|
Original Article
The application of bi-level positive airway pressure in patients with severe pneumonia and acute respiratory failure caused by influenza A (H1N1) virus
Wei Liu, Shucheng Hua, Liping Peng
The Respiration Department of the First Affiliated Hospital of Jilin University, Changchun 130021, Jilin Province, PR China
Corresponding author: Wei Liu, MD. The Respiration Department of the 1st Affiliated Hospital of Jilin University, Changchun 130021, Jilin, PR China. Tel:+86-431-88782318; Fax: +86-431-85664490. E-mail: liuwei1002@sina.com
|
|
Abstract
Objective: To evaluate the effect of noninvasive Bi-level Positive Airway Pressure (BiPAP) ventilation on the severe influenza A virus associated with pneumonia and acute respiratory failure (ARF).
Methods: Based on conventional therapy via face mask using BiPAP ventilator positive airway pressure ventilation in the treatment of severe pneumonia caused by influenza A (H1N1) virus with acute respiratory failure (ARF) in 18 cases, we observed and evaluated the therapeutic effects.
Results: PaO2 and SaO2 before and after treatment were (48.85 ± 12.15)mmHg, (68.56 ± 16.25) mmHg and (80 ± 6)%, (92 ± 5)%, respectively. The results were significantly different (P<0.05) before and after treatment. Endotracheal intubation rate was 25% (6/24) and case-fatality rate was 8.3% (2/24).
Conclusion: BiPAP ventilator airway pressure by face mask ventilation can reduce the rate of endotracheal intubation in the treatment of severe pneumonia caused by influenza A (H1N1) virus in acute respiratory failure. It could be an effective approach in the emergency treatment with clinical value.
Key words
Bi-level positive airway pressure ventilation; severe influenza A (H1N1) virus; acute respiratory failure
J Thorac Dis 2010;2:134-137. DOI: 10.3978/j.issn.2072-1439.2010.02.03.4
|
|
Introduction
Influenza A H1N1 is a new type of global infectious disease
( 1, 2). The genetic sequence of Influenza A (H1N1) virus is
different from the known human influenza virus ( 3-5). The
crowd would be generally susceptible and vulnerable to its
outbreak. Since the first case of H1N1 flu reported in Mexico ( 6),
South America in March 2009, Influenza A H1N1 had extended
rapidly to more than 30 countries and regions throughout the
world, including China, the United States ( 7, 8), Canada, Japan
( 9), and Hong Kong. Particularly in winter, the patient number
of outbreak was increasing, as well as the cases of pneumonia
caused by this virus. The major pathological features of influenza
A (H1N1) complicated with severe pneumonia are bronchial
wall necrosis, neutrophil infiltration, diffuse alveolar damage
with hyaline membrane disease, including diffused alveolar damage, bronchioles and perivascular lymphocyte infiltration,
proliferative changes in airway and bronchiolitis obliterans ( 10).
It may affect the ventilation and air exchange, and easily leads to
hypoxia. Irreversible damage to important viscera, which is fetal,
will be followed if without prompt therapy. Non-invasive ventilation (NIV) refers to various methods
of respiratory support that do not require tracheal intubation,
such as continuous positive airway pressure ventilation (CPAP)
and bi-level positive airway pressure (BiPAP). By contrast to
CPAP wherein fixed pressure support is maintained throughout
the respiratory cycle, BiPAP devices deliver bias-flow pressurecontrolled
air via a nasal, oral-nasal, or helmet mask. Bi-level
positive airway pressure is generally applied in adults with
chronic obstructive pulmonary diseases (COPD), obstructive
sleep apnea, or acute respiratory distress syndrome (ARDS)
( 11). Non-invasive ventilation was introduced for use in children
during the polio epidemic of the 1950s (the iron lung) in the
form of negative pressure ventilation ( 12). Maurizio et al repor ted that BiPAP showed up an
antiarrhythmic effect in patients with acute respiratory failure
caused by COPD in a randomized clinical trail. It was reported
that the BiPAP can affect global cardiac performance through
its effects on the determinants of cardiac function, i.e. heart rate,
preload, contractility and afterload ( 13). The routine therapies of influenza A (H1N1) include anti-virus treatment, glucocorticoids therapy, anti-infection treatment
and nutrition support therapy. The drug susceptibility can be
found in the U.S Centers of Diseases of Control and Prevention
(CDC) and Chinese Ministry of Health ( 14). In this study, we designed a new therapeutic approach by
adding the non-invasive BiPAP based on the routine therapy
strategy in 18 cases of severe influenza caused by H1N1
influenza virus pneumonia with acute respiratory failure (ARF)
in single institution, and retrospectively evaluated the effects of
this approach by lung function test, which might induce a new
therapeutic direction on this disease.
|
|
Material and method
Patient basic data
18 cases of influenza A (H1N1) complicated with severe
pneumonia in our study are diagnosed etiologically, the throat
swab specimens were detected by RT-PCR. And they were sent
to pneumology department and infectious disease department in
NO.1 Hospital of Jilin University ( Jilin, China).
