A bench evaluation of fraction of oxygen in air delivery and tidal volume accuracy in home care ventilators available for hospital use
Introduction
Ventilators can be used in a large variety of medical settings including operating room, pre-hospital setting, emergency room, pneumology ward, intensive care unit (ICU), and at home for long-term mechanical ventilation. ICU ventilators and home care ventilators (HCV) are fundamentally different.
Comparison of differences of ICU and HCV
Of notice, ICU ventilators are fed by pressurized gas and allow direct setting of accurate inspiratory fraction of oxygen in air (FIO2) over a wide range (21–100%). HCV are piston- or turbine-driven and are limited in their capability to deliver high FIO2. Turbine-driven ventilators can be used in the ICU setting and have been shown to perform in the range of the newest ICU ventilators in terms of triggering sensitivity and quality of pressurization (1). On the bench and in patients dedicated ventilators to noninvasive ventilation were found with a better patient-ventilator synchrony than ICU ventilators even if these latter were set with their specific noninvasive mode (2-4).
Problems of FIO2 and tidal volume (VT), use and indications of HCV in hospital and ICU
In the hospital setting HCV can be used to provide non-invasive ventilator support to patients with mild to moderate acute respiratory failure (5). Moreover, HCV could be of importance in specific situations e.g., during ICU bed or ICU ventilator shortage during pandemics or other multi-patient situations. It is, therefore, very important to verify that these ventilators have the right capabilities to meet patients’ needs. The advantage of a turbine is that it means the ventilator can operate without high-pressure compressed air. The potential limitations of a turbine include the risk of the gas reaching a high temperature at the ventilator outlet, the lack of accuracy in FIO2 when the oxygen is added, and the lack of accuracy VT delivery for patients with a marked impairment in respiratory mechanics (6). A previous bench study demonstrated acceptable temperatures at the outlets of turbine ventilators, and hence a very low risk of humidifier dysfunction (7). One bench study pointed out heterogeneity in VT delivery with HCV and mouthpiece (8). FIO2 delivery and VT accuracy in HCV have received less attention. Thus, we carried out the present bench study to investigate the performance of the HCV, all of them used in our ICU and hypothesized that HCV differed for both FIO2 delivery and VT accuracy.
Methods
Present study was not submitted to an IRB because it was a bench study that did not involve and include any patients.
Equipment
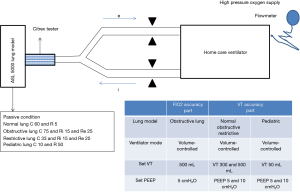
The set-up comprised of the following items (Figure 1): (I) Four HCV: Astral 150 (ResMed), Elisée 150 (ResMed), Monnal T50 (Air Liquide Medical System), and Trilogy 200 (Philips); (II) the ASL 5000 Active Servo Lung model (IngMar Medical, Pittsburgh, PA, USA); (III) a ventilator tester (Citrex H4TM, imtmedical, Buchs, Switzerland), which contains devices for measuring oxygen concentration in the air, gas temperature and pressure; (IV) a double limb ventilator circuit (Intersurgical, Fontenay Sous-bois, France) of 22 mm internal diameter (ID) and 1.70 m length per limb; (V) a flow-meter (Floval, Air Liquide Médical System, Antony, France) to adjust the rate of oxygen supply delivered from the wall at high pressure (3.5 bars). The four HCV and the ICU ventilator presently investigated were selected because they are used in our unit composed of a 15-bed medical ICU, a 5-bed step down unit, and a 6-bed respiratory medicine unit which is responsible for long-term home ventilated patients. The Astral 150, Elisée 150, Monnal T50 are used in our ICU and were purchased by the institution, and the Trilogy 200 was provided by the manufacturer. However, for the purposes of the present study the four HCV used were all brand-new devices provided by the manufacturers.
Protocol
The experiments were conducted in our laboratory at room temperature. Before the measurements were taken the tester was calibrated then plugged into the ASL 5000 and connected to a laptop computer. The ventilators were submitted to a full test before use according to the manufacturer’s recommendations.
The protocol comprised of two parts.
