Review of tracheobronchial foreign body aspiration in the South African paediatric age group
Introduction
Children, and in particular the very young, are the most vulnerable for aspiration and ingestion of foreign bodies (FBs) (1).
Although the spectrum of FBs varies from country to country, depending on the diet and customs of the population, the most common foreign body aspiration (FBA) causing injuries are from diminutive food items (2). Case reports, cases series and data emanating from death certificates testify that nuts and seeds could represent an earnest threat being not only the most documented FB, but also frequently involved in cases presenting with complications and requiring hospitalization (3).
Aspiration of a FB into the air passages conventionally occurs in older infants and toddlers. Boys are affected more than girls in a ratio of 2:1 (4).
FBA is a prevalent cause of pathology in children, particular in those younger under 3 years of age. It has been estimated that in the year 2000, FBs, either ingested and/or aspirated were responsible for over 17,000 visits to health facilities of children under the age of 15 in North America (5).
While the mortality has been typically high in previous centuries, (almost a quarter of all cases), with the advance of modern bronchoscopy techniques, current mortality has significantly declined over the last 25 years (6).
It has been estimated that the vast majority of FB aspiration takes place in children under the age of 4, while the peak incidence seems to occur between the age of 12 and 24 months (7-14). These children can move around and are able and prone to explore the outside world with their mouth, putting any object they can get hold of within their mouth, while they still lack proper molars to grind objects to smaller (and less dangerous) pieces.
Other predisposing factors for FBA at this young age include access to unsuitable foods or tiny objects, all kinds of other active behaviour while eating. Above all, children are far more vulnerable to aspiration of a FB due to the small diameter of their airway, prone to easily be obstructed (15). In adolescents and adults, neurodevelopmental delays (16), low level of consciousness, and drugs and alcohol will increase the risk of FBA (17).
In paediatrics, commonly aspirated FBs are nuts, victual particles, equipment, and parts or bits of toys, peanuts (36–55% of FBs aspirations in civilized countries), seeds and popcorn (9-11,13,14).
Aliment parts are the most widely recognized objects aspirated by newborns and babies, while non-food particles as pins and coins are mostly present in elder kids (2,18-20). Inflatables toys or other objects (e.g., inflated gloves or condoms) are the most prevalent objects in lethal FBAs (15).
Factors that make FBs more perilous include roundness (round objects are most liable to cause consummate airway obstruction and asphyxiation), failure to break asunder facilely, compressibility, and smooth, slippery surface (15). The effects of tablet aspiration depend on the properties of the medication. Certain medications such as iron or potassium may dissolve in the airways and cause excruciating inflammation and eventually stenosis, so early diagnosis and timely extraction is consequential to minimize long-term consequences (21,22).
The majority of FBAs in children are located in the bronchi (7,11,23). Laryngeal and tracheal FBs are less common. In a large case series of FBA aspirations in children, the sites of the FB are shown in Table 1 (7).
Full table
Although most aspirated FBs are located in the bronchi, sizably voluminous, bulky FBs (e.g., aliment), or those with sharp, aberrant edges may also become lodged in the larynx (11,24). This is particularly prevalent in infants younger than one year. Tracheal narrowing or impotent respiratory effort may predispose to tracheal FB (11). Compared with bronchial FBs, laryngo-tracheal FBs are associated with incremented morbidity and mortality (24,25).
Clinical presentation
Youngsters frequently move and giggle while they are eating and don’t focus on masticating or gulping. In addition, the neurological-motor mechanism controlling swallowing may also be still underdeveloped, disqualifying it to give appropriate control to eschew nourishments or different materials to enter air passages.
Roughly 75% of upper airways FBs in the children happen in kids less than 3 years. Most FBs are sufficiently small to pass to the trachea.
Because of the wide calibre of the trachea contrasted with the cricoid cartilage, only few FBs lodge within the trachea. Consequently most FBs will pass through the trachea to lodge within the bronchi.
In children less than 5 years, non-food particles are less common than food particles, while in elder children non-food particles dominate.
A detailed history and a thorough clinical examination are very important in assessing children that potentially aspirated a FB (26).
