Association between postoperative bulla neogenesis at the staple line and resected lung weight for primary spontaneous pneumothorax: a retrospective study using the inverse-probability of treatment weighted method in patients grouped according to age
Introduction
Primary spontaneous pneumothorax (PSP) is common medical condition that is encountered in general hospitals as well as specialized institutions for PSP. However, the postoperative recurrence rate of PSP after both conservative and surgical therapies is relatively high, and current treatment outcomes are generally unsatisfactory. Patients with PSP usually have particularly demanding lifestyles, including school attendance, employment, etc. Thus, the reduction of post-therapy recurrence rate is of particular importance. For surgical treatment of PSP, bullectomy, using autosutures under video-assisted thoracoscopic surgery (VATS), is the standard procedure at present (1-6). This procedure is particularly useful, as it is both simple and safe. However, postoperative bulla neogenesis (POBN) along the staple line is relatively common and is considered a factor in promoting PSP recurrence (3,7). In a modification of the original surgical technique, the staple line is reinforced with an absorbable sheet and/or fibrin glue to prevent POBN. Several reports have demonstrated the utility of this reinforcement technique in reducing the postoperative PSP recurrence rate (4,5,7). However, the use of fibrin glue involves the risk of exposure to infectious agents (8). If the risk factor(s) for POBN could be predicted, then reinforcement with fibrin glue could be limited to those patients who have a high risk of developing POBN.
The tension at the staple line is thought to result in POBN (9), and we believed that the resected lung weight (LW) affects this tension. Therefore, we hypothesized that the tension at the staple line would increase as the weight of resected lung tissue, performed by autosutures, increases. As a result, POBN may be more likely to develop in sites involving particularly large resection. We subsequently reported the relationship between POBN and LW (10).
It has recently been reported that the postoperative recurrence rate is higher in young individuals with PSP than in the elderly (11,12). This suggests that the characteristics of POBN may also differ according to age. As our study is retrospective, patient backgrounds were heterogeneous. Therefore, we have used the inverse-probability of treatment weighted (IPTW) method in order to adjust for heterogeneous patient backgrounds and evaluated the association between POBN and LW in patients grouped according to age treated surgically for PSP. This study was approved by the Institutional Review Board of Takasago Municipal Hospital (No. 2016-1).
Methods
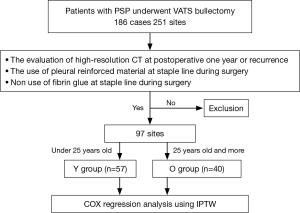
Between February 2011 and April 2016, we enrolled 178 consecutive PSP patients with 238 resected lung sites, who underwent VATS at our hospital. Only cases meeting the following criteria were evaluated: (I) staple lines were covered with an oxidized cellulose sheet without fibrin glue; (II) POBN was evaluated with high resolution computed tomography. In total, 96 sites in 67 patients were evaluated (Figure 1). Patients were subdivided into two groups according to their age for subsequent analysis: The Y group, less than 25 years old (56 sites) and the O group, aged 25 years or older (40 sites). We used the Cox regression analysis with IPTW method. In order to adjust for the different patient backgrounds, the IPTW method included the following factors: gender, smoking habit, history of previous ipsilateral operations, body mass index and resected lung sites.
Patients underwent VATS according to the following indications: ipsilateral PSP recurrence, a persistent air leakage after chest tube drainage, contralateral PSP, patient request, and tension pneumothorax. All procedures were performed by a single surgical team. The surgical protocol required that the bullae be resected with a sufficient margin and that the team was certain that no residual bullae were present around the staple line. LW was measured with a gravimeter in the operating room immediately after surgery. Chest radiography was performed in each patient every 3 months postoperatively, and the presence of POBN was investigated using 1.00–1.25 mm thickness high-resolution computed tomography 1 year postoperatively, if there was no evidence of recurrence, or sooner if dyspnea, chest pain, and others symptoms occurred. None of the patients underwent perioperative chemical pleurodesis.