The first part evaluated the delivery of FIO2. The ASL 5000 was set to passive condition, with lung compliance (C) and resistance (R) mimicking obstructive lung: nonlinear C 75 mL/cmH2O, inspiratory R 15 cmH2O/L/s and expiratory R 25 cmH2O/L/s. HCV were used in volume controlled mode (VC) at constant flow inflation and set to VT 500 mL, positive end-expiratory pressure (PEEP) 5 cmH2O, breathing frequency 15 cycles/min and inspiratory time 0.8 s, inspiratory trigger off. The HCV was supplied with room air or pure oxygen from the hospital wall at rates of 3 and 15 L/min. Oxygen was administered to the rear of the HCV via a specific low pressure plug, which was the same across the ventilators. The FIO2 signal was recorded at 200 Hz and continuously displayed on the computer screen. Each level of gas was supplied to the ventilator until FIO2 reached a plateau.
The second part of the study evaluated the accuracy of VT delivery. The ASL 5000 was set in passive mode to mimic a normal adult lung (linear C 60 mL/cmH2O, inspiratory and expiratory R 5 cmH2O/L/s), an obstructive lung as described above, or restrictive lung (linear C 33 mL/cmH2O, inspiratory R 15 cmH2O/L/s and expiratory R 25 cmH2O/L/s) and to mimic pediatric lungs (linear C 10 mL/cmH2O, inspiratory and expiratory R set to 50 cmH2O/L/s). The HCV were set in VC, with triggering off. For the three adult conditions the target VT was 300 and 500 mL, each tested at both 5 and 10 cmH2O PEEP. Target VT of 50 mL was tested for the pediatric lung conditions at the same PEEP levels. All ventilators were set to body temperature pressure saturated (BTPS). The volume signal was acquired at 200 Hz for 2 min under each condition.
The various settings used to determine the lung configurations at the ASL 5000 lung model were taken from the literature and notably from (9-11) for the obstructive lung, (12) for the restrictive lung and (13-16) for the pediatric lung.
No leak, either intentional or nonintentional, was present in our experimental set-up.
Data analysis
We used Flowlab software (imtmedical, Buchs, Switzerland) to measure both FIO2 and VT because our ASL 5000 was not equipped to measure FIO2. The accuracy of the Citrex H4TM device is ±1% for FIO2 measurement and ±2% for volume measurement.
FIO2 was measured over the last ten breaths during the plateau in FIO2. Plateau was defined as an average change in FIO2 <10% as compared to the previous ten breaths. For each ventilator, at each oxygen supply rate and each ventilator circuit, the values of FIO2 were averaged over ten consecutive breaths.
Ten consecutive breaths were used to measure VT. The volume error was defined as follows:
(measured VI − targeted VI)/targeted VI × 100
and expressed as percentage. A positive or a negative value for the volume error indicates overestimation or underestimation, respectively, of the measured volume relative to the value set on the ventilator.
Given the nature of the investigation, i.e., a bench experiment, we expected no or very low within-ventilator variability for the FIO2 and VT values, for any given ventilator and condition tested. It was therefore decided, a priori to not perform statistical tests if this assumption was verified. Therefore, any observed differences in mean FIO2 and VT were considered as true. In case of standard deviations different from zero the statistical analysis was done and the comparison between ventilators was performed by using one-factor ANOVA with a Bonferroni correction for multiple tests.
The data are presented as mean ± standard deviation unless otherwise stated. The accuracy of VT delivery was defined within a range of ±10% on both sides of the mean value for volume error. This 10% value was chosen because it is the average difference in lung volume between BTPS and ambient temperature pressure dry conditions and, is therefore relevant. It has also been used in previous studies, including one of the recent bench evaluation of ventilators (17).
The statistical analysis was carried out using R software, version 2.15.2 (R Development Core Team. R: A Language and Environment for Statistical Computing. In Vienna, Austria: R Foundation for statistical Computing; 2009).
Results
FIO2 efficiency
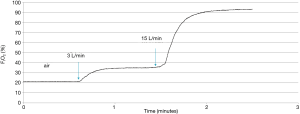
Three experiments were performed for each ventilator for this part of the study. A representative tracing of continuous FIO2 measurement at different oxygen supplementation rates is shown in Figure 2.