It is not uncommon following aspiration of a FB that a “silent era” to occur. Only when time progresses, the FM may cause erosion and/or inflammation. This condition could be accompanied by fever, cough discomfort and haemoptysis. Serious lung infections may develop later (4,26).
The signs and symptoms of FBA vary according to the location of the FB (27,28) (Table 2).

Full table
Delayed diagnosis—patients who present days or weeks after the aspiration often develop symptoms due to complications cognate to the presence of the FB, such as infection and inflammation of the airway. Thus, they may present with fever and other signs and symptoms of pneumonia. In the absence of a history of choking, FBA may not be suspected. These patients with occult FBA may amend with antibiotic therapy. However, the infiltrate on chest radiograph customarily does not resolve, and recurrence of pneumonia is common.
One reason for delay in diagnosis is that children with lower airway FBs may present with subtle or nonspecific symptoms (30). As a result, they may come to medical attention only when they develop dyspnoea, wheezing, chronic cough, or recurrent pneumonia (31).
Other factors contributing to diagnostic delay include unwitnessed aspiration, a decision by the parents or physician not to pursue evaluation once the acute choking episode has resolved, and misinterpretation of symptoms as evidence fortifying the diagnosis of de novo pneumonia, asthma or asthma exacerbation, or bronchiolitis (11,30,32).
Life-threatening FBA—if a child presents with consummate airway obstruction (i.e., is unable to verbalize or cough), dislodgement utilizing back blows and chest compressions in infants, and the Heimlich manoeuvre in older children, should be endeavoured. In contrast, these interventions should be eschewed in children who are able to talk or cough since they may convert a partial to a consummate obstruction (11). For the same reason “blind” sweeping of the mouth should be evaded.
The recommendations of the American Heart Sodality (AHA) regarding interventions for choking represent the standard in acute life-threatening events (33).
Diagnosis
Posteroanterior and lateral chest radiographs (Figure 1) are acquired to assess a youngster suspected of FB aspiration. Posteroanterior and lateral neck radiographs are subsidiary for distinguishing tracheal radiopaque particles. Chest radiographs on respiration can be of use. Expiratory radiographs can demonstrate air which caught underneath the obstacle, bringing about emphysema of the included part; contralateral shift of the mediastinum can also be seen.

Radiographs may demonstrate any other inflammatory lung problems. In any case, endoscopy remains the gold standard for both discovery of FBs and treatment by extraction (4,26). Flexible rather than rigid bronchoscopy may be utilized for diagnostic purposes in cases in which the diagnosis is obscure, or if the FBA is known but the location of the object is obscure (34).
Plain radiographic evaluation of the chest may or may not be helpful in establishing the diagnosis of FBA, depending upon whether the object is radio-opaque, and whether and to what degree airway obstruction is present. The diagnosis of FBA is readily established with plain radiographs when the object is radio-opaque (only about 10% of FBs). However, most objects aspirated by children are radiolucent (e.g., nuts, aliment particles) (35), and are not detected with standard radiographs unless aspiration is accompanied by airway obstruction or other complications (7,35-37). As a result, common findings on radiography do not rule out FBA, and the clinical history is the main determinant of whether to perform a bronchoscopy (38).
In children with lower airway FBA, the most prevalent radiographic findings are listed in Table 3 (27,28,41,42).

Full table
The chest radiograph is normal in at least 30% of cases (7,41,43). The sensitivity of chest films has been reported to be between 68% and 76%, and the specificity between 45% and 67% when evaluating for FBs in the airway (44). Ideally, both inspiratory and expiratory radiographs should be obtained, if this is possible, because this may increase the sensitivity for detecting a radiolucent FB.
In adolescent children in whom it is arduous to obtain expiratory radiographs (either because they are tachypneic or because they cannot cooperate), left decubitus films may simulate expiratory radiographs. However, two retrospective studies suggested that these films did not integrate diagnostic value, at least as routinely performed (45,46).
If a laryngotracheal FB is suspected predicated on symptoms (stridor, wheeze, and dyspnoea, and sometimes hoarseness) a neck radiograph should be performed. These should include posteroanterior and lateral views, with the arms and shoulders situated inferiorly and posteriorly to optimize the image of the larynx and trachea. Even if the FB is radiolucent, these films may suggest the diagnosis if they show a subglottic density or swelling (25).
