Current situation of asthma-COPD overlap syndrome (ACOS) in Chinese patients older than 40 years with airflow limitation: rationale and design for a multicenter, cross-sectional trial (study protocol)
Introduction
In the continuum of chronic airway diseases, asthma and chronic obstructive pulmonary disease (COPD) are undoubtedly the common conditions considered as distinct clinical entities (1). However, a significant proportion of patients often present with overlapping conditions, which has now become a major health concern worldwide, accounting for approximately 15–25% of the obstructive airway diseases with patients experiencing worse outcomes compared with either of the conditions alone (2-4). Majorly, patients of a chronic airway disease present with a syndrome comprising symptoms of both asthma and COPD, the exact definition of which remains ambiguous (2). The Global Initiative for Chronic Obstructive Lung Disease (GOLD) proposed a term “asthma-COPD overlap syndrome” (ACOS) in 2014 to define this overlapping condition based on a detailed review of available literature and consensus (4). To simplify, ACOS represents a condition of an asthmatic smoker who advances to chronic airflow obstruction with an unknown history of asthma, with symptoms of increased variability of airflow in association with incompletely reversible airflow obstruction (5). The prevalence of ACOS tends to increase with age in asthmatic individuals with estimates of >50% and in patients with COPD up to 23% at ages of ≥80 and >50 years, respectively (6). This reflects that ACOS develops gradually in patients with asthma and COPD (7,8). Furthermore, lack of specific biomarkers for ACOS makes the diagnosis more difficult (5). Recurrent exacerbations, rapid disease progression, diminished health-related quality of life, rapidly deteriorating lung function, high co-morbidities, increased reversibility of airflow obstruction, eosinophilic bronchial and systemic inflammation, frequent hospitalization, and high mortality rates are frequently observed in such patients and they tend to receive an inconsistent healthcare management compared with either of the conditions alone (3-5,9,10). A stepwise approach for diagnosis and treatment of asthma, COPD, and ACOS is advised in the recent 2015 Global Initiative for Asthma (GINA) report along with differentiating features that identify and characterize ACOS (4). However, GINA did not clarify whether ACOS is a coexistence of asthma and COPD or a subtype of chronic airflow limitation. Few studies have been conducted to provide a fair understanding of ACOS manifested by both asthma and COPD symptoms (9,11,12). Studies from the western population have shown the prevalence of ACOS to be 1.8% when diagnosed using spirometry (13) and 2.7% when diagnosed based on self-reported or physician-diagnosed asthma and COPD (14). Furthermore, the prevalence of ACOS (3.2%) was lower than COPD (6.0%) or asthma alone (5.6%) in the United States (15), whereas the percentage of patients visiting emergency departments was high for ACOS than for COPD alone in Korea (16). This is associated with utilization of a large proportion of medical resources and, in turn, leading to higher healthcare costs because hospitalizations account to the largest expenditure, thereby imposing heavy economic burdens on patients (17). Previous research conducted in urban China, 2010, 2012, and 2013 China National Health and Wellness and internet-based Survey (NHWS) revealed a high incidence of ACOS in urban China, which was associated with the greatest co-morbidity burden (P<0.05) compared with asthma and COPD along with worse healthcare outcomes (18). The proportion, features, prognosis, and clinical practice of ACOS are still poorly recognized in China. Moreover, criteria for ACOS diagnosis still remain unclear and require more research. Early identification of patients with ACOS has significant therapeutic implications as well, such as restraining the use of long-acting bronchodilators. Patients with ACOS have enhanced response to ICS treatment (12). As per the Canadian guidelines 2007, early use of ICS is justified in ACOS (19). Because of the increasing burden of ACOS in global healthcare system and the sparse data availability of literature-based evidence in China, there is a critical need of understanding the epidemiology, features, and current clinical practice of ACOS in China. The specific and differential treatment required for patients with ACOS justifies the need to distinguish them from patients with asthma and COPD. This study was designed to investigate the distributions of ACOS, asthma, and COPD in patients >40 years of age with chronic airflow limitation in China along with evaluating the main clinical practice and features of these diseases. The study will also explore the factors that may influence the exacerbations and severity of ACOS in Chinese patients.