Statistical analyses were performed using Student t-test, the χ2 test, Fisher’s exact test and Cox regression analysis using the IPTW method. A P value of <0.05 indicated statistical significance. The hazard ratio and 95% confidence interval were calculated for each variable.
Results
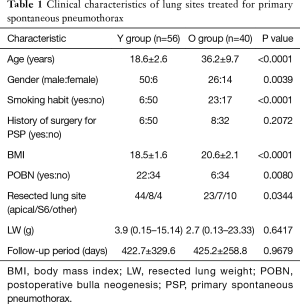
POBN was detected at 22 of 56 (39.3%) and 6 of 40 (15.0%) sites on high-resolution CT in the Y and O groups, respectively, with this difference being statistically significant (P=0.0080, Table 1). The mean age of individuals in the Y and O groups was 18.6±2.6 and 36.2±9.7 years old, respectively and this difference was statistically significant (P<0.0001, Table 1). A smoking habit was present in 6 of 56 (10.7%) and 23 of 40 (57.5%) sites, in the Y and O groups, respectively and this difference was statistically significant (P<0.0001, Table 1). Mean body mass index was 18.5±1.6 and 20.6±2.1, in the Y and O groups respectively and this difference was statistically significant (P<0.0001, Table 1). Resected sites including apical, segment six and others were 44/8/4 and 23/7/10, in the Y and O groups, respectively with this difference reaching statistical significance (P<0.0344, Table 1). The results showed that there were different backgrounds between both groups. Neither the median LW, 3.9 and 2.7 g, in the Y and O groups, respectively; nor the mean follow-up period, 422.7±329.6 and 425.2±258.8 days in the Y and O groups, respectively differed significantly between the two groups (Table 1).
Full table
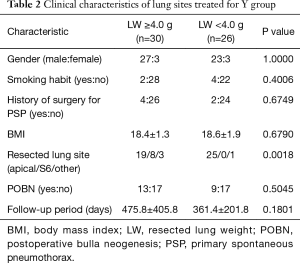
When LW cut off was set at 4.0 g, which is close to the median LW value, for patient backgrounds in the Y group, no statistically significant differences were identified by univariate analysis, except for resected sites (Table 2).
Full table
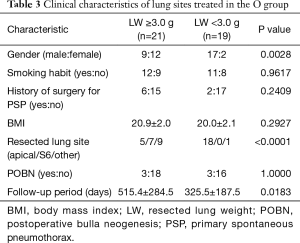
Similarly for the O group, males represented 9 of 21 (42.9%) and 17 of 19 (89.5%) sites and apical resected sites represented 5 of 21 (23.8%) and 18 of 19 (94.7%) sites for LW <3.0 g and LW ≥3.0 g, respectively and reached statistical significance (P=0.0028 and <0.0001, respectively, Table 3).
Full table
We used Cox regression analysis combined with the IPTW method to take into account various aspects of patient backgrounds including gender, smoking habit, history of operation, BMI and resected lung sites.
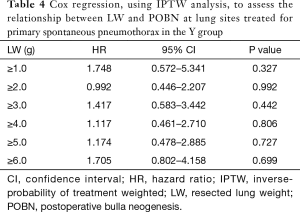
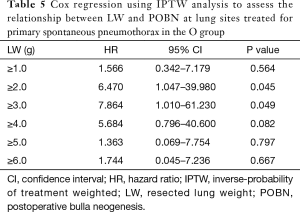
For the Y group, no LW, whose cut-off values ranged from 1.0 to 6.0 g was associated with POBN (Table 4). For the O group, LW ≥2.0 g and LW ≥3.0 g were both significantly associated with POBN (P=0.045 and 0.049, respectively, Table 5) although other LW cut-offs, ranging from 1.0 to 6.0 g, were not associated with POBN (Table 5).