CT is a possible diagnostic option for patients who are asymptomatic or symptomatic but stable, who have normal or inconclusive plain radiographs but a perpetual clinical suspicion of FB aspiration. However, this imaging is only subsidiary if the provider judges that negative imaging would be adequate to preclude bronchoscopy (47,48).
Treatment
An emergency endoscopy is obligatory in critical situations. After the patient is anaesthetised in recumbent position the neck should be gently extended. We advocate the use a laryngoscope to also inspect the larynx as part of the bronchoscopy.
The ventilating endoscope is than carefully introduced into the trachea, while ventilation continues. All air passages are carefully examined, and the FB abstracted through or with the bronchoscope.
FB extraction will fail with bad vision or sometimes when fragmented particles have moved more distally. These are sometimes amenable for extraction utilising a Fogarty catheter. In very rare cases more drastic procedures may be require such as bronchotomy or resection of the lung.
Corticosteroids or bronchodilators may be indicated to decrease oedema. Adrenaline can also be useful in certain circumstances. Chest radiographs are mandatory in the follow-up for the identification of pneumothorax and/or air in the mediastinum following FB extraction (4,26).
FB extraction
If FBA is known to have occurred or is vigorously suspected, rigid bronchoscopy is the procedure of choice to identify and extract the object (29,34,49). Rigid bronchoscopy sanctions control of the airway, good visualization, manipulation of the object with a wide variety of forceps, and yare management of mucosal haemorrhage (20,50-52).
Bronchoscopy is successful in extracting the FB in approximately 95% of cases, with a very low complication rate of less than 1% (7,53,54). Thoracotomy is rarely indicated in those cases in which FBs can be visualized but cannot be extracted by means of a rigid bronchoscope.
FB extraction should be performed by an experienced operator to minimize the jeopardy of complications. Unsuccessful attempts to remove the FB may push it into a distal position, making them more arduous to retrieve. Disintegration or dislodgement of all or part of the FB, or a fragment of the FB, into the main bronchus of the contralateral lung are potentially lethal complications if the pristinely involved bronchus remains obstructed by inflammation or residual FB (55). Major complications of FB extraction include pneumothorax, hemorrhage, and respiratory apprehend, but they occur infrequently.
Alternatively, flexible (rather than rigid) bronchoscopy is utilized to extract the FB in some centers with experience in this technique (28,51,56,57). This technique customarily is circumscribed to older adolescents or adolescent adults. Potential advantages of utilizing flexible bronchoscopy for FB extraction are avoidance of general anaesthesia and the facility to reach sub-segmental bronchi.
In a large case series, the FB was successfully extracted by flexible bronchoscopy in 91% of patients (28). The main disadvantage of flexible bronchoscopy for FB abstraction is the peril of dislodging the FB and further compromising the airway. Because of these concerns, the American Thoracic Society (ATS) states, “In general, rigid instruments are superior for detailed anatomic assessment of the larynx and cervical trachea and for operative manipulation, principally foreign body extraction” (52). Flexible bronchoscopy is commonly utilized by most centers for management of FBA in adults.
If there is a suspicion for multiple diminutive FBs or fragments, we recommend performing a flexible bronchoscopy after FB abstraction, to evaluate the entire tracheobronchial tree (31,58).
Complications
When FBA is diagnosed soon after the event, there is customarily little damage to the airway or lung parenchyma. The longer the FB is retained, the more likely are complications (e.g., atelectasis, post-obstructive pneumonia). A FB that causes chronic or recurrent distal infection may lead to bronchiectasis (31,39,40,59,60). This complication should be treated after the FB is abstracted. Cultures obtained during bronchoscopy guide the initial antibiotic cull in treating infected areas of bronchiectasis. Failure to promptly diagnose the FBA may additionally cause complications from the utilization of non-indicated treatments, such as steroids, antibiotics, or bronchodilators (61,62).
Prevention
As a general rule, primary passive intervention strategies to reduce the jeopardy of FBA (e.g., legislation that eliminates choking hazards from the market) are more efficacious than active intervention strategies (strategies that require constant parental supervision) (63).