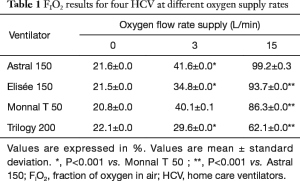
For each given ventilator and condition, the measurements were mostly identical except in two cases with very low variability, namely Monnal T 50 at 3 L/min oxygen flow rate and Astral 150 at 15 L/min flow rate (Table 1). According to our statistical strategy we performed the statistical comparisons between ventilators at these oxygen flow rates and used Monnal T50 and Astral 150 as controls (Table 1). There were no differences between the ventilators when they were supplemented with air (Table 1). Under oxygen supply at 3 L/min flow rate, the FIO2 values delivered with the Astral 150, Elisée 150 and Trilogy 200 were significantly different from those with the Monnal T50. At 15 L/min the values of FIO2 were significantly higher with the Astral 150 than with any other HCV (Table 1).
Full table
Accuracy of VT delivery
Twelve and two experiments were performed for each ventilator for the adult lung configuration (2 VT × 2 PEEP × 3 lung configurations) and for the pediatric lung condition (1 VT × 2 PEEP × 1 lung configuration), respectively. For each given ventilator and every single condition, the measurements were identical, the standard deviation being nil in every instance. Therefore, according to our statistical approach no statistical comparison was performed.
In the adult configurations the Monnal T50 systematically over-delivered VT by more than 10% (Figures 3,4), except for target VT of 500 mL at PEEP 10 (Figure 3). In the normal lung condition the remaining three HCV delivered VT within the 10% accuracy range and these values were very similar to each other. In the obstructive lung condition the Trilogy 200 delivered VT above the 10% upper limit of accuracy whilst the Astral 150 and the Elisée 150 were within the 10% bounds and gave very similar values. For the restrictive lung condition, the three HCV Astral 150, Elisée 150 and Monnal T50 produced similar values. These results were consistent for target VT 300 mL at both PEEP levels (Figure 3). For target VT 500 mL, the VT delivered by the HCV was within the 10% range for accuracy (Figure 3), except for the Monnal T50. The three HCV Astral 150, Elisée 150 and Trilogy 200 gave very similar values.
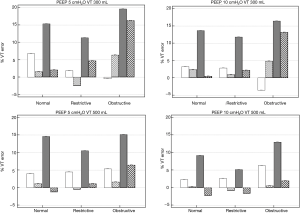
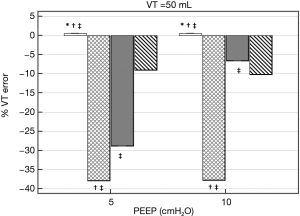
For the pediatric condition, Astral 150 over delivered VT by less than 1% (0.47%±0%). This is in sharp contrast with the VT error found with the other HCV. At PEEP 5, it amounted to −38%±0% for Elisée 150, −29%±0% for Monnal 50 and −9%±0% for Trilogy 200 (Figure 4) (P<0.001 between ventilators by using one-factor ANOVA). The results were essentially the same at PEEP 10, except for the Monnal 50 that felt into the range of accuracy (−7%±0%) and was statistically significantly more accurate than the Trilogy (Figure 4). As can also be seen in Figure 4, the reproducibility of VT from breath to breath was very high.
Discussion
The main findings of the present bench investigation were that the Trilogy 200 and Astral 150 met the 10% standard for VT delivery and the Astral 150, Elisée 150 and Monnal T50 HCV provided the most efficient use of oxygen.
Our hypothesis of very low variability between FIO2 and VT values was verified. Hence, no statistical tests were performed when the standard deviation was nil, and the differences in means were considered as true. It should be mentioned that we used ten consecutive breaths in our analysis. Should a much greater number of breaths has been used some variability may have been present but it is unlikely this would have changed the results.
