Parma tracheostomy technique: a hybrid approach to tracheostomy between classical surgical and percutaneous tracheostomies
Introduction
Tracheostomy (TT) is one of the most common and ancient surgical procedures. The term tracheotomy originates from two Greek words meaning “cutting the trachea” (trachea-tomeo) maybe procedure had known for at least 3000 years (1,2).
Nowadays, there are four main indications for TT:
- Long-term mechanical ventilation;
- Weaning failure;
- Upper airway obstruction;
- Copious secretions.
Absolute contraindication for tracheotomy is skin infection and prior major neck surgery which completely obscures the anatomy (3,4).
Beside surgical classical technique (“open” technique”) in 1985 Ciaglia described the percutaneous dilatational tracheotomy (PDT) (5). This procedure involves making a very small skin incision (1–1.5 cm) and introducing a needle into the trachea through which a J-tipped guide wire is passed. The needle is removed and a guiding catheter is threaded over the J-wire. A subsequent adequate blunt dilatation of the aperture over the J-wire/guiding catheter unit with a series of eight graduated dilators allows the insertion of a preselected TT tube. This entire procedure requires a step by step endoscopic guidance from the beginning to the end and needs a dedicated Kit of instruments for the procedure. The procedure and the kit were updated in 1998 with the introduction of a single, sharply tapered dilator with a hydrophilic coating instead of the eight dilators (Ciaglia Blue Rhino Percutaneous Tracheotomy Introducer Kit; Cook Critical Care Inc. Bloomington, IN, USA) and its last update was the Ciaglia Blue Dolphin Tracheotomy Introducer Kit (Cook Critical Care Inc. Bloomington, IN, USA) in which the dilator is represented by an expansible balloon introduced in soft tissues and in trachea over the guiding catheter and forced to expand for 30 seconds before being removed and replaced by the TT tube. This technique is the most widely used in North America (6).
Other two techniques are also available: the Griggs guide wire dilating forceps (first described in 1990) and the PercuTwist, described by Frova and Quintel in 2002. This two are catheter-based procedures like Ciaglia’s Technique and they require a dedicated Kit and a continuous endoscopic guidance (7,8).
Complications
As every surgical procedure the TT has a series of early and late complications due to the procedural difficulties faced during the procedure or derived from the patient’s anatomy or the patient’s co-morbidities. While early complications are well known by the same physicians who performed the procedure, late complications are difficult to categorise and to quantify, as a lot of patients are critically ill and lost to follow up after discharge (4).
Early complications:
- Haemorrhage;
- Wound infections;
- Subcutaneous emphysema;
- Tube obstruction.
Early tube displacement and/or obstruction defined as a displacement or obstruction of the tube which happened in the first 48 hours after the procedure.
Late complications:
- Swallowing problems;
- Tracheal stenosis;
- Tracheo-Innominate artery fistula (<0.7%);
- Tracheoesophageal fistula;
- Tracheal granulomas formation;
- Persistent stoma;
- Cheloids.
We want to report our experience and our approach to the surgical procedure of TT because we have developed a type of procedure which stands between the classical surgical procedure and the PDT avoiding the “strong” surgical trauma of the first one and costs and dedicated equipment of the latter.
Our TT technique
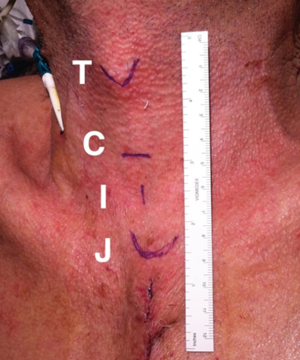
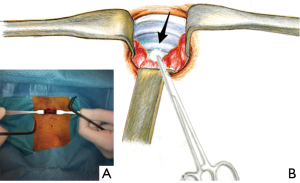
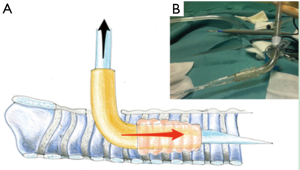
Patient positioning is obtained as in Figure 1. We perform a vertical 1.5 cm incision 1 cm below the cricoid cartilage (Figure 2). The soft tissues are dilated at first with scissors or with a mosquito and then by using two Volkmann’s retractors. Emostasis is obtained by packing the incision with gauzes and the use of electric cautery is not generally required. The thyroid isthmus is generally retracted superiorly or inferiorly even in presence of a pyramidal thyroid lobe (Figure 3) until we obtain the isolation of the trachea at the level of the first and the second tracheal rings. At this time the orotracheal tube is slowly advanced to just below the tracheotomy incision and the balloon cuff is re-expanded allowing the patient’s ventilation during the following steps. The tracheal incision is horizontal and obtained with an 11-number surgical blade between the first and the second tracheal ring, then the incision is gently dilated with a Laborde’s forceps. The endotracheal tube chosen is mounted on a beveled-shaped silicon probe used as a Seldinger’s wire to guide the endotracheal tube in the correct position. When the medical team is ready, the balloon cuff is slightly deflated and the tube is slowly withdrawn by the anaesthetist or by an expert paramedic until it is positioned just above the tracheal incision but not removed. If an urgent re-insertion of the orotracheal tube is required due to difficulties in tracheotomy the orotracheal tube is still ready to be inserted. The tip of the silicone rubber probe is advanced into the trachea until the TT tube is correctly placed (Figure 4). The correct positioning of the tube is controlled by the connection to the mechanical ventilator and the positive control of lung-expansion. At the end the prior orotracheal tube is removed and a short and “superficial” suction is performed though the new tube to check the absence of haemorrhage.