Methods
Study design
This is a multicenter, cross-sectional, observational study (NCT02600221) that will collect data from medical records or patient- or physician-reported data from approximately 20 sites from six geographical regions of China including northeast, north, south, east, west, and central China. The site numbers allocated to the six regions are generally consistent with the population (patients) distribution. Only tier-3 hospitals with GCP certificates will be selected as the study sites because those sites are well qualified to conduct this observational clinical study on ACOS. The planed study duration is from December 2015 to December 2016. This study is currently recruiting participants. Approximately 50–150 patients will be recruited from each site consecutively. That is, all eligible patients who consent to participate in this study will be recruited without any prejudice or preference from study personnel. All centers will have highly trained, experienced personnel. Investigators will be selected if they are respiratory physicians working in the respiratory department of tier-3 hospitals and are able to recruit and manage the expected number of patients with asthma, COPD, or ACOS in the stipulated time of 1 year. Physicians should have patient spirometric information available in the patient’s medical files [post-bronchodilator forced expiratory volume (post-BD FEV1% pred.) and post-bronchodilator forced vital capacity (post-BD FEV1/FVC)] and spirometries must be according to the guidelines (20). A total of 2,000 participants who meet the entry criteria will be enrolled in the study. This study will be carried out under routine clinical practice. Drug treatment or examinations will be determined by the physicians responsible for treatments and no investigational drugs will be used to treat asthma, COPD, or ACOS. Data about current medications and dosages used for treatment of the diseases or regarding concomitant medications will be collected at the visit. All the data pertaining to study outcomes will be recorded in CRF. The outcomes are expected to reflect the actual situation about ACOS in China.
Study participants
Participants will be recruited from the study sites if they fulfill the following inclusion criteria: age ≥40 years, male or female, clinically diagnosed asthma, and COPD/chronic bronchitis/emphysema or ACOS for at least 12 months with airflow limitation (post-BD FEV1/FVC: <0.7). Patients will be excluded if they have been involved in another clinical trial in the past 3 months, have acute exacerbation or have other respiratory diseases that can influence airflow, such as lung cancer, tuberculosis, pneumonia, and bronchiectasis, and are unable to understand the study procedures or unable/reluctant to answer the questionnaire as judged by the investigator. The study will be performed in accordance with the ethical principles of the Declaration of Helsinki and will also be consistent with the International Conference on Harmonization and Good Clinical Practice. The study protocol, including the Informed Consent Form, is approved by an Independent Ethics Committee (IEC). The principal investigator(s) at each center will ensure that the patients are provided with adequate oral and written information about the purpose, as well as possible risks and benefits of the study. Participants will also be informed of their independence to discontinue participation at any time. The participants will be given the opportunity to ask any questions at any time regarding the information provided. Patients will have to provide signed consent form before participating in the study and their information will be kept anonymous.
Study outcomes
Primary variable
The proportion of ACOS among patients older than 40 years with airflow limitation (post-BD FEV1/FVC: <0.7) based on GINA and GOLD 2015 definitions was considered as the primary variable (4).
Secondary variables
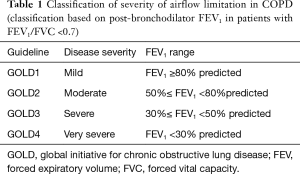
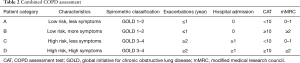
Secondary variables included determination of the proportions of COPD and asthma among patients older than 40 years with airflow limitation based on GINA and GOLD 2015 definitions, respectively (4). The distributions of the severity of airflow limitation according to GOLD lung function grading based on post-BD FEV1 in patients with ACOS, COPD, or asthma (Table 1), distribution of groups according to GOLD 2015 group definition (A, B, C, and D) in patients with ACOS or COPD (Table 2), and distribution of medication by drug class in patients with ACOS, asthma, or COPD were also determined. In addition, the proportion of ACOS patients with a previous diagnosis of asthma/COPD/chronic bronchitis/emphysema was determined. Acute exacerbation history in 12 months before the visit (the number of exacerbations, severity of exacerbation (using systemic hormones/antibiotics/emergency/hospitalization), days of hospitalization or emergency room visit, and severity of ACOS as evaluated using COPD Assessment Test (CAT; mild, moderate, severe, and very severe), Asthma Control Questionnaire (ACQ-5; complete control, good control, and uncontrolled), and Modified British Medical Research Council (mMRC; 0, 1, 2, 3, and 4) were also assessed in patients with ACOS.
