disease,
cardiology, and cardiac surgery (7). The indications for and
timing of surgery are still controversial among internists who
treat these patients, and the input of a cardiac surgeon is needed
if mortality and morbidity are to be reduced (7, 8). Close
surveillance of these patients is indispensable to detect early
failure of adequate antibiotic therapy to avoid Cardiogenic or
septic shock and multi-organ failure.
It has been shown that cases of endocarditis caused by S
aureus and other virulent microorganisms on valves in the
left side of the heart are best treated with early surgery. In a
large merged database on native valve endocarditis, the overall
mortality was higher among patients with S aureus endocarditis
than among those with other bacteria (20% vs 12%, P <0.001);
surprisingly, however, fewer patients infected with S aureus
had surgery (26% vs. 39%, P <0.001). S aureus emerged as an
independent predictor of operative mortality in many surgical
series.
The outcomes of prosthetic valve endocarditis are worse than those of native valve endocarditis. We found that not
only was prosthetic valve endocarditis associated with higher
operative mortality, but also it adversely affected long-term
survival relative to native valve endocarditis. In a report from
the United Kingdom Heart Valve Registry on 322 cases of
prosthetic valve endocarditis, the 30-day mortality was 20% and
the 5- and 10-year survivals were 55% and 37%, respectively (9).
Investigators from the Cleveland Clinic reported an operative
mortality of 13% among 146 patients with prosthetic valve
endocarditis; among those who survived surgery, the 5-year
survival was 82% and the freedom from reoperation was 75%
(10). In another report from the same institution on prosthetic
aortic valve endocarditis treated exclusively with aortic valve
homograft, the operative mortality was only 3.9% and the 5- and
10-year survivals were 73% and 56%, respectively.
The main reason the operative mortality for prosthetic valve
endocarditis is higher than that for native valve endocarditis is the
complexity of the operation and the fact that it is often associated
with para-valvular abscess. Resection of aortic root abscess is
indeed a complex operation, but resection of mitral annulus
abscess can be even worse. Although aortic valve homografts
are believed to be the best valve for aortic root abscess, they are
not a substitute for radical debridement and implantation of
the new valve on healthy and strong tissues. Persistent or early
recurrent endocarditis is probably related more to the surgeon’s recognition of and ability to extirpate all infected tissues than
to the type of valve used for replacement. We believe that aortic
homograft is ideally suited for reconstruction of the aortic root,
however, because it is easier to handle than prosthetic materials
and its anterior leaflet of the mitral valve can be used to patch
defects created by the resection of the abscess.
In conclusion, surgery for active infective endocarditis
continues to be challenging and to be associated with high
operative mortality and morbidity. The long-term survival
is satisfactory, although these patients are at higher risk for
development of recurrent endocarditis than are patients who
have never had valve infection.
|
|
References
Cite this article as: Aziz F, Doddi S, Penupolu S, Dutta S, Alok A. Surgical treatment of active infective endocarditis: A single center experience. J Thorac Dis 2010;2(3):129-133. doi: 10.3978/j.issn.2072-1439.2010.02.03.3
|