Full table
Full table
Discussion
Bullectomy for PSP is routinely performed with autosutures (1-6). This procedure is performed using VATS, and its simplicity and safety make it particularly useful. However, it always results in a staple line on the visceral pleura. POBN is relatively common occurrence, and is considered a risk factor for PSP recurrence (3,7). Fibrin glue and absorbable sheet, both of which have been evaluated for use in reinforcement of the staple line, are thought to be effective in preventing POBN (7). In a study by Lee et al., it was shown that the use of fibrin glue and absorbable cellulose mesh for re-enforcement of the staple line after VATS bullectomy was comparable to mechanical pleurodesis in terms of prevention of postoperative PSP recurrence (4). Another study by Nakanishi revealed that the combined use of fibrin glue and an absorbable sheet in stapled VATS bullectomy reduced the 5-year recurrence rate of postoperative PSP (5). However, the intraoperative use of fibrin glue has the potential risk of exposure to infectious agents (8). Sakamoto et al. reported that the use of an absorbable sheet alone for re-enforcement of the staple line, without fibrin glue, was effective in preventing postoperative air leakage and in decreasing the recurrence of postoperative PSP (6). We now reinforce the staple line with absorbable sheet alone at our institution, based on their findings. However, a study by Muramatsu et al. revealed a significant reduction in the rate of postoperative PSP recurrence by reinforcement of the staple line with fleece-coated fibrin glue (3), and thus, the utility of fibrin glue cannot be ignored. If POBN could be reliably predicted, then thoracic surgeons could be able to limit fibrin glue reinforcement to resection sites that have a high risk of POBN. With this in my mind we assessed, and subsequently published, data on the relationship between POBN and LW (10). Cox regression analysis showed that LW is the only significant factor affecting POBN occurrence. It is thought that the presence of tension at the staple line is linked to the mechanism of POBN (9). In general, the residual lung gradually approaches its original size, as seen on radiograph or CT. When LW is increased, the residual lung is prone to over-expansion. We hypothesized that tension on the staple line occurs in the process. However, it has been reported that young patients with PSP have a higher postoperative recurrence rate than elderly individuals (11,12). Therefore, the characteristics of POBN may differ according to the patient’s age.
With the exception of our previous study, POBN risk factors have not been reported to differ from those for postoperative PSP recurrence associated with patient backgrounds (10-12). Therefore, we selected LW as the only factor to be evaluated. Because our study was retrospective, patient backgrounds were heterogeneous. We used the IPTW method, as this has previously been used to adjust for these factors in retrospective studies (13-15).
Since the median LW was approximately 4.0 and 3.0 g for the Y and O groups, respectively, we investigated its relationship with POBN by varying the LW cut-off value from 1.0 to 6.0 g. For the Y group, no LW value was a significant risk factor for POBN. On the other hand, in the O group, LW ≥2.0 and ≥3.0 g were significant POBN risk factors (P=0.045 and 0.049, respectively). Although significant differences were observed with both cut-off values, we thought a cut-off value of LW ≥3.0 g was more clinically relevant. The reason why POBN was more frequent in Y group than in O group is unclear. PSP is a single disease that occurs independent of age or smoking habits. However, we believe that PSP includes cases of so-called young, secondary spontaneous pneumothorax (SSP) which develops in association with external factors such as smoking. If this is true, POBN might occur regardless of these external factors following PSP, while young SSP might demonstrate different features that are easily affected by LW.
In the present study, the resected sites were only reinforced with absorbable sheet. Therefore, active reinforcement of the staple line with both fibrin glue and absorbable sheet may in fact be necessary. Although we measured the LW postoperatively in our study, it can also be measured intraoperatively to determine whether the use of fibrin glue is indicated. It is unclear to what extent reinforcement of the staple line with fibrin glue is able to prevent POBN and this warrants further investigation. Furthermore, additional studies are required as the present study was not able to investigate thoroughly the relationship between POBN and PSP recurrence.
Our study has some limitations. The patient population was relatively small, and the study was retrospective. It is very difficult for thoracic surgeons to control LW in a prospective study, as the conditions of bullae are highly variable. Therefore, we think that it is necessary for any future study to analyze retrospectively a larger patient population, sampled from multiple institutions.