Full table
Full table
Data analyses
Sample size justification
Considering that ACOS accounts for approximately 15–25% of the obstructive airway diseases and on the basis of previous studies, we expected that the proportion of patients with ACOS will be 20% among Chinese population (>40 years of age) with airflow limitation. With a sample size of 2,000 patients, the precision (half-length of 95% CI) of the ACOS proportion estimate will be 1.8%, which would adequately suffice the requirement of the study.
Statistical and analytical plans
Statistical analysis will be conducted based on the availability of data, and missing or incomplete data will be excluded from the analysis. Descriptive statistics will be used for analyzing primary and secondary outcomes. Continuous data will be expressed as number of patients, mean ± SD, or median. Categorical data will be expressed as frequency and percentages along with the 95% CI. Summary will be provided for ACOS, COPD, and asthma separately wherever applicable, as well as for overall. To explore the risk factors (continuous or categorical), univariate and multivariate Poisson regression analyses will be performed with grouped number of exacerbation as the dependent variable and the selected patient characteristics or/and clinical practices [gender, age, educational level, allergic history, smoking status, disease history (diagnosis/course), FEV1% pred., etc.] as the independent variables. For multivariate analysis, the selection of predicted factors will be processed by backward stepwise algorithm using a cutoff of 0.15. Similar risk factor analyses will be applied on the severity of patients with ACOS evaluated using CAT, ACQ-5, and mMRC. Statistical analyses will be performed using SAS Version 9.3 (SAS Institute Inc., Cary, NC); a P value of <0.05 will be used to indicate statistical significance.
Study implications
Patients with ACOS comprise individuals who are usually smokers or nonsmokers with long-standing asthma that eventually develops to COPD. Concurrent doctor-diagnosed asthma and COPD have been reported in 15% to 20% of the patients. COPD gene and EPI-SCAN studies reported that approximately 13% and 17.4% of patients with COPD, respectively, have a history of asthma, and 22.8% of the patients with an FEV1/FVC of <0.7 reported of having a previous diagnosis of asthma in the PLATINO study (5,20-27). This is the first multicenter, observational cross-sectional trial conducted to determine the current situation, main clinical practices, and features of ACOS, asthma, and COPD in Chinese patients (>40 years of age) with airflow limitation. Hence, the findings of this study may add significant data to the previous NHWS.
In China, among all adults in the NHWS, 0.61% had ACOS (N=366), and 30.73% and 18.60% of those with asthma and COPD, respectively, had ACOS. Notably, patients with ACOS reported higher comorbidity burden and significantly worse health outcomes (13). Despite demonstrating clinically high significance, thorough understanding of the features and current clinical practice of ACOS remains elusive. There exists an unmet need on the data available regarding management of patients with ACOS as the patients are typically excluded from therapy trials for asthma or COPD. This indicates that the current data on efficacy of treatment may be irrelevant for the growing proportion of older patients with obstructive lung disease, and thus, the understanding and necessity to include ACOS in drug evaluation programs are demanded (24). Physicians seek clarity for differentiating asthma, COPD, and ACOS and land up in non-systematic use of varying diagnostic labels such as asthma with chronic bronchitis, chronic obstructive bronchitis, asthma with permanent obstruction, and COPD with a reversible component, which leads to a high uncertainty in understanding a case description (24). As a result of lack of diagnostic skills, delay in diagnostic testing, and underestimation of the symptom severity, patients become reluctant to consult the physician, which overall contribute toward underdiagnosis. Furthermore, the condition is aggravated and continued exposure to risk factors without adequate diagnosis will cause the condition to become worse. Understanding the clear diagnostic criteria and prospective validation of ACOS will be of great value in determining the optimal management strategies for ACOS.