FIO2
HCV are not equipped with gas blender and, hence most of them have a low-pressure inlet for oxygen supplementation. In present study, the FIO2 values reached at the 15 L/min oxygen rate supply were high, in particular with the Astral 150 and Elisée 150 machines. With the BiPAP synchrony device (18) FIO2 averaged 0.60 at best with a 10 L/min oxygen supply. With the Breathe ventilator, delivered FIO2 ranged from 0.36 to 0.45 (19). In contrast, the portable ventilator LTV 1000 (Pulmonetic systems) delivered FIO2 up to 90% when supplied with oxygen at a 10 L/min flow rate (20). Different factors may influence FIO2 values during non-invasive ventilation (21). Leaks are one of them (22). In the present study we did not investigate the effect of non-intentional leaks on FIO2. The site of oxygen injection also influences the value of FIO2. Dai et al. (18) measured FIO2 at four different oxygen injection locations, i.e., at the ventilator, the humidifier, the mask or the exhalation valve, and found that the closer the site was to the patient, the higher the FIO2. In the present study oxygen supplementation was administered at the rear of the ventilator in each case. The two ventilators that achieved the highest values of FIO2 (Astral 150 and Elisée 150) are made by the same manufacturer, which suggests that the mixing of air and oxygen that comes from the regulation of the corresponding valves is better than for the other ventilators tested. Another possibility is that these ventilators better accommodate the speed of the turbine facing high rate of oxygen supply, however this is more unlikely. The most likely factors contributing to high FIO2 are low bias flow during expiration and control of the oxygen entering the turbine from a reservoir inside the ventilator. This is how the LTV achieves high FIO2. Finally, although high FIO2 can be achieved with turbine ventilators, the stability of FIO2 is not guaranteed as changes in respiratory rate and minute ventilation may influence FIO2 (20). FIO2 with HCV is also influenced by the inspiratory flow rate or inspiratory time of the spontaneous breath because the mixing rate of air and O2 can change with circuit flow. This situation was not explored in the passive setting used in this study. As our study was designed for the bench it allowed us to focus solely on the operational performance of the machine itself.
VT
VT delivery must match the physician’s prescription as closely as possible. As well as the ventilator’s ability to achieve the target VT, gas compression in the ventilator circuit, and gas expansion under increased temperatures may also influence the amount of VT and hence should be properly taken into account by the algorithms (2).
For the adult lung configuration in the present study three ventilators consistently delivered VT within the 10% accuracy range, in almost all instances, namely the Astral 150, Elisée 150 and Trilogy 200. The Monnal T50 systematically departed from the 10% upper bound for accuracy indicating over delivery of VT. The Trilogy 200 was above the 10% upper bound for accuracy in the obstructive lung configuration. In the normal lung condition, the volume error was similar for the Elisée and Trilogy, but lower with the Astral and Monnal ventilators. This comparison holds true for both VT and both PEEP levels. In the obstructive lung configuration, the volume error for the Astral was lower than the Monnal and Trilogy. In the restrictive lung configuration, the volume error for the Astral, Elisée and Trilogy was similar and departed markedly form the Monnal, which over delivered VT. Blakeman et al. compared VT delivery in VC in seven turbine-driven ventilators in a lung model set to 50 mL/cmH2O C and 10 cmH2O/L/s R (23). For a target VT of 400 mL, Trilogy 200 delivered 362 mL on average, which was exactly the same as the VT delivered by this ventilator in present study. These results were obtained in a configuration close to our normal condition so this finding is consistent with the present results. Unfortunately for the purposes of comparison, obstructive and restrictive lung configurations were not used in the study by Blakeman et al. (23). In our study we found that HCV tended to over deliver VT in the obstructive lung as compared to the normal or restrictive lung condition. This was particularly true for target VT of 500 mL. Given the configurations used in our study, it appears that the over delivery of VT in the obstructive lung profile by the HCV may result from higher C. For the pediatric lung configuration, apart from the Astral 150 that delivered VT within less than 1%, the other ventilators systematically delivered VT up to 40% below target. Present results showed that some HCV can achieve very low VT accurately. The importance of lowering VT in patients receiving mechanical ventilation is now largely supported by the evidence, showing improved outcomes as compared to higher VT, not only for patients with ARDS (24) but also for patients with normal lungs both in the ICU (25) and in the operating room for elective surgery (26). Therefore, a ventilator’s ability to accurately deliver VT goes hand in hand with the clinician’s ability to select low VT for the patients under her/his responsibility. When doing so, the clinician must also have complete confidence in the performance of the ventilator used.