Materials and methods; experience of trauma unit in Red Cross War Memorial Children’s Hospital, University of Cape Town
All data were recorded for every patient since 1991. All patients were treated according to the unit’s management protocol (Figure 2).
Results
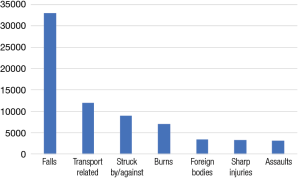
A total retrospective study was performed on 88,822 children who attended the trauma unit from January 1991 till December 2000. Fall from a height was the commonest trauma (n=32,766) 21%, transportation traumas (n=11,915) 13%, Burns (n=7,241) 8%, struck by objects (n=9,064) 10%, FBs (n=3,677) 4%, sharp objects (n=3,601) 4% and assault (n=3,302) 4% (Figure 3). Three-hundred and forty [340] patients were analysed in more detail.
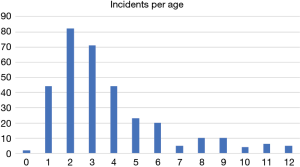
Genders were similarly influenced. Ages went somewhere around 0 and 12 years, in spite of the fact that there was only one kid less than 1 year, at 2 years of age rate increased dramatically, with 25% of all cases happening (Figure 4).
Details of aspirated or ingested FBs
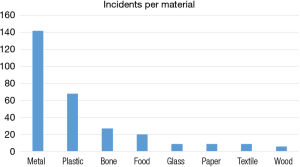
Most of them were of metallic nature (44%) or made of plastic (21%) (Figure 5).
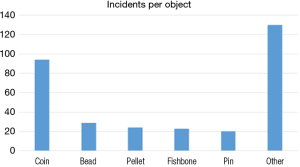
Coins were the most common FB (30%), bead (8%) and pellet (7%), (Figure 6). Diameter was 0.1–3 cm.
Anatomical region affected
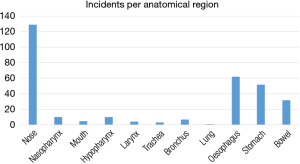
Nose (129 cases or 41%), followed by the oesophagus (64 cases or 20%), Stomach (52 cases or 17%) and bowel (32 cases or 10%). Other anatomical sites included nasopharynx (11 cases or 4%), Hypopharynx (10 cases or 3%), bronchus (6 cases or 2%), oral cavity (4 cases or 1.3%), larynx (3 cases or 1%), trachea (2 cases or 0.7%) and lung (1 case or 0.3%) (Figure 7).
Severity of symptoms
Case were rated utilising the Abbreviated Injury Score (AIS). We found that 0.6% of conditions were severe, 14% were moderate and 49% were mild. Thirty six percent was asymptomatic.
Retrieval of FBs
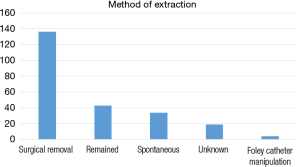
Fifty-seven per cent (57%) of FBs were extracted by surgical means, 19% left in place, 14% spontaneously came out and 1% extracted by Foley’s catheter (Figure 8).
Regarding the most vulnerable age for aspiration, the difference according to sex was studied. Where girls are susceptible from an early age (3.0 years), they are only at risk for a relatively brief period (3.0 to 3.9 years), a period of approximately 10 months (P=0.023). However, boys are susceptible at a later age (3.7 years), but remain at risk for a far longer duration (3.7 to 5.1 years) or a period of approximately 15 months.
Discussion
Trauma represents a very important part of mortality and morbidity worldwide with disregard to age and sex. Road traffic crashes, falls from heights and interpersonal violence are among the fundamental drivers of harm related disability and death (64).
Traditionally, trauma was viewed as unpreventable and only recently has been perceived as avoidable (65,66).
Childsafe South Africa’s (CSA’s) database was used as the fundamental hotspot for investigation of ingestion and aspiration trauma conditions experienced in Cape Town. Over the last 25 years we have been prospectively collecting data on all childhood injuries utilizing a constant data sheet.
There have been relatively few reports on FB ingestion and aspiration from Africa. Several reports indicate the predominance of peanuts as the aspirated FB (67,68). Where most reports indicate a low morbidity, some report a high mortality (11%) of children aspirating a FB (69). In Durban (South Africa), three children died after aspirating parts of a ballpoint pen (70).