Considering the continuous population increase in China and medical advancements, the overall death rate is slowed, but there is a rapid increase in the proportion of geriatric patients (28). Knowing that patients with ACOS are usually older in age, the possibility of the Chinese geriatric group having pulmonary diseases will also increase manifold. Currently, chronic respiratory diseases are the second leading cause of death in China (29). Studying the current status and management of ACOS in China may lead to identification of mechanistic pathways involved in it, which will lead in early identification of ACOS syndrome in patients and will subsequently result in providing appropriate care at proper time, thereby preventing the accelerated deterioration of lung function. Thus, the current study will prove to be very crucial in a growing country such as China and will add scientific knowledge on the current understanding of ACOS and management. Even though ACOS progresses as an indistinct entity and has clinical and pathophysiological features that often appear similar to those of asthma or COPD, we must emphasize the importance of the syndrome because of the following reasons:
- More frequent exacerbations than patients with COPD;
- Higher rates of dyspnea and wheezing (but not more cough and sputum), increased reversibility of airflow, and reduced physical activity compared with either disease alone;
- Poorer health-related quality of life, higher hospitalization rate, and lower self-rated health. Appropriate diagnosis and treatment on time will have implications on improving QoL of patients and reducing the financial impact;
- Patients with ACOS require 2- to 6-fold more healthcare resources compared with either disease alone (5,20).
Although asthma and COPD are two different entities, both the GINA and GOLD define ACOS as a syndrome characterized by persistent airflow limitation with several features usually associated with asthma and COPD. Studies suggest that patients with ACOS share the same demographic features and exhibit similar patterns on pulmonary function test as those with only COPD. Furthermore, patients with asthma are at a significant risk for the future development of COPD, which in turn may accelerate ACOS (3). Therefore, this overlap has challenged the differential diagnosis of COPD and asthma with persistent airflow limitation, especially in smokers and geriatric patients. To overcome this challenge, the scientific committee of GINA and GOLD has jointly set guidelines on systematic diagnosis approach for identification of respiratory diseases in 2014, which were revisited in 2015. These guidelines elaborate the clinical features of asthma and COPD, features that favor the development of asthma or COPD, and also diagnosis based on spirometric differences.
The syndromic diagnosis is mainly a 3-step approach:
- Assemble the features that favor a diagnosis of asthma or of COPD;
- Compare the number of features in favor of a diagnosis of asthma or a diagnosis of COPD;
- Consider the level of certainty around the diagnosis of asthma or COPD, or whether there are features of both, suggesting ACOS (30).
Patients aged >40 years with respiratory symptoms including external dyspnea, persistent airflow limitation not fully reversible, a history of doctor-diagnosed asthma, allergies or familial history of asthma and/or exposure to noxious exposures, chest X-rays similar to COPD, more common exacerbations than COPD, and presence of eosinophils and/or neutrophils in sputum are the major diagnostic features of ACOS suggested by GINA and GOLD (30). However, the joint committee urges a need for more research on the clinical and physiological characteristics, biomarkers, outcomes, and underlying mechanisms with broader population groups with respiratory symptoms to strengthen the existing knowledge on ACOS.
Several researchers have been extensively studying on the differential diagnosis of ACOS from asthma and COPD. Xie et al. reported that asthmatic patients with a high emphysema index fulfill the features of ACOS, as described in the GINA and GOLD guidelines, suggesting quantitative CT measurements of emphysema in diagnosing ACOS (31). Furthermore, when the quality of life was studied as a feature of differential diagnosis, patients with ACOS reported higher disease impacts and dyspnea sensation not proportional to the severity of airflow limitation (32).