In a previous bench study the Trilogy was tested at low target VT (23) and was found to accurately deliver VT For 50 ml target VT, measured VT averaged 51 mL with the Trilogy, a result which is in sharp contrast with the present finding. Two reasons might explain the discrepancy between the two studies. One is the lung model used, as the previous study used the Training Test Lung pneumatic model. The second is that in the study by Blakeman et al. (23) lung C was set to 25 mL/cmH2O (vs. 10 mL/cmH2O in our study) and R to 20 cmH2O/L/s (vs. 50 cmH2O/L/s). We observed in present study that VT error differs significantly across the lung configurations for a given ventilator. This was particularly the case for the Trilogy regarding obstructive lung configuration at VT 300 mL (Figure 3). This finding is a concern as in volume control the ventilator should deliver a target VT, with little variation as specified by the manufacturer. Thus, if there is a noticeable difference, the reasons could be either the followings: (I) the ventilator is not performing as stated by the manufacturers; (II) leaks, which were lacking in our study as discussed below; (III) circuit compensation, which is unlikely because the C of circuit was measured before the experiment for each ventilator, this option was activated during the experiment and the same circuit was used for every ventilator; (IV) accuracy of flow meter used for the working processing in the ventilator; (V) variability across ventilators (we tested at random one specimen); (VI) the difference in pressure generated by the different lung configurations that can impact on the measurement of flow depending on the flowmeter used in each ventilator. To address the issues IV to VI, a specific study should be done.
Limitation and strengths
The main limitation of the present study is that it is a bench study and hence our results cannot be extrapolated to patients. Furthermore, different results might have been obtained if different settings had been used in the lung model. However, the results of present study do support the interest of conducting in vivo investigations in patients. Another limitation is the absence of leak in our experimental set-up. This could be seen as a weakness of present study because results would be different in presence of leaks, either intentional or nonintentional, which limits the generalizability of present findings. This concern applies for VT, FIO2 and also PEEP. In a study on ICU ventilators, Garnier et al. recently found that leaks made less accurate the values of VT and PEEP shown at the ventilator (17). We did not use any leak in our study because we aimed at making the clearest assessment as possible of the accuracy of both FIO2 and VT delivery avoiding any other confounding factor.
Conclusions
The Astral 150, Elisée 150 and Monnal T50 were able to deliver high enough FIO2 than the Trilogy 200. The Astral 150 delivered low VT accurately in the condition of very low lung C and high lung R, Monnal 50 systematically over delivered VT and Trilogy 150 was sensitive to lung configuration when VT was set to 300 mL at either PEEP.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Richard JC, Carlucci A, Breton L, et al. Bench testing of pressure support ventilation with three different generations of ventilators. Intensive Care Med 2002;28:1049-57. [Crossref] [PubMed]
- Carteaux G, Lyazidi A, Cordoba-Izquierdo A, et al. Patient-ventilator asynchrony during noninvasive ventilation: a bench and clinical study. Chest 2012;142:367-76. [Crossref] [PubMed]
- Lofaso F, Brochard L, Hang T, et al. Home versus intensive care pressure support devices. Experimental and clinical comparison. Am J Respir Crit Care Med 1996;153:1591-9. [Crossref] [PubMed]
- Tassaux D, Strasser S, Fonseca S, et al. Comparative bench study of triggering, pressurization, and cycling between the home ventilator VPAP II and three ICU ventilators. Intensive Care Med 2002;28:1254-61. [Crossref] [PubMed]
