Focusing on spontaneous coronary artery dissection: actuality and future perspectives
Current ESC Guidelines on Acute Coronary Syndromes (ACS) declare that up to 20% of patients have no lesions or non-obstructive lesions of epicardial coronary arteries (1). When angiograms are silent, a spontaneous coronary artery dissection (SCAD) could be the underlying cause of myocardial ischemia. SCAD is considered nowadays a rare disease that occurs in 0.1–1.1% of most angiographic series and represents 0.1–4% of ACS (2,3). Notably, more of 80% of SCAD cases occurs in female (3) causing 24% of myocardial infarction (MI) in young women (3). Its incidence appears to be low in most angiographic series but recent studies found out that it could be misdiagnosed in more of 70% cases (4) because the classical hallmarks such as radiolucent signs of intimal flap or multiple lumens due to contrast staining in the false lumen are not easily found. A great pulse to its recognition has been brought from new technologies in the field of intravascular imaging, namely intravascular ultrasound (IVUS) and optical coherence tomography (OCT). Furthermore, compared with men, women presenting with ACS, are up to 30% less likely to be referred for catheterization (1).
Physiopathological mechanisms of SCAD consist of a primary tear in the intima or an intramedial bleeding caused by the rupture of dysfunctional vasa vasorum. The detachment of wall layers leads to the creation of a false lumen that inevitably limits the main coronary flow, leading to myocardial ischemia. Clinical manifestations include ACS, especially ST-segment elevation myocardial infarction (STEMI), syncope, cardiogenic shock or sudden cardiac death (2,3).
SCAD is a multifactorial disease. Known predisposing factors are related to the patient such as female gender, age <50 years, peripartum period or multiple prior pregnancies and hormonal therapy or to his vascular anatomy, e.g., coronary artery tortuosity, the absence of atherosclerotic plaques in remaining arteries and extra-coronary vascular abnormalities, especially connective tissue disorders (2,3,5). Additionally, the Canadian group from Vancouver recently discovered the existence of a strong connection between SCAD and fibromuscular dysplasia (FMD), a condition that also affects women (6).
In patients with these predisposing conditions, precipitating factors such as intense exercise, particularly isometric, or emotional stress, may trigger SCAD (7).
Given the challenging diagnosis and controversial treatment of SCAD, we propose a clinical-angiographic score (Figure 1) and a therapeutic strategy.
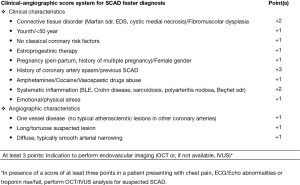
Based on our approach, patients presenting with chest pain, ECG or echocardiogram abnormalities and rise/fall of cardiac biomarkers (preferably troponin) with a score of at least 3, according to suspected angiograms, should undergo an endovascular imaging examination. IVUS and OCT can indeed clarify the ambiguous appearance of SCAD and help in detecting alternative diagnosis. We prefer OCT as the first choice since it provides ten times better axial resolution (15 µm), gives insights on the underlying anatomic substrate, depicts the entry tear, the circumferential and longitudinal extent of the disease, and the involvement of related side branches (8), reveals the occurrence of thrombosis in the false lumen and the presence of an intramural hematoma. Moreover, in the cohort of patients undergoing revascularization, OCT confirms the position of the guidewire and helps in choosing the correct length of the stent.
Speaking of therapeutic strategies, we suggest a conservative management in case of asymptomatic, hemodynamically stable patients with dissections occurring distally or inside small vessels (diameter <3.0 mm). This watchful waiting strategy is justified by the fact that spontaneous healing represents the natural history of this condition in the majority of cases. There is no evidence about beneficial effects of standard ACS medical therapy in patients with SCAD. Despite this, administering double antiplatelet therapy (DAPT) for 12 months seems reasonable.
Conversely, an invasive approach with bioresorbable vascular scaffold (BVS) should be preferred in the case of proximal/middle vessel lesions, occurring in larger vessels (≥3.0 mm vessel diameter) and whenever the patient is still symptomatic or hemodynamically unstable (5,9). Although large trials are needed, BVS strategy has been described as safe and efficient in several case reports as well as in our own case series (10) and experience (5).