Given the fact that patients with ACOS are often excluded from asthma and COPD clinical trials, there is a lack of available evidence on the clinical features of ACOS. In our opinion, insights from the current study will aid in redefining the guidelines in China for optimum benefits in the management of ACOS as it exhibits greater risks of acute respiratory events in all age groups for both women and men (20).
Our study has several strengths: It adds significant data to the existing knowledge pertaining to not only ACOS but also asthma and COPD. It we will be analyzing the records of physician-diagnosed diseases rather than patient-reported diagnoses and outcomes, which will depict real-world situation of China. Moreover, this is the first observational study to detect the ACOS situation in China conducted across 20 sites, which will depict the current status of ACOS and will improve the knowledge of physicians. Exacerbation rates will be analyzed by using Poisson regression model, which is the recommended method for analyzing exacerbations (33). Nevertheless, our study also has a limitation of being a non-interventional trial, because of which, not all variables may be collected in all the enrolled patients.
The current treatment guidelines provide scant evidence for the management of ACOS in patients (34); the outcomes of current study may be of prime interest to physicians in defining the clinical features of ACOS, which may in turn aid in deciding effective treatment strategies and improving the clinical outcomes. The present study will also consider the key clinical features defined by the Spanish guideline for COPD (GesEPOC) (35) and the ACOS consensus statement (36) for a post-hoc analysis.
In summary, the findings may provide a comprehensive understanding of significant clinical impact depicted by ACOS and will emphasize the need for clear diagnostic criteria to provide the optimal and cost-effective management approaches for patients with ACOS.
Acknowledgements
This study was funded by AstraZeneca Co Ltd. The authors thank Dr. Amit Bhat (Indegene Pvt Ltd, Bangalore) for providing necessary writing assistance and editorial support toward the development of the manuscript, funded by AstraZeneca.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study protocol was approved by the institutional ethics committees of: (I) The First Affiliated hospital of China medical university [Approval ID: (2016)2015-142-2]; (II) Shengjing Hospital (China Medical University) (Approval ID: 2015PS324K); (III) Peking University Third Hospital (Approval ID: 2015-73-QT-HXK); (IV) West China Hospital, Sichuan University [Approval ID: 2015(295)]; (V) First Affiliated Hospital of Guangzhou Medical College (Approval ID: 2015-68); (VI) Shanghai Jiaotong University School of Medicine Ruijin Hospital [Approval ID: 2015(84)]; (VII) Beijing Union Medical College Hospital of Chinese Academy of Medical Sciences (Approval ID: B153); (VIII) Beijing Chaoyang Hospital, Capital University of Medical Sciences (Approval ID: 2015-2); (IX) Fudan University, East China Hospital (Approval ID: 20150239); (X) Henan Provincial People’s Hospital [Approval ID: 2015(37)]; (XI) First Affiliated Hospital of Xi’an Jiaotong University (Approval ID: XJTU1AF2015LSY-65); (XII) General Hospital of Tianjin Medical University (Approval ID: IRB2015-103-01); (XIII) Second Affiliated Hospital of Zhejiang University Medical College (Approval ID: 2015-083); (XIV) General Hospital of Chinese PLA Shenyang Military Region [Approval ID: (2015)38]; (XV) Chinese People’s Liberation Army 202 Hospital (Approval ID: 202H2016PJ001); (XVI) The First Affiliated Hospital of Sun Yat-sen University (Approval ID: 2016019); (XVII) Affiliated Hospital of Inner Mongolia Medical University [Approval ID: 2015(007)]; (XVIII) Hainan Provincial People’s Hospital [Approval ID: (2016)10]; (XIX) Second Affiliated Hospital of the Third Military Area of Chinese People’s Liberation Army (Approval ID: 2016023); (XX) Second Xiangya Hospital of Central South University [Approval ID: 2016(017)].