Conclusions
This study shows that a LW of ≥3.0 g is a significant risk factor for POBN development in individuals aged 25 years and above. In these sites, intraoperative measurement of LW could be used to indicate when it may be necessary to reinforce the staple line with both fibrin glue and absorbable sheet in order to prevent POBN.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study was approved by the Institutional Review Board of Takasago Municipal Hospital (No. 2016-1).
References
- MacDuff A, Arnold A, Harvey J, et al. Management of spontaneous pneumothorax: British Thoracic Society Pleural Disease Guideline 2010. Thorax 2010;65 Suppl 2:ii18-31. [Crossref] [PubMed]
- Tsuboshima K, Nagata M, Wakahara T, et al. Modified Chest Wall Pulley for Lung Excision during Single-Incision Thoracoscopic Surgery for Primary Spontaneous Pneumothorax. Ann Thorac Cardiovasc Surg 2016. [Epub ahead of print]. [PubMed]
- Muramatsu T, Ohmori K, Shimamura M, et al. Staple line reinforcement with fleece-coated fibrin glue (TachoComb) after thoracoscopic bullectomy for the treatment of spontaneous pneumothorax. Surg Today 2007;37:745-9. [Crossref] [PubMed]
- Lee S, Kim HR, Cho S, et al. Staple line coverage after bullectomy for primary spontaneous pneumothorax: a randomized trial. Ann Thorac Surg 2014;98:2005-11. [Crossref] [PubMed]
- Nakanishi K. An apical symphysial technique using a wide absorbable mesh placed on the apex for primary spontaneous pneumothorax. Surg Endosc 2009;23:2515-21. [Crossref] [PubMed]
- Sakamoto K, Takei H, Nishii T, et al. Staple line coverage with absorbable mesh after thoracoscopic bullectomy for spontaneous pneumothorax. Surg Endosc 2004;18:478-81. [Crossref] [PubMed]
- Hirai K, Kawashima T, Takeuchi S, et al. Covering the staple line with a polyglycolic acid sheet after bullectomy for primary spontaneous pneumothorax prevents postoperative recurrent pneumothorax. J Thorac Dis 2015;7:1978-85. [PubMed]
- Kawamura M, Sawafuji M, Watanabe M, et al. Frequency of transmission of human parvovirus B19 infection by fibrin sealant used during thoracic surgery. Ann Thorac Surg 2002;73:1098-100. [Crossref] [PubMed]
- Inderbitzi RG, Leiser A, Furrer M, et al. Three years' experience in video-assisted thoracic surgery (VATS) for spontaneous pneumothorax. J Thorac Cardiovasc Surg 1994;107:1410-5. [PubMed]
- Tsuboshima K, Nagata M, Wakahara T, et al. Relationship between postoperative bulla neogenesis at the staple line and the resected lung volume in primary spontaneous pneumothorax. Gen Thorac Cardiovasc Surg 2015;63:572-5. [Crossref] [PubMed]
- Noh D, Lee S, Haam SJ, Paik HC, et al. Recurrence of primary spontaneous pneumothorax in young adults and children. Interact Cardiovasc Thorac Surg 2015;21:195-9. [Crossref] [PubMed]
- Jeon HW, Kim YD, Kye YK, et al. Air leakage on the postoperative day: powerful factor of postoperative recurrence after thoracoscopic bullectomy. J Thorac Dis 2016;8:93-7. [PubMed]
- Pagès PB, Delpy JP, Falcoz PE, et al. Videothoracoscopy versus thoracotomy for the treatment of spontaneous pneumothorax: a propensity score analysis. Ann Thorac Surg 2015;99:258-63. [Crossref] [PubMed]
- Deb S, Austin PC, Tu JV, et al. A Review of Propensity-Score Methods and Their Use in Cardiovascular Research. Can J Cardiol 2016;32:259-65. [Crossref] [PubMed]
- Hwang HY, Oh HC, Kim YH, et al. Complete Revascularization of the Three-Vessel Territories Using a Left Internal Thoracic Artery Composite Graft. Ann Thorac Surg 2015;100:59-66. [Crossref] [PubMed]