There have been attempts to correlate the size of the ingested object with the anatomical location of impaction (71). Nearly all reports on FB ingestion show a predominance of boys (about two-thirds of all patients).
The presentation of a child with aspiration can vary greatly (e.g., in many series, less than 50% present with the history of aspiration) and the diagnosis might be difficult. However, most children present with coughing (approximately 80%), dyspnoea (approximately 70%), have abnormal auscultation (approximately 75%), or abnormal radiographs of the lateral cervical spine (soft tissue) or chest (approximately 60%).
FBs aspiration and ingestion is the fifth most common indication for admissions to our unit. In our review the rate of severe adverse outcome was very low (only 0.4%); this may be a result of transport issues in our environment. Seriously injured patients may have given up amid the long duration of transportation and we are currently gathering information on this issue.
Coins were the commonest ingested or aspirated FBs. It might be due to shortage of toys in our communities. FBs lodged in the nose were more common than in the oesophagus. Most FBs were extracted in the operating room with the patient anaesthetized, by method for oesophagoscopy. FB’s that either reached the stomach or were left alone and passed all through the GIT tract without further complications.
Although it is generally known that boys are at higher risk than girls, no detailed information is usually provided regarding prevention. An analysis was performed on the exact age for both sexes. Comparing the box and whisker diagrams of both sexes, there is a good overlap between the medians of both groups.
However, the 95% intervals calculated with the means indicate that there is a gap between the average ages of both groups susceptible for ingestion of FBs. Where girls are susceptible from an early age (3.0 years), they are only at risk for a shorter period (3.0 to 3.9 years), a period of approximately 10 months (P=0.023). However, boys are susceptible at a later age (3.7 years), but remain at risk for a far longer duration (3.7 to 5.1 years) or a period of approximately 15 months.
The results of this study confirm the frequent occurrence of FBs ingestion and aspiration in paediatrics and have implications for preventive measures. Parents of children should be educated about the specific period in which their child is most susceptible for the ingestion and aspiration of a FB, and preventive programmes should also be aimed at preschool children (e.g., minimising young children’s access to metal coins).
Conclusions
Ingestion or aspiration of FBs is very common in paediatric age group. Coins were the commonest aspirated FBs in South Africa. On the premise of this study we firmly advice parents and caregivers to keep coins far from kids, particularly youngsters less than 6 years old. We used the results of this study in our programs for prevention.
Acknowledgements
The authors would like to thank Childsafe South Africa for kindly providing the statistics.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Rothmann BF, Boeckman CR. Foreign bodies in the larynx and tracheobronchial tree in children. A review of 225 cases. Ann Otol Rhinol Laryngol 1980;89:434-6. [Crossref] [PubMed]
- Rimell FL, Thome A Jr, Stool S, et al. Characteristics of objects that cause choking in children. JAMA 1995;274:1763-6. [Crossref] [PubMed]
- Tander B, Kirdar B, Aritürk E, et al. Why nut? The aspiration of hazelnuts has become a public health problem among small children in the central and eastern Black Sea regions of Turkey. Pediatr Surg Int 2004;20:502-4. [PubMed]
- Roddenbery SA, Reynolds M, Adolph V. Foreign Bodies in the Air Passages and Esophagus. In: Arensman RM, Bambini DA, Almond PS, et al. editors. Pediatric Surgery. 2nd Ed. Austin, Texas: Landes Bioscience, 2009:341-5. Available online: https://www.scribd.com/document/253422759/Pediatric-Surgery-pdf
- Centers for Disease Control and Prevention (CDC). Nonfatal choking-related episodes among children--United States, 2001. MMWR Morb Mortal Wkly Rep 2002;51:945-8. [PubMed]