References
- Kim SR, Rhee YK. Overlap Between Asthma and COPD: Where the Two Diseases Converge. Allergy Asthma Immunol Res 2010;2:209-14. [Crossref] [PubMed]
- Papaiwannou A, Zarogoulidis P, Porpodis K, et al. Asthma-chronic obstructive pulmonary disease overlap syndrome (ACOS): current literature review. J Thorac Dis 2014;6 Suppl 1:S146-51. [PubMed]
- Alshabanat A, Zafari Z, Albanyan O, et al. Asthma and COPD Overlap Syndrome (ACOS): A Systematic Review and Meta Analysis. PLoS One 2015;10:e0136065. [Crossref] [PubMed]
- Global Initiative for Asthma. Global Strategy For Asthma Management And Prevention Guidelines 2015 [Internet]. [cited 2016 Mar 23]. Available online: http://ginasthma.org/
- Barrecheguren M, Esquinas C, Miravitlles M. The asthma-chronic obstructive pulmonary disease overlap syndrome (ACOS): opportunities and challenges. Curr Opin Pulm Med 2015;21:74-9. [Crossref] [PubMed]
- Soriano JB, Davis KJ, Coleman B, et al. The proportional Venn diagram of obstructive lung disease: two approximations from the United States and the United Kingdom. Chest 2003;124:474-81. [Crossref] [PubMed]
- Vonk JM, Jongepier H, Panhuysen CI, et al. Risk factors associated with the presence of irreversible airflow limitation and reduced transfer coefficient in patients with asthma after 26 years of follow up. Thorax 2003;58:322-7. [Crossref] [PubMed]
- Perret JL, Dharmage SC, Matheson MC, et al. The interplay between the effects of lifetime asthma, smoking, and atopy on fixed airflow obstruction in middle age. Am J Respir Crit Care Med 2013;187:42-8. [Crossref] [PubMed]
- Zeki AA, Schivo M, Chan A, et al. The Asthma-COPD Overlap Syndrome: A Common Clinical Problem in the Elderly. J Allergy (Cairo) 2011;2011:861926.
- Kauppi P, Kupiainen H, Lindqvist A, et al. Overlap syndrome of asthma and COPD predicts low quality of life. J Asthma 2011;48:279-85. [Crossref] [PubMed]
- Soler-Cataluña JJ, Cosío B, Izquierdo JL, et al. Consensus document on the overlap phenotype COPD-asthma in COPD. Arch Bronconeumol 2012;48:331-7. [Crossref] [PubMed]
- Bujarski S, Parulekar AD, Sharafkhaneh A, et al. The asthma COPD overlap syndrome (ACOS). Curr Allergy Asthma Rep 2015;15:509. [Crossref] [PubMed]
- Ding B, DiBonaventura M, Karlsson N, et al. Asthma-chronic obstructive pulmonary disease overlap syndrome in the urban Chinese population: prevalence and disease burden using the 2010, 2012, and 2013 China National Health and Wellness Surveys. Int J Chron Obstruct Pulmon Dis 2016;11:1139-50. [PubMed]
- O'Donnell DE, Aaron S, Bourbeau J, et al. Canadian Thoracic Society recommendations for management of chronic obstructive pulmonary disease - 2007 update. Can Respir J 2007;14 Suppl B:5B-32B.