Coronary-aortic bypass graft (CABG) seems reasonable in cases of left main coronary artery involvement, multivessel disease or concomitant valve disease (2,3).
Regarding the future of patients with a previous SCAD, we recommend a close clinical follow-up at 1, 3, 6 and 12 months with or without intravascular imaging. In the case of persistent symptoms or extensive disease, an invasive evaluation with coronary angiography after 6 to 12 months should be performed.
The overall outcome of patients who survived their first episode of SCAD is good and long-term mortality is lower than for ACS controls. However, long-term MACEs are frequent, including recurrent SCAD, post-partum women have larger MIs and lower mean ejection fraction and SCAD could have fatal exitus (3).
Our purpose is to bring attention to a rare cause of myocardial infarction. Given the absence of international guidelines or expert consensus documents on this hot topic, our approach could be a good starting point to avoid misdiagnoses and to allow a faster recognition and treatment of this condition. Our score needs further evaluation in larger ad hoc studies but it has been already validated on case reports and case series, giving promising results (11).
Under the circumstances, the European Society of Cardiology, in partnership with the Acute Cardiovascular Care Association (ACCA), established a European SCAD registry as a platform for collaborative research with the aims of improving awareness of this condition, advising clinicians to seek aid with patient management, promoting collaboration and creating a European registry of SCAD survivors to facilitate research.
From our side, we recently launched a survey, currently underway, addressed to the corresponding authors of 608 PubMed results for “SCAD” from the year 2000.
Finally, in young patients presenting with clinical or instrumental suspicion of ongoing ischemia, especially when with normal angiograms, it is advisable to consider SCAD as an important underlying cause of juvenile MI, especially if women and in the post-partum period. Just because you can’t see it, doesn’t mean it’s not happening.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Hamm CW, Bassand JP, Agewall S, et al. ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: The Task Force for the management of acute coronary syndromes (ACS) in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J 2011;32:2999-3054. [Crossref] [PubMed]
- Yip A, Saw J. Spontaneous coronary artery dissection-A review. Cardiovasc Diagn Ther 2015;5:37-48. [PubMed]
- Tweet MS, Hayes SN, Pitta SR, et al. Clinical features, management, and prognosis of spontaneous coronary artery dissection. Circulation 2012;126:579-88. [Crossref] [PubMed]
- Saw J, Mancini GB, Humphries K, et al. Angiographic appearance of spontaneous coronary artery dissection with intramural hematoma proven on intracoronary imaging. Catheter Cardiovasc Interv 2016;87:E54-61. [Crossref] [PubMed]
- Buccheri D, Piraino D, Latini RA, et al. Spontaneous coronary artery dissections: A call for action for an underestimated entity. Int J Cardiol 2016;214:333-5. [Crossref] [PubMed]
- Saw J, Poulter R, Fung A. Intracoronary imaging of coronary fibromuscular dysplasia with OCT and IVUS. Catheter Cardiovasc Interv 2013;82:E879-83. [Crossref] [PubMed]
- Saw J, Aymong E, Sedlak T, et al. Spontaneous coronary artery dissection: association with predisposing arteriopathies and precipitating stressors and cardiovascular outcomes. Circ Cardiovasc Interv 2014;7:645-55. [Crossref] [PubMed]
- Alfonso F, Paulo M, Gonzalo N, et al. Diagnosis of spontaneous coronary artery dissection by optical coherence tomography. J Am Coll Cardiol 2012;59:1073-9. [Crossref] [PubMed]
- Panoulas VF, Ielasi A. Bioresorbable scaffolds and drug-eluting balloons for the management of spontaneous coronary artery dissections. J Thorac Dis 2016;8:E1328-E1330. [Crossref] [PubMed]
- Ielasi A, Cortese B, Tarantini G, et al. Sealing spontaneous coronary artery dissection with bioresorbable vascular scaffold implantation: Data from the prospective "Registro Absorb Italiano" (RAI Registry). Int J Cardiol 2016;212:44-6. [Crossref] [PubMed]
- Buccheri D, Piraino D, Cortese B. Intravascular imaging as a tool for definite diagnosis of acute coronary syndrome caused by spontaneous coronary artery dissection. Int J Cardiol 2016;214:43-5. [Crossref] [PubMed]