- Kramer TA, Riding KH, Salkeld LJ. Tracheobronchial and esophageal foreign bodies in the pediatric population. J Otolaryngol 1986;15:355-8. [PubMed]
- Eren S, Balci AE, Dikici B, et al. Foreign body aspiration in children: experience of 1160 cases. Ann Trop Paediatr 2003;23:31-7. [Crossref] [PubMed]
- Burton EM, Brick WG, Hall JD, et al. Tracheobronchial foreign body aspiration in children. South Med J 1996;89:195-8. [Crossref] [PubMed]
- Mu L, He P, Sun D. Inhalation of foreign bodies in Chinese children: a review of 400 cases. Laryngoscope 1991;101:657-60. [Crossref] [PubMed]
- Schmidt H, Manegold BC. Foreign body aspiration in children. Surg Endosc 2000;14:644-8. [Crossref] [PubMed]
- Tan HK, Brown K, McGill T, et al. Airway foreign bodies (FB): a 10-year review. Int J Pediatr Otorhinolaryngol 2000;56:91-9. [Crossref] [PubMed]
- Ciftci AO, Bingöl-Koloğlu M, Senocak ME, et al. Bronchoscopy for evaluation of foreign body aspiration in children. J Pediatr Surg 2003;38:1170-6. [Crossref] [PubMed]
- Chapin MM, Rochette LM, Annest JL, et al. Nonfatal choking on food among children 14 years or younger in the United States, 2001-2009. Pediatrics 2013;132:275-81. [Crossref] [PubMed]
- Altkorn R, Chen X, Milkovich S, et al. Fatal and non-fatal food injuries among children (aged 0-14 years). Int J Pediatr Otorhinolaryngol 2008;72:1041-6. [Crossref] [PubMed]
- Committee on Injury, Violence, and Poison Prevention. Prevention of choking among children. Pediatrics 2010;125:601-7. [Crossref] [PubMed]
- DeRowe A, Massick D, Beste DJ. Clinical characteristics of aero-digestive foreign bodies in neurologically impaired children. Int J Pediatr Otorhinolaryngol 2002;62:243-8. [Crossref] [PubMed]
- Wolkove N, Kreisman H, Cohen C, et al. Occult foreign-body aspiration in adults. JAMA 1982;248:1350-2. [Crossref] [PubMed]
- Fitzpatrick PC, Guarisco JL. Pediatric airway foreign bodies. J La State Med Soc 1998;150:138-41. [PubMed]
- Lemberg PS, Darrow DH, Holinger LD. Aerodigestive tract foreign bodies in the older child and adolescent. Ann Otol Rhinol Laryngol 1996;105:267-71. [Crossref] [PubMed]
- Jiaqiang S, Jingwu S, Yanming H, et al. Rigid bronchoscopy for inhaled pen caps in children. J Pediatr Surg 2009;44:1708-11. [Crossref] [PubMed]
- Küpeli E, Khemasuwan D, Lee P, et al. "Pills" and the air passages. Chest 2013;144:651-60. [Crossref] [PubMed]
- Kinsey CM, Folch E, Majid A, et al. Evaluation and management of pill aspiration: case discussion and review of the literature. Chest 2013;143:1791-5. [Crossref] [PubMed]
- Black RE, Johnson DG, Matlak ME. Bronchoscopic removal of aspirated foreign bodies in children. J Pediatr Surg 1994;29:682-4. [Crossref] [PubMed]
- Lima JA. Laryngeal foreign bodies in children: a persistent, life-threatening problem. Laryngoscope 1989;99:415-20. [Crossref] [PubMed]
- Esclamado RM, Richardson MA. Laryngotracheal foreign bodies in children. A comparison with bronchial foreign bodies. Am J Dis Child 1987;141:259-62. [Crossref] [PubMed]
- Nguyen LT. Foreign Bodies. In: Puri P, Höllwarth ME. editors. Pediatric Surgery: Diagnosis and Management. Springer-Verlag Berlin Heidelberg, 2009:207-9.
- Zhijun C, Fugao Z, Niankai Z, et al. Therapeutic experience from 1428 patients with pediatric tracheobronchial foreign body. J Pediatr Surg 2008;43:718-21. [Crossref] [PubMed]
- Tang LF, Xu YC, Wang YS, et al. Airway foreign body removal by flexible bronchoscopy: experience with 1027 children during 2000-2008. World J Pediatr 2009;5:191-5. [Crossref] [PubMed]
- Laks Y, Barzilay Z. Foreign body aspiration in childhood. Pediatr Emerg Care 1988;4:102-6. [Crossref] [PubMed]
- Mu L, He P, Sun D. The causes and complications of late diagnosis of foreign body aspiration in children. Report of 210 cases. Arch Otolaryngol Head Neck Surg 1991;117:876-9. [Crossref] [PubMed]
- Blazer S, Naveh Y, Friedman A. Foreign body in the airway. A review of 200 cases. Am J Dis Child 1980;134:68-71. [Crossref] [PubMed]
- Kugelman A, Shaoul R, Goldsher M, et al. Persistent cough and failure to thrive: a presentation of foreign body aspiration in a child with asthma. Pediatrics 2006;117:e1057-60. [Crossref] [PubMed]
- American Heart Association. BLS for Healthcare Providers. p.163.