- Kumbhare S, Pleasants R, Ohar JA, et al. Characteristics and Prevalence of Asthma/Chronic Obstructive Pulmonary Disease Overlap in the United States. Ann Am Thorac Soc 2016;13:803-10. [Crossref] [PubMed]
- Menezes AM, Montes de Oca M, Pérez-Padilla R, et al. Increased risk of exacerbation and hospitalization in subjects with an overlap phenotype: COPD-asthma. Chest 2014;145:297-304. [Crossref] [PubMed]
- Diaz-Guzman E, Khosravi M, Mannino DM. Asthma, chronic obstructive pulmonary disease, and mortality in the U.S. population. COPD 2011;8:400-7. [Crossref] [PubMed]
- Rhee CK, Yoon HK, Yoo KH, et al. Medical utilization and cost in patients with overlap syndrome of chronic obstructive pulmonary disease and asthma. COPD 2014;11:163-70. [Crossref] [PubMed]
- Toy EL, Gallagher KF, Stanley EL, et al. The economic impact of exacerbations of chronic obstructive pulmonary disease and exacerbation definition: a review. COPD 2010;7:214-28. [Crossref] [PubMed]
- Chung WS, Lin CL, Kao CH. Comparison of acute respiratory events between asthma-COPD overlap syndrome and COPD patients: a population-based cohort study. Medicine (Baltimore) 2015;94:e755. [Crossref] [PubMed]
- Miller MR, Hankinson J, Brusasco V, et al. Standardisation of spirometry. Eur Respir J 2005;26:319-38. [Crossref] [PubMed]
- Hardin M, Silverman EK, Barr RG, et al. The clinical features of the overlap between COPD and asthma. Respir Res 2011;12:127. [Crossref] [PubMed]
- Miravitlles M, Soriano JB, Ancochea J, et al. Characterisation of the overlap COPD-asthma phenotype. Focus on physical activity and health status. Respir Med 2013;107:1053-60. [Crossref] [PubMed]
- Gibson PG, Simpson JL. The overlap syndrome of asthma and COPD: what are its features and how important is it? Thorax 2009;64:728-35. [Crossref] [PubMed]
- Regan EA, Hokanson JE, Murphy JR, et al. Genetic epidemiology of COPD (COPDGene) study design. COPD 2010;7:32-43. [Crossref] [PubMed]
- Tálamo C, de Oca MM, Halbert R, et al. Diagnostic labeling of COPD in five Latin American cities. Chest 2007;131:60-7. [Crossref] [PubMed]
- Menezes AM, Victora CG, Perez-Padilla R, et al. The Platino project: methodology of a multicenter prevalence survey of chronic obstructive pulmonary disease in major Latin American cities. BMC Med Res Methodol 2004;4:15. [Crossref] [PubMed]
- Flaherty JH, Liu ML, Ding L, et al. China: the aging giant. J Am Geriatr Soc 2007;55:1295-300. [Crossref] [PubMed]
- Chronic Respiratory Diseases. World Health Organisation Website [Internet]. [cited 2016 May 19]. Available online: http://www.who.int/gard/publications/chronic_respiratory_diseases.pdf
- Diagnosis of diseases of chronic airway limitation: Asthma COPD and Asthma-COPD overlap syndrome (ACOS). Upated 2015. A joint project of GINA and GOLD [Internet]. [cited 2016 Oct 13]. Available online: http://www.everyday-breathing.com/media/15569/asthmacopdoverlap.pdf
- Xie M, Wang W, Dou S, et al. Quantitative computed tomography measurements of emphysema for diagnosing asthma-chronic obstructive pulmonary disease overlap syndrome. Int J Chron Obstruct Pulmon Dis 2016;11:953-61. [Crossref] [PubMed]
- Kurashima K, Takaku Y, Ohta C, et al. COPD assessment test and severity of airflow limitation in patients with asthma, COPD, and asthma-COPD overlap syndrome. Int J Chron Obstruct Pulmon Dis 2016;11:479-87. [Crossref] [PubMed]
- Keene ON, Jones MR, Lane PW, et al. Analysis of exacerbation rates in asthma and chronic obstructive pulmonary disease: example from the TRISTAN study. Pharm Stat 2007;6:89-97. [Crossref] [PubMed]
- Bateman ED, Reddel HK, van Zyl-Smit RN, et al. The asthma-COPD overlap syndrome: towards a revised taxonomy of chronic airways diseases? Lancet Respir Med 2015;3:719-28. [Crossref] [PubMed]
- Miravitlles M, Soler-Cataluña JJ, Calle M, et al. Spanish guideline for COPD (GesEPOC). Update 2014. Arch Bronconeumol 2014;50 Suppl 1:1-16. [PubMed]
- Sin DD, Miravitlles M, Mannino DM, et al. What is asthma-COPD overlap syndrome? Towards a consensus definition from a round table discussion. Eur Respir J 2016;48:664-73. [Crossref] [PubMed]


