Non-intubated subxiphoid uniportal video-assisted thoracoscopic thymectomy using glasses-free 3D vision
Case presentation
Clinical summary
A 42-year-old male presented with an 8-month history of a thymic mass associated with myasthenia gravis (MG). The electromyography (EMG) study was abnormal, and serum acetylcholine receptor (AChR) antibody testing was positive. According to the classification of Myasthenia Gravis Foundation of America (MGFA), the clinical stage of this patient was I. No serious comorbidities, such as a bleeding disorder, sleep apnea, or evidence of potential pleural adhesions were revealed during preoperative evaluation. A well-encapsulated thymoma the size of 3 cm was diagnosed on contrast computer tomography (CT). The tumor did not contact the lung and there were no other signs of infiltration of other mediastinal structures.
Technique
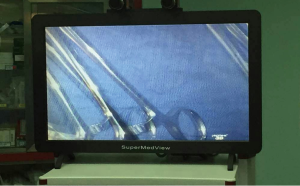
The patient was placed in the lithotomy position and non-intubated spontaneous ventilation anesthesia was initiated. No muscle relaxants were used. Details of the anesthesiologic procedure are described in previous reports (1). A laryngeal mask was used for oxygen support, as well as a facility of conversion if necessary. Subsequently, subxiphoid uniportal video-assisted thoracoscopic surgery (VATS) thymectomy was performed. Our self-developed product, glasses-free 3D thoracoscopic display system—Super Med View (Zhuhai Mingyi Medical Technology Co., Ltd, Zhuhai, China), was used during the entirety of the operation (Figure 1).
The procedure was completed as follows: a single 3-cm transverse skin incision was made 2 cm below the lower edge of the xiphoid. The anterior layer of the rectus sheath was cut and dissected on the reverse side of the xiphoid by the finger. An incision protector (Hakko Co. Ltd. Japan) was placed and a 1-cm thoracoscope with a 30-degree angle was inserted through the port. Once vision of the thoracic cavity was obtained the connective tissue between the sternum and pericardium was cut using a harmonic scalpel (Ethicon, Inc., Somerville, NJ, USA). The right pleura was revealed and opened. We started from right lower to the upper pole of the thymus. The pericardial and the right epiphrenic fat pad were dissected en bloc without any attempt to separate the thymus gland from the thymoma. We then carefully exposed and divided the brachiocephalic vein and innominate artery, and removed all surrounding soft tissue. The branch vessels for thymus blood supply from left internal thoracic artery and left innominate vein were securely dissected using a harmonic scalpel and hemo-lock. The opening of the left pleura and dissection of the left side of the thymus directly followed. Blunt dissection should reach the superior mediastina and lower neck regions, which will enable visualization of the whole upper poles of the thymus and the lower portion of the thyroid. The thymus and all surrounding dissected tissue were placed in a plastic extraction bag and removed through the subxiphoid incision (Figure 2).
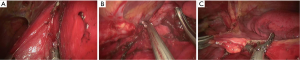
Upon completion of surgery, a 24 F chest drainage tube was inserted and set to the anterior mediastinum through the incision. During the operation, the lowest PaO2 and the peak EtCO2 were 96% and 42 mmHg, respectively. Operative duration was 120 min and total operative blood loss was 40 mL. The patient was sent back to ward after full anesthesthetic recovery in the post-anesthesia care unit (PACU). No myasthenia crisis or other complications occurred postoperatively. The chest drain was removed 1 day after surgery. The patient was discharged on postoperative day 3. The final pathologic examination confirmed the diagnosis of thymic hyperplasia.
Discussion
This is the first report showing non-intubated subxiphoid uniportal video-assisted thoracoscopic thymectomy using glasses-free 3D vision. This subxiphoid approach provides an excellent view of the bilateral pleural cavities, which is essential for adequate mediastinal fatty tissue dissection, especially because the surgical plan calls for removal of all the bilateral pericardiophrenic fat pads and the mediastinal fat tissue between the bilateral phrenic nerves.
VATS thymectomy is completed by revealing and opening the double pleura one after the other, The completion time for the first surgical area (right pleural side) was 60 min and the completion of the left (when both pleura were opened) was 30 min. The PaO2 and EtCO2 were stable without need for conversion to intubation. In addition, we think rib arch can be raised by device if the operation space is limited.
Non-intubated anesthesia has emerged with reliable results and has been reported to reduce the adverse effects of tracheal intubation and general anesthesia with encouraging results (2,3). In our institute, we have completed more than 1,800 VATS procedures under spontaneous respiration. This method benefits the patient by minimizing the side effects of anesthesia allowing the patient a faster recovery.
The glasses-free 3D thoracoscopic display system was developed and applied in thoracic surgery for the first time by our surgical team in May, 2015 (4). Compared to the traditional 3D display system, our system is advantageous to the surgeon by allowing the surgeon to see the high definition 3D image without polarized lenses changing the light and coloring of the image. In this way the image coloring and comfort that is expected from a high definition 2D screen is combined with the depth perception and exactitude experienced with a 3D image. In our experience this 3D image also reduced the burden and fatigue commonly experienced when using 3D glasses, especially for surgeons that must wear corrective lenses as well.
Subxiphoid uniportal video-assisted thoracoscopic thymectomy is safe and feasible. The use of the glasses-free 3D display provides better surgical conditions, clearer views, and brighter images to help surgeons more comfortably complete operations.
Acknowledgements
Funding: This study was supported by the Science and Technology Planning Project of Guangdong Province, China (20140215).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Guo Z, Yin W, Wang W, et al. Spontaneous ventilation anaesthesia: total intravenous anaesthesia with local anaesthesia or thoracic epidural anaesthesia for thoracoscopic bullectomy. Eur J Cardiothorac Surg 2016;50:927-932. [Crossref] [PubMed]
- Chen JS, Cheng YJ, Hung MH, et al. Nonintubated thoracoscopic lobectomy for lung cancer. Ann Surg 2011;254:1038-43. [Crossref] [PubMed]
- Liu J, Cui F, Li S, et al. Nonintubated video-assisted thoracoscopic surgery under epidural anesthesia compared with conventional anesthetic option: a randomized control study. Surg Innov 2015;22:123-30. [Crossref] [PubMed]
- Li M. The world's first radical resection for lung cancer using glasses-free 3D thoracoscope was completed in Guangzhou. J Thorac Dis 2015;7:E384-5. [PubMed]