The subsequent management of the TT and the care of the wound are made using the current guidelines about it (4).
In contrast with the Classical Surgical Technique (CST), our technique is a little bit different because:
- The skin incision is about 1 cm shorter and, at the end of the procedure, interrupted skin sutures are not required;
- Isolation of the trachea is obtained by simple separation of tissutal planes without cutting the surrounding structures and the use of electrocautery is general avoided;
- TT is obtained with a linear incision between tracheal rings followed by dilation avoiding fenestration of the trachea and removal of the anterior part of one or more tracheal rings: we prefer this approach because we think that it will avoid post procedural tracheal stenosis once the tracheostomic cannula is removed;
- The use of a silicon probe as a “Seldinger” guide wire prevents the operator to applying an excessive force during cannula insertion and it prevents the cannula to damage the posterior wall of the trachea. The silicon probe is very soft and, even if it is shaped with a sharply peaked tip, we never note tracheal mucosal lesion of the internal tracheal lumen due to the tip of the probe.
In comparison with percutaneous TT techniques we notice that:
- The NMST have the same procedural time than CST and percutaneous method;
- No tracheal hook or other instruments to traction the trachea are required;
- Fibroscopy is not needed;
- The equipement is not disposable and the economic saving is substantial.
Methods
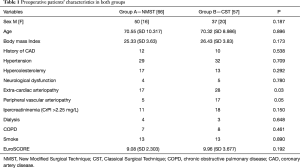
From January 2011 to March 2014 we performed 67 tracheostomies using this New Modified Surgical Technique (NMST) and these patients formed the Group A. The Group B was created collecting clinical data from medical records of 56 patients who underwent the CST from October 2008 to December 2010. TT was performed by four different operators and they were the same in both groups.
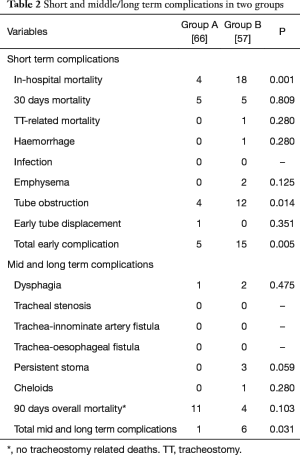
We collected data about early clinical complications (haemorrhage, wound infections, subcutaneous emphysema, tube obstruction, and early tube displacement), deaths TT-related, deaths due to other complications and we phoned the survivors to assess the presence of late TT’s complications (swallowing problems, tracheal stenosis, tracheo-Innominate artery fistula, tracheoesophageal fistula, tracheal granulomas formation, persistent stoma, cheloids).
All data were stored in a SPSS (IMB vs. 21) database used for the statistical analysis.
Categorical data were treated with chi square test and continuous data were treated with t-test for independent samples.
Results
The preoperative patients’ characteristics are shown in Table 1. NMST Group had a significantly lower number of early complication (P=0.005) compared to CST Group (5 vs. 15). In-hospital mortality was significantly higher in CST group (18 deaths vs. 4 in NMST group, P=0.001) and we registered only one case of TT-related mortality in CST group (P=0.280). We did not observe other differences between the two groups regarding short term or mid- long term complications (Table 2).
Full table
Full table
Discussion
Our study showed that our new surgical technique has a comparable safety to the classical surgical technique in terms of mortality and morbidity associated with the procedure.
We found a statistically higher mortality in CST group but it should be noted that the patients in this group had an higher average EuroSCORE value (even if not significant statistically) and a higher number of patients with an extra-cardiac artery disease and peripheral vascular disease (P=0.03 and P=0.05 respectively) than in NMST Group.
