Principles of biopsy in suspected lung cancer: priority still based on invasion in the era of targeted therapy?
Introduction
Tumor biopsy is an essential part of the diagnostic workup and sound therapeutic decision making in oncology. For patients with suspected lung neoplasms, diagnosis and staging of the tumor are paramount to direct an optimal treatment plan (1,2). There are multiple ways to obtain a biopsy for patients with suspected lung cancer under clinical circumstances. Percutaneous, endoscopic, incisional, and excisional biopsies have different indications, invasion, accuracy, and efficacy (2,3). These sampling techniques should be properly selected or planned in reasonable sequence on a specific case. Principles of biopsy described previously in literature were based on the safety, invasion, and cost (3,4). As the development of individualized treatment in clinical oncology, molecular profile was imperative in lung cancer patient management. Molecular selection triumphed clinical selection in the era of targeted therapy (5,6). Histological classification, molecular examination, screening for clinical trials, and establishment of tissue bank required more and more tissue (5,7-10). Therefore, principles of biopsy for suspected lung cancer have to be revisited in the era of targeted therapy. We reported a patient with suspected lung cancer undergoing various biopsy techniques.
Case presentation
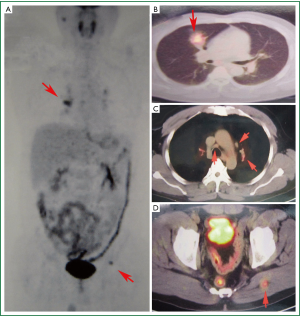
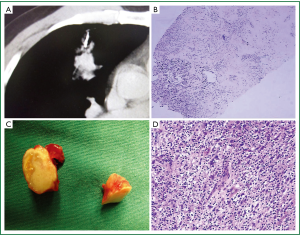
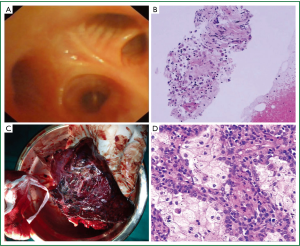
A 53-year-old gentleman consulted to our hospital because of bloody sputum. He experienced 10-year dust exposure in previous occupation, and was diagnosed with diabetes mellitus five years ago. As a smoker with 80 pack-year cigarette history, he presented blood-streaked sputum one month ago, and the symptom was persistent. Physical examination revealed no significant signs. Laboratory tests including complete blood count, biochemistry profile and tumor markers (CYFRA, SCC, and CEA) were within normal range. PET/CT scanning showed a mass in the anterior segment of right upper lung lobe, with 3.2 centimeters in diameter, and the maximum standard uptake value (SUV) achieved 5.5. Metabolically active lesions were also detected in multiple stations of mediastinal or bilateral hilar lymph nodes, and an intramuscular nodule in the left gluteus maximus (Figure 1). Due to lung cancer was suspected clinically, he underwent transthoracic core needle biopsy of lung lesion on the date of hospitalization. Blood clot and phagocytic cells were detected in pathological examination (Figure 2A,B). One week later he underwent resection of intramuscular nodule, aggregation of foamy histiocytes and surrounding fibrosis plus calcification was detected pathologically (Figure 2C,D). The following bronchoscopy also revealed non-malignancy (Figure 3A,B). Finally, right upper lung lobectomy was performed after a 3-week stay in hospital. The final diagnosis was considered as systemic lipid deposition (Figure 3C,D). Clinical data of the patient was from the electronic medical record database of the Guangdong Lung Cancer Institute (GLCI). The study was approved by the Institutional Review Boards of Guangdong General Hospital (GGH). Informed consent was obtained from the patient.
Discussion
The reported case was clinically diagnosed as advanced lung cancer based on imaging data. There were several candidate lesions for biopsy, and various biopsy techniques with different performance characteristics may apply. One lesion would be selected as the prioritized target in clinical practice. Scientific arrangement in biopsy selection should refer to available principles. The existing biopsy concepts were established in the age of cyto-toxic chemotherapy, and were based on the safety, invasion, and cost (3,4). As the oncology developed into the era of individualized treatment, tumor biopsy aimed to meet not only evidence of malignancy, but also molecular profiling and translational study. The presented patient initially underwent CT guided transthoracic core needle biopsy on lesion in the right upper lung lobe. It was a minimally invasive procedure for this case (11,12). And the maneuver was efficacious as it was conducted on the date of hospitalization. But core needle biopsy failed to establish a diagnosis on this case, although its safety was observed afterwards. Even the needle biopsy of lung lesion could detect malignancy; the pathological staging of the disease would not achieve. Thus, core needle biopsy on lung mass could not direct the whole management of the patient, and should not be the priority in biopsy sequence. There was a similar story with bronchoscopy in this patient. Both core needle biopsy and bronchoscopy may face a dilemma in subsequent management in that acquisition of tissue for molecular profiling, or slides for trial screening would not fulfill. For the surgical resection of intramuscular nodule in the gluteus maximus, the procedure determined if the disease was classified as stage IV with solitary distant metastasis. Because the gluteus maximus was not a common metastatic site of lung cancer, confirmation of the intramuscular nodule was pivotal in subsequent management (13-15). Therefore, biopsy of intramuscular nodule held the highest weight in diagnosis and treatment. And, the surgical specimen could fulfill the molecular profiling, meet clinical trials screening or provide additional tissue for tissue bank establishment. With regard to safety and efficacy, the excisional procedure would have to be conducted in operation room; registration for operation may prolong the patient’s stay in hospital, but its safety was proved and should be on the top of biopsy options for this patient. Lobectomy in this case was more invasive, more costly and time consuming, when compared with the aforementioned biopsy techniques, but the procedure produced the largest tissue and determined the final diagnosis.