- Martinot A, Closset M, Marquette CH, et al. Indications for flexible versus rigid bronchoscopy in children with suspected foreign-body aspiration. Am J Respir Crit Care Med 1997;155:1676-9. [Crossref] [PubMed]
- Mu LC, Sun DQ, He P. Radiological diagnosis of aspirated foreign bodies in children: review of 343 cases. J Laryngol Otol 1990;104:778-82. [Crossref] [PubMed]
- Zerella JT, Dimler M, McGill LC, et al. Foreign body aspiration in children: value of radiography and complications of bronchoscopy. J Pediatr Surg 1998;33:1651-4. [Crossref] [PubMed]
- Tokar B, Ozkan R, Ilhan H. Tracheobronchial foreign bodies in children: importance of accurate history and plain chest radiography in delayed presentation. Clin Radiol 2004;59:609-15. [Crossref] [PubMed]
- Mortellaro VE, Iqbal C, Fu R, et al. Predictors of radiolucent foreign body aspiration. J Pediatr Surg 2013;48:1867-70. [Crossref] [PubMed]
- Denney MK, Berkas EM, Snider TH, et al. Foreign body bronchiectasis. Dis Chest 1968;53:613-6. [Crossref] [PubMed]
- al-Majed SA, Ashour M, al-Mobeireek AF, et al. Overlooked inhaled foreign bodies: late sequelae and the likelihood of recovery. Respir Med 1997;91:293-6. [Crossref] [PubMed]
- Sahin A, Meteroglu F, Eren S, et al. Inhalation of foreign bodies in children: experience of 22 years. J Trauma Acute Care Surg 2013;74:658-63. [Crossref] [PubMed]
- Boufersaoui A, Smati L, Benhalla KN, et al. Foreign body aspiration in children: experience from 2624 patients. Int J Pediatr Otorhinolaryngol 2013;77:1683-8. [Crossref] [PubMed]
- Even L, Heno N, Talmon Y, et al. Diagnostic evaluation of foreign body aspiration in children: a prospective study. J Pediatr Surg 2005;40:1122-7. [Crossref] [PubMed]
- Svedström E, Puhakka H, Kero P. How accurate is chest radiography in the diagnosis of tracheobronchial foreign bodies in children? Pediatr Radiol 1989;19:520-2. [Crossref] [PubMed]
- Assefa D, Amin N, Stringel G, et al. Use of decubitus radiographs in the diagnosis of foreign body aspiration in young children. Pediatr Emerg Care 2007;23:154-7. [Crossref] [PubMed]
- Brown JC, Chapman T, Klein EJ, et al. The utility of adding expiratory or decubitus chest radiographs to the radiographic evaluation of suspected pediatric airway foreign bodies. Ann Emerg Med 2013;61:19-26. [Crossref] [PubMed]
- Lee EY, Greenberg SB, Boiselle PM. Multidetector computed tomography of pediatric large airway diseases: state-of-the-art. Radiol Clin North Am 2011;49:869-93. [Crossref] [PubMed]
- Yang C, Hua R, Xu K, et al. The role of 3D computed tomography (CT) imaging in the diagnosis of foreign body aspiration in children. Eur Rev Med Pharmacol Sci 2015;19:265-73. [PubMed]
- Divisi D, Di Tommaso S, Garramone M, et al. Foreign bodies aspirated in children: role of bronchoscopy. Thorac Cardiovasc Surg 2007;55:249-52. [Crossref] [PubMed]
- Paşaoğlu I, Doğan R, Demircin M, et al. Bronchoscopic removal of foreign bodies in children: retrospective analysis of 822 cases. Thorac Cardiovasc Surg 1991;39:95-8. [Crossref] [PubMed]
- Wood RE, Gauderer MW. Flexible fiberoptic bronchoscopy in the management of tracheobronchial foreign bodies in children: the value of a combined approach with open tube bronchoscopy. J Pediatr Surg 1984;19:693-8. [Crossref] [PubMed]