Another significant difference was found statistically in the greater number of early tube obstruction in CST (P=0.014). Since the operators have always been the same as with the management protocol of the TT tube the new technique allows an incision a little farther from the manubrium of the sternum keeping the entrance of the cannula into the trachea always between the first and the second tracheal ring ensuring better preservation of the original curvature of the cannula. More important: minimal dissection of tissues ensures a better retention in its location of the tube as you can read in Table 2 there was one case of early tube displacement registered in NMST Group (Group A) but it was due to a wrong tube management during the routine medication.
Moreover, minimal tissue dissection in the NMST group creates minimal bleeding and this reflects, in our opinion, the lower number of early tube obstruction in the NMST group.
Thanks to this new technique the management of accidental removal of the tube is extremely simple and much safer in our experience compared to the classical techniques: it is sufficient to equip a new TT tube with a silicon probe even without shaping it (Figure 4) to reposition the tube avoiding the risk of an incorrect positioning of the tube.
From the economical point of view and in relation to the operating time, the NMST presents no advantages over the classical technique, while it presents certain economic advantages over percutaneous techniques as it avoids the use of the endoscope of a dedicated cannula and of dedicated systems of dilation.
The use of the silicon probe, furthermore, minimises the possibility of injuring the posterior wall of the trachea. In our series of operated patients using the conventional technique we had one death due to the development of a massive mediastinal pneumothorax owing to a difficult and forced positioning of the TT tube while this possibility is extremely rare with the NMST.
It is interesting that overall medium and long term complications between the two groups show a significant lower number of complications in the NMST group and, in our opinion, this is correlate to the minimized surgical trauma of the NMST. However it is worth noting that the sample is still small and, moreover, the 90-day mortality is affected more than other things by the overall clinical condition of the patient and not so much by the TT procedure itself.
All the complications related to the CST are present in Group B while no one can be detected in group A (persistent stoma n=3, Keloids n=1) so we might infer that the NMST has also a better aesthetic impact during the rehabilitation period of these patients.
Conclusions
In our experience the NMST has demonstrated to be easy and reproducible with a short learning curve and a minor surgical trauma. Major and minor complications appear to be lower than the CST and this last evidence led us to use this technique as the leading technique in our Intensive Care Unit to perform TT. We mean to make additional evaluation on larger numbers of patients but our view is that this technique may fit between the classical surgical and percutaneous systems avoiding the trauma of the first and the costs of the second.
Acknowledgements
We thank Mr. Arnaldo Molardi for the beautiful colour illustrations which he painted for this paper and Mrs. Maria Rosa Annetta Pelizzoni, English teacher, for her help and assistance in the revision of the manuscript.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by Regional Ethics Committee board of University of Parma (Protocol No. 28600) and all data were obtained from the registry of our current clinical practice, but the requirement for the individual patient consent was waived because of the retrospective design of the study and because data were collected from routine care. All data were anonymized and de-identified prior to statistical analysis. The protocol of the study is in accordance with the declaration of Helsinki.
References
- Frost EA. Tracing the tracheostomy. Ann Otol Rhinol Laryngol 1976;85:618-24. [Crossref] [PubMed]
- Goldenberg D, Ari EG, Golz A, et al. Tracheotomy complications: a retrospective study of 1130 cases. Otolaryngol Head Neck Surg 2000;123:495-500. [Crossref] [PubMed]
- McClelland RM. Tracheostomy: its management and alternatives. Proc R Soc Med 1972;65:401-4. [PubMed]
- De Leyn P, Bedert L, Delcroix M, et al. Tracheotomy: clinical review and guidelines. Eur J Cardiothorac Surg 2007;32:412-21. [Crossref] [PubMed]
- Ciaglia P, Firsching R, Syniec C. Elective percutaneous dilatational tracheostomy. A new simple bedside procedure; preliminary report. Chest 1985;87:715-9. [Crossref] [PubMed]
- Kost KM. Endoscopic percutaneous dilatational tracheotomy: a prospective evaluation of 500 consecutive cases. Laryngoscope 2005;115:1-30. [Crossref] [PubMed]
- Griggs WM, Worthley LI, Gilligan JE, et al. A simple percutaneous tracheostomy technique. Surg Gynecol Obstet 1990;170:543-5. [PubMed]
- Frova G, Quintel M. A new simple method for percutaneous tracheostomy: controlled rotating dilation. A preliminary report. Intensive Care Med 2002;28:299-303. [Crossref] [PubMed]