Among the 18 cases, there were 10 male patients and 8
female cases, the average age was 28.73±9.24 (16 to 57), and
all got community-acquired pneumonia (CAP). 2 cases were
complicated with basic diseases (11.1%), while 1 case was with
the bronchial asthma. And there is 1 case got CAP after the
organ transplant. 2 cases were pregnant (11.1%). The BMIs in 12
of the 18 cases were all above 30 (66.7%).
Comprehensive treatment strategy
According to the standard procedure of Ministry of Health
( 14, 15), the comprehensive treatment of viral pneumonia
is adapted, including: (1) Anti-virus treatment: each of the
18 patients was given anti-virus therapy under the regimen
of Oseltamivir 75mg or 150mg , bid, for oral use; (2)
Glucocorticoids: 16 cases were treated with glucocorticoids
(88.9%) under Methylprednisolone 0.5-1mg/Kg.d and other
2 cases are not; (3) Anti-infection treatment: the routine antiinfection
drug was Carbapenems Antibiotic at the beginning,
and then was adjusted according to the patients’ condition; (4)
Nutrition support was used on all the 18 cases; (5) Mechanical
ventilation: Based on the conventional treatment above, we
applied nasal mask positive airway pressure. We chose the
appropriate masks (including closed type and nasal type)
according to the factors below: mouth coverage, secretion
amount and the surface shape&size (BIPAP Synchrony ventilator
S/T self-trigger respiratory mode, Wellkang LLC, USA).
The primary parameters setting were: respiratory frequency
was 18/min; the IPAP increased gradually from 6 cmH 2O (1
cmH 2O=0.098kPa) to 12~20 cmH 2O in 30 minutes; the EPAP
was 4 cmH 2O and the pressure range was 4 to 12 cmH 2O, which
adjusted to the IPAP synchronously with oxygen flow of 5 L/min. After 6 hours’ ventilation, we reexamined the blood and
gas, then analyzed and recorded the clinical condition. When
the worse conditions, for example, suffocating or disturbance of
consciousness, hypotension, that is systolic pressure is less than
90mmHg (1mmHg=0.133kPa), PaO 2 decreases to 40mmHg,
and arterial pH≤7.25, happened, the patient would be given
endotracheal intubation mechanical ventilation treatment. We monitored and recorded the blood and gas before the
treatment for 6 hours every 24 hours after their treatment. If
PaO 2/FiO 2>200 or increased by >100 compared to before
the treatment, it was believed that the air exchange had been
improved ( 16). If it could last until the ventilation ending, it was
believed that the air exchange improved constantly.
CT scanning
We scanned all the patients 3 days later after the therapy to
identify the change in lung parenchyma, which could further
prove the effectiveness.
Statistics processing
We analyzed the data with SPSS13.0 software. The data is
represented by -x±s, and paired t test is applied. The difference
has statistical significance if P
|
|
Results
Blood gas analysis
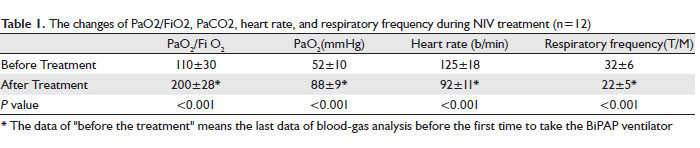
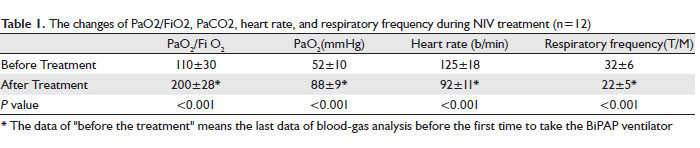
After the treatment of 18 cases, 12/18 had been statistically
improved ( Table 1). In these 12 cases, the expiratory dyspnes
had been lessened, respiratory frequency and heart rate had
been decreased, with PaO 2 and PaO 2/FiO 2 increased. The
efficiency rate was 66.7%. Endotracheal intubation was applied
in other 6 cases, among whom, 4 survived and 2 died. Ratio of
the application of endotracheal intubation was 33.3 % (6/18)
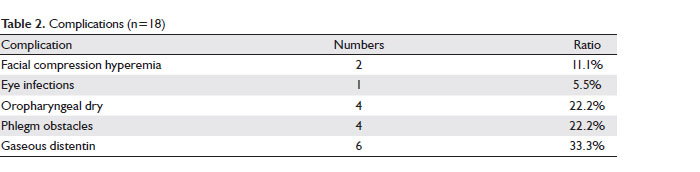
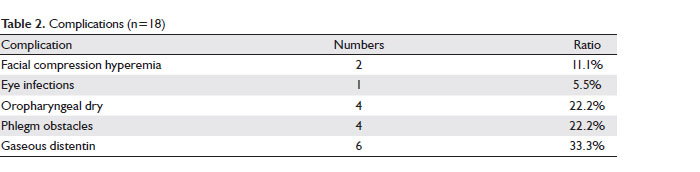
and fatality rate was 11.1% (2/18). Among the 18 cases, facial
compression hyperemia was found in 2 cases, eye infections in 1
case, oropharyngeal dry in 4, phlegm obstacles in 4 and gaseous
distention in 6 ( Table 2).