- Faro A, Wood RE, Schechter MS, et al. Official American Thoracic Society technical standards: flexible airway endoscopy in children. Am J Respir Crit Care Med 2015;191:1066-80. [Crossref] [PubMed]
- Rovin JD, Rodgers BM. Pediatric foreign body aspiration. Pediatr Rev 2000;21:86-90. [Crossref] [PubMed]
- Sersar SI, Rizk WH, Bilal M, et al. Inhaled foreign bodies: presentation, management and value of history and plain chest radiography in delayed presentation. Otolaryngol Head Neck Surg 2006;134:92-9. [Crossref] [PubMed]
- Pawar DK. Dislodgement of bronchial foreign body during retrieval in children. Paediatr Anaesth 2000;10:333-5. [Crossref] [PubMed]
- Swanson KL, Prakash UB, Midthun DE, et al. Flexible bronchoscopic management of airway foreign bodies in children. Chest 2002;121:1695-700. [Crossref] [PubMed]
- Ramírez-Figueroa JL, Gochicoa-Rangel LG, Ramírez-San Juan DH, et al. Foreign body removal by flexible fiberoptic bronchoscopy in infants and children. Pediatr Pulmonol 2005;40:392-7. [Crossref] [PubMed]
- McGuirt WF, Holmes KD, Feehs R, et al. Tracheobronchial foreign bodies. Laryngoscope 1988;98:615-8. [Crossref] [PubMed]
- Cataneo AJ, Reibscheid SM, Ruiz Júnior RL, et al. Foreign body in the tracheobronchial tree. Clin Pediatr (Phila) 1997;36:701-6. [Crossref] [PubMed]
- Jackson, C, Jackson, CL. Diseases of the air and food passages of foreign body origin. Philadelphia: WB Saunders, 1936:135.
- Louie MC, Bradin S. Foreign body ingestion and aspiration. Pediatr Rev 2009;30:295-301, quiz 301. [Crossref] [PubMed]
- Chung MK, Jeong HS, Ahn KM, et al. Pulmonary recovery after rigid bronchoscopic retrieval of airway foreign body. Laryngoscope 2007;117:303-7. [Crossref] [PubMed]
- Baker SP. Childhood injuries: the community approach to prevention. J Public Health Policy 1981;2:235-46. [Crossref] [PubMed]
- Sharma GK, Krug EG, Lozano R. A leading cause of the burden of disease. International journal on Injury Control and Safety Promotion 2000;7:261-7. [Crossref]
- Committee on Trauma Research, Commission on Life Sciences, National Research Council and Institute of Medicine. Injury in America: a continuing public health problem. Washington, DC: National Academic Press, 1985.
- Mercy JA, Rosenberg ML, Powell KE, et al. Public health policy for preventing violence. Health Aff (Millwood) 1993;12:7-29. [Crossref] [PubMed]
- Agarwal RK, Banerjee G, Shembish N, et al. Foreign bodies in the tracheobronchial tree: a review of 102 cases in Benghazi, Libya. Ann Trop Paediatr 1988;8:213-6. [Crossref] [PubMed]
- Sissokho B, Conessa C, Petrognani R. Rigid endoscopy and laryngo-tracheo-bronchial foreign bodies in children: observations apropos of 200 endoscopies conducted in a tropical setting. Med Trop (Mars) 1999;59:61-7. [PubMed]
- Melaku G. Foreign body aspiration in children: experience from Ethiopia. East Afr Med J 1996;73:459-62. [PubMed]
- Bhana BD, Gunaselvam JG, Dada MA. Mechanical airway obstruction caused by accidental aspiration of part of a ballpoint pen. Am J Forensic Med Pathol 2000;21:362-5. [Crossref] [PubMed]
- Bhatia PL. Problems in the management of aspirated foreign bodies. West Afr J Med 1991;10:158-67. [PubMed]