- Chatburn RL. Which ventilators and modes can be used to deliver noninvasive ventilation? Respir Care 2009;54:85-101. [PubMed]
- Marchese AD, Sulemanji D, Chipman D, et al. Performance of current intensive care unit ventilators during pressure and volume ventilation. Respir Care 2011;56:928-40. [Crossref] [PubMed]
- Chikata Y, Onodera M, Imanaka H, et al. Temperature of gas delivered from ventilators. J Intensive Care 2013;1:6. [Crossref] [PubMed]
- Ogna A, Prigent H, Falaize L, et al. Accuracy of tidal volume delivered by home mechanical ventilation during mouthpiece ventilation: A bench evaluation. Chron Respir Dis 2016. [Epub ahead of print]. [Crossref] [PubMed]
- Nava S, Bruschi C, Fracchia C, et al. Patient-ventilator interaction and inspiratory effort during pressure support ventilation in patients with different pathologies. Eur Respir J 1997;10:177-83. [Crossref] [PubMed]
- Vitacca M, Nava S, Confalonieri M, et al. The appropriate setting of noninvasive pressure support ventilation in stable COPD patients. Chest 2000;118:1286-93. [Crossref] [PubMed]
- Zhou S, Chatburn RL. Effect of the anatomic reservoir on low-flow oxygen delivery via nasal cannula: constant flow versus pulse flow with portable oxygen concentrator. Respir Care 2014;59:1199-209. [Crossref] [PubMed]
- Volsko TA, Hoffman J, Conger A, et al. The effect of targeting scheme on tidal volume delivery during volume control mechanical ventilation. Respir Care 2012;57:1297-304. [Crossref] [PubMed]
- Hutten GJ, van Eykern LA, Latzin P, et al. Relative impact of respiratory muscle activity on tidal flow and end expiratory volume in healthy neonates. Pediatr Pulmonol 2008;43:882-91. [Crossref] [PubMed]
- Hutten GJ, van Eykern LA, Latzin P, et al. Respiratory muscle activity related to flow and lung volume in preterm infants compared with term infants. Pediatr Res 2010;68:339-43. [Crossref] [PubMed]
- Merkus PJ, Arets HG, Joosten T, et al. Measurements of interrupter resistance: reference values for children 3-13 yrs of age. Eur Respir J 2002;20:907-11. [Crossref] [PubMed]
- Gerhardt T, Hehre D, Feller R, et al. Pulmonary mechanics in normal infants and young children during first 5 years of life. Pediatr Pulmonol 1987;3:309-16. [Crossref] [PubMed]
- Garnier M, Quesnel C, Fulgencio JP, et al. Multifaceted bench comparative evaluation of latest intensive care unit ventilators. Br J Anaesth 2015;115:89-98. [Crossref] [PubMed]
- Dai B, Kang J, Yu N, et al. Oxygen injection site affects FIO2 during noninvasive ventilation. Respir Care 2013;58:1630-6. [Crossref] [PubMed]
- Blakeman T, Branson R. Evaluation of a volume targeted NIV device: bench evaluation of the Breathe Technologies non-invasive open ventilation system (NIOV™). COPD 2014;11:568-74. [Crossref] [PubMed]
- Bordes J. FiO2 delivered by a turbine portable ventilator with an oxygen concentrator in an Austere environment. J Emerg Med 2014;47:306-12. [Crossref] [PubMed]
- Samolski D, Antón A, Güell R, et al. Inspired oxygen fraction achieved with a portable ventilator: determinant factors. Respir Med 2006;100:1608-13. [Crossref] [PubMed]
- Goutorbe P, Daranda E, Asencio Y, et al. Leaks can dramatically decrease FiO2 on home ventilators: a bench study. BMC Res Notes 2013;6:282. [Crossref] [PubMed]
- Blakeman TC, Rodriquez D Jr, Hanseman D, et al. Bench evaluation of 7 home-care ventilators. Respir Care 2011;56:1791-8. [Crossref] [PubMed]
- Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. The Acute Respiratory Distress Syndrome Network. N Engl J Med 2000;342:1301-8. [Crossref] [PubMed]
- Serpa Neto A, Nagtzaam L, Schultz MJ. Ventilation with lower tidal volumes for critically ill patients without the acute respiratory distress syndrome: a systematic translational review and meta-analysis. Curr Opin Crit Care 2014;20:25-32. [Crossref] [PubMed]
- Futier E, Constantin JM, Paugam-Burtz C, et al. A trial of intraoperative low-tidal-volume ventilation in abdominal surgery. N Engl J Med 2013;369:428-37. [Crossref] [PubMed]