CT scanning analysis
After 3 days of therapy, we scanned the lung with Computed
Tomography (CT). We found partly absorption of consolidation
in 15 cases (83.3%), while thickening interlobular septa in 12
cases (66.7%) ( Fig 1b). After 7 days of therapy, we scanned
the lung again with CT. We found significantly absorption of
consolidation of 14 cases (77.8%), while fiber rope formation in
the disease lesion in 16 cases (88.9%) ( Fig 1c).
|
|
Discussion
Bi-level positive airway pressure ventilation (BiPAP) is a new type of respiration support mode, which has been used in ARF
caused by COPD or paediatric oncology, heart failure caused
by sleep apnea and other respiratory diseases ( 12-14). BiPAP
ventilator enables patients’ spontaneous breath by Bi-level
positive airway pressure, therefore, it has the characteristic of
spontaneous breath and breath control simultaneously. On one hand, the operating principle of BiPAP ventilator
S and S/L modes is PSV. That is because the respiratory
frequency and ventilation VT mainly depend on the patients’
self-regulation, which is closer to physiological status than other
modes ( 13). Therefore, it can lessen the influence of volume
damage on hemodynamic and the counteraction between the
ventilator and patient. On the other hand, the ventilator provides
non-invasive Bi-level positive airway pressure, so it reduces
respiratory workload and oxygen consumption, meanwhile
increases the alveolar ventilation and reopens the atelectatic lung
resulting in improving the ventilation-flow ratio ( 14). The pathological symptoms of influenza A (H1N1)
complicated by severe pneumonia are lung tissue oedema,
inflammatory exudation, partly sinking and collapsing alveolus
and lung consolidated. Hyoxemia is mainly caused by arterial and
venous blood diffluency and the imbalance of ventilation-flow ratio. The application of BiPAP ventilator can raise pulmonary
oxygen pressure by reducing the pulmonary workload and
activating the collapsing alveolus ( 17). This study illustrated that BiPAP ventilator had improved the
clinical status of the patients enrolled in the study. Respiratory
frequency and heart rate had fallen (P<0.05). PaO2 rised
(P<0.05). 66.7% of the patients didn’t experience intubation
and related complicated diseases. The costs of medical care had
decreased.
The result of this study had proved the application of BiPAP
ventilator could improve respiratory status of patients with
H1N1 influenza virus pneumonia and acute respiratory failure.
It could significantly improve arterial blood gas analysis status
of the patient without negative influence on haemodynamics.
What’s more, in the study we found that the application of
BiPAP ventilator at the early stage could reduce intubation
and related complicated diseases. That is because when acute
respiratory failure happens, the capillary alveolar membrane
permeability increases, which leads to the pulmonary edema
( 11, 14). Most patients have little purulent secretion in our study,
which provides suitable conditions for NPPV treatment. NPPV
reduces the pulmonary effusion and edema status through positive pressure, which improves oxygenation. The incidence
rate of ventilator related pneumonia and lung injury is lower than
that of invasive ventilation ( 18). Our data showed that the BiPAP
could have a significant effect on the treatment of the influenza
H1N1 virus pneumonia with acute respiratory failure patients,
especially on emergency situations. Further large samples
randomized controlled trials are needed to evaluate whether the
death rate of patients could be reduced. Nevertheless, some complications of BiPAP shown in our
study has to be noticed, such as eye and face skin damage,
oropharyngeal dry, phlegm difficulties and gaseous distention.
Based on our experience, choosing appropriate masks with better
tissue compatibility, applying humidifying device, choosing
appropriate pressure, guiding the nasal respiration and avoidance
of mouth respiration are the effective approaches to deal with
the complications. However, gaseous distention is also one of the
complications, and the gastrointestinal decompression should be
given in time.