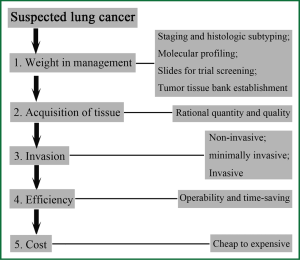
Based on the above discussion, we could propose principles of biopsy in suspected lung cancer into five items (Figure 4). Item I, weight in whole management. For a patient with suspected malignancy, clinical doctors should plan the framework of following management, evaluate the weight of available biopsic techniques for management, and select a key biopsy site. Item II, acquisition of tissue. The biopsy technique should provide tissue with rational quantity and quality to support the whole management. Item III, invasion. Progress on instruments and techniques provide increased patient comfort, excellent cosmetic results and minimal morbidity (4). Biopsy in surgical way could be prioritized when it became a determinant to clinical management. Item IV, efficiency. An efficacious biopsy could shorten the stay in hospital before reach a sound therapeutic decision. Item V, medical cost. The affordability for specific biopsy technique should be taken into account. Evaluation of four biopsy techniques performed on the reported patient was summarized in Table 1. Surgical resection of intramuscular nodule should be the prioritized biopsic technique for this patient.

Full Table
Conclusions
Principles of biopsy in suspected lung cancer should be based on weight in clinical management, acquisition of tissue, invasion, efficiency and cost as priority in sequence.
Acknowledgements
This work was supported by Guangdong Science and Technology Department, Industry Technology Research and Development Projects, Grant No. 2011A030400010 and Guangzhou Science and Information Technology Bureau, Grant No. 2011Y2-00014 (Y.-L.W.).
Disclosure: The authors declare no conflict of interest.
References
- Ehrhart N. Principles of tumor biopsy. Clin Tech Small Anim Pract 1998;13:10-6. [PubMed]
- Stone EA. Biopsy: principles, technical considerations, and pitfalls. Vet Clin North Am Small Anim Pract 1995;25:33-45. [PubMed]
- Yung RC. Tissue diagnosis of suspected lung cancer: selecting between bronchoscopy, transthoracic needle aspiration, and resectional biopsy. Respir Care Clin N Am 2003;9:51-76. [PubMed]
- Rivera MP, Mehta AC, American College of Chest Physicians. Initial diagnosis of lung cancer: ACCP evidence-based clinical practice guidelines (2nd edition). Chest 2007;132:131S-148S.
- Cheng L, Alexander RE, Maclennan GT, et al. Molecular pathology of lung cancer: key to personalized medicine. Mod Pathol 2012;25:347-69. [PubMed]
- Grüllich C, von Kalle C. Recent developments and future perspectives of personalized oncology. Onkologie 2012;35:4-7. [PubMed]
- Mok TS, Wu YL, Thongprasert S, et al. Gefitinib or carboplatin-paclitaxel in pulmonary adenocarcinoma. N Engl J Med 2009;361:947-57. [PubMed]
- Beasley MB, Brambilla E, Travis WD. The 2004 World Health Organization classification of lung tumors. Semin Roentgenol 2005;40:90-7. [PubMed]
- Travis WD, Brambilla E, Noguchi M, et al. International Association for the Study of Lung Cancer/American Thoracic Society/European Respiratory Society: international multidisciplinary classification of lung adenocarcinoma: executive summary. Proc Am Thorac Soc 2011;8:381-5. [PubMed]
- Manegold C. eds. Non-Small Cell Lung Cancer Treatment (1st edition). Bremen: UNI-MED, 2007:24-7.
- Steil S, Zerwas S, Moos G, et al. CT-guided percutaneous core needle biopsy in oncology outpatients: sensitivity, specificity, complications. Onkologie 2009;32:254-8. [PubMed]
- Gupta S, Wallace MJ, Morello FA, et al. CT-guided percutaneous needle biopsy of intrathoracic lesions by using the transsternal approach: experience in 37 patients. Radiology 2002;222:57-62. [PubMed]
- Detterbeck FC, Boffa DJ, Tanoue LT. The new lung cancer staging system. Chest 2009;136:260-71. [PubMed]
- Mercier O, Fadel E, de Perrot M, et al. Surgical treatment of solitary adrenal metastasis from non-small cell lung cancer. J Thorac Cardiovasc Surg 2005;130:136-40. [PubMed]
- Quint LE, Tummala S, Brisson LJ, et al. Distribution of distant metastases from newly diagnosed non-small cell lung cancer. Ann Thorac Surg 1996;62:246-50. [PubMed]