In conclusion, BiPAP ventilator airway pressure by face mask
ventilation can reduce the rate of endotracheal intubation in the
treatment of severe pneumonia caused by influenza A (H1N1)
virus in acute respiratory failure. It could be an effective approach
in the emergency treatment and has an important application
value.
|
|
References
- Centers for Disease Control and Prevention (CDC). Update: infections with a swine-origin influenza A (H1N1) virus -United States and other countries, April 28, 2009. MMWR Morb Mortal Wkly Rep 2009;58:431-3.[LinkOut]
- Naffakh N, van der Werf SV. April 2009: an outbreak of swine-origin influenza A(H1N1) virus with evidence for human-to-human transmission. Microbes Infect 2009;11:725-8.[LinkOut]
- Novel Swine-Origin Influenza A (H1N1) Virus Investigation Team, Dawood FS, Jain S, Finelli L, Shaw MW, Lindstrom S, et al. Emergence of a novel swine-origin influenza A (H1N1) virus in humans. N Engl J Med 2009;360:2605-15.[LinkOut]
- Trifonov V, Khiabanian H, Greenbaum B, Rabadan R. The origin of the recent swine influenza A (H1N1) virus infecting humans. Euro Surveill 2009;14:19193.[LinkOut]
- Centers for Disease Control and Prevention (CDC). Update: drug susceptibility of swine-origin influenza A (H1N1) viruses, April 2009. MMWR Morb Mortal Wkly Rep 2009;58:433-5.[LinkOut]
- Centers for Disease Control and Prevention (CDC). Outbreak of swine-origin influenza A (H1N1) virus infection -Mexico, March-April 2009. MMWR Morb Mortal Wkly Rep 2009;58:467-70.[LinkOut]
- Centers for Disease Control and Prevention (CDC). Swine-origin influenza A (H1N1) virus infections in a school-New York City, April 2009. MMWR Morb Mortal Wkly Rep 2009;58:470-2.[LinkOut]
- Centers for Disease Control and Prevention (CDC). Swine influenza A (H1N1) infection in two children -Southern California March-April 2009. MMWR Morb Morta Wkly Rep 2009;58:400-2.[LinkOut]
- World Health Organization (WHO). Human infection with new influenza A (H1N1) virus: clinical observations from a school-associated outbreak in Kobe, Japan, May 2009. Wkly Epidemiol Rec 2009;84:237-44.[LinkOut]
- Gill JR, Sheng ZM, Ely SF, Guinee DG, Beasley MB, Suh J, et al. Pulmonary pathologic findings of fatal 2009 pandemic influenza A/H1N1 viral infections. Arch Pathol Lab Med 2010;134:235-43.[LinkOut]
- Schiller O, Schonfeld T, Yaniv I, Stein J, Kadmon G, Nahum E. Bi-level positive airway pressure ventilation in pediatric oncology patients with acute respiratory failure. J Intensive Care Med 24:383-8.[LinkOut]
- Aschenbrenner R, Donhardt A, Foth K. Permanent artificial respiration in the iron lung; report on experiences with 105 respirator paralyzed poliomyelitis patients from 1947 to 1952. Munch Med Wochenschr 1953;95:748-51.[LinkOut]
- Marvisi M, Brianti M, Marani G, Turrini G, Zambrelli P, Ajolfi C, et al. Acute antiarrhythmic effects of bi-level positive airway pressure ventilation in patients with acute respiratory failure caused by chronic obstructive pulmonary disease: a randomized clinical trial. Respiration 2004;71:152-8.[LinkOut]
- Centers for Disease Control and Prevention (CDC). Update: drug susceptibility of swine-origin influenza A (H1N1) viruses, April 2009. MMWR Morb Mortal Wkly Rep 2009;58:433-5.[LinkOut]
- Hui DS, Lee N, Chan PK. Clinical Management of Pandemic (H1N1) Infection. Chest 2010;137:916 -25.[LinkOut]
- Meduri GU, Turner RE, Abou-Shala N, Wunderink R, Tolley E. Noninvasive positive pressure ventilation via face mask. First-line intervention in patients with acute hypercapnic and hypoxemic respiratory failure. Chest 1996;109:179-93.[LinkOut]
- Elliott MW.Non-invasive ventilation for acute respiratory disease. British Medical Bulletin 2004;72:83-9.[LinkOut]
- Burns KE, Adhikari NK, Keenan SP, Meade M. Use of non-invasive ventilation to wean critically ill adults off invasive ventilation: meta-analysis and systematic review. BMJ 2009;338:b1574.[LinkOut]
Cite this article as: Liu W, Hua SC, Peng LP. The application of bi-level positive airway pressure in patients with severe pneumonia and acute respiratory failure caused by influenza A (H1N1) virus. J Thorac Dis 2010;2(3):134-137. doi: 10.3978/j.issn.2072-1439.2010.02.03.4
|