Learning curve and established phase for uniportal VATS lobectomies: the Papworth experience
Introduction
Uniportal video-assisted thoracoscopy (VATS) gained importance in the thoracic surgery scenario in the last years. The development of angulated instruments and articulated staplers has helped to perform major pulmonary resections such as lobectomies through a single 4-cm incision approach (1). In the literature, the benefit of the uniportal versus the triportal VATS is still debated, but many authors report that the it reduces postoperative pain (2-4) and often the length of stay (4). Furthermore, this surgical technique gives the surgeon the same operative perspective as open surgery, but with the advantages of the minimally invasive approach (5). To the best of our knowledge, there are no studies concerning the learning curve of uniportal VATS lobectomies. Therefore, this study aimed to review our experience of uniportal VATS lobectomies and to evaluate the feasibility and learning curve of this technique.
Methods
Surgical technique
The required instrumentation was the same as for the conventional VATS, including in particular polymer ligating clips with a 45° clip applier, an articulated endoscopic stapler and the Ligasure (Covidien – Medtronic, Minneapolis, USA) as energy device for the dissection. We used a 10-mm, 30°, angled thoracoscopic video camera. The performed incision was 4 cm long and located in the 5th intercostal space, mid axillary line. After the operation, one chest tube was routinely used and was inserted though the posterior part of the incision.
Data collection
We analysed retrospectively the data of 73 patients that underwent uniportal VATS lobectomies from November 2014, when we started to introduce the uniportal approach in our institution until December 2015. The selection criteria for the patients undergoing uniportal VATS lobectomies was the same as for the tri- or biportal VATS. Within this period of time we only performed VATS procedure for patients requiring lobectomies using the uniportal technique, whenever feasible and indicated. For patients requiring lobectomies who did not meet the criteria for VATS, we choose the classic open approach (12 in total).
For statistical reasons the patients were divided in two groups (group 1: initial group of first 30 patients vs. group 2: established phase, 43 patients) to compare and evaluate the data regarding the learning curve and the established phase. The performing surgeons (4 in total) were already experienced in triportal and biportal VATS lobectomies. The study was approved as part of a clinical audit for service evaluation to analyse if uniportal VATS was more cost and time effective compared to triportal VATS and if there were complications.
As this was a retrospective review for service evaluation and there was no modification in patients’ care (no prospective randomised study), we did not need the ethic approval in our institution.
Statistical analysis
Statistical analysis was realized with the bootstrap method using 1,000 simple bootstrap samples with 95% confidence interval. Bootstrap analysis was proposed as a breakthrough method for internal validation of surgical regression models (6). Characteristics of the patients were compared using the independent samples Student’s t-test (for age and lung function) and the Bravais-Pearson’s χ2 test or the Fisher’s exact test when appropriate (for gender, and removed lobe). Independent samples t-tests were used to compare the procedures performed in the two groups. To explore a possible development in conversion rate and complications as the surgeons progressed along the learning curve, they were plotted and the correlations were calculated using the Spearman’s Rank-Order Correlation. The learning curve technique can be applied to any surgical process with a binary outcome. It is understandable that after a definite number of surgical procedures, both the operation times and complication rates decline; nevertheless, in uniportal VATS lobectomies the estimated number of procedures that have to be performed until the learning curve is saturated has not been calculated. In this study, the acceptable failure rate for the operation time was set at 50%. The acceptable failure rate for postoperative complications was set at 5%, for non uniportal VATS cases at 5%. The unacceptable failure rate for the operation time was set at 70%, for postoperative complications at 10%, for non-uniportal VATS cases at 10%. This assumption was supported by considering the data in our study and usually acceptable or unacceptable standards. R version 3.2.3 was used for statistical analysis (R Core Team. 2014. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. Available online: http://www.R-project.org/).
Results
Table 1 listed the patients’ characteristics distributed in the different groups. There were no statistically significant differences in groups for the features of patients. The patients consisted in 33 males and 40 females. The median age was 69.3 years in the whole group; 69.9 (group 1) and 68.8 (group 2) years.
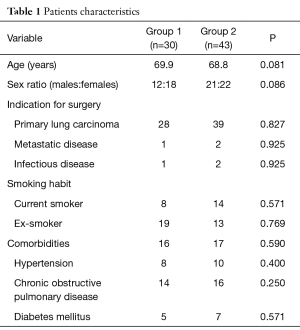
Full table
Overall the indication to undergo surgery was for primary carcinoma of the lung in 67 patients (54 adenocarcinoma, 13 squamous carcinoma), for metastatic disease (3 patients) and for infectious disease (3 patients). Twenty-two patients were current smokers and 32 ex-smokers. Of the 75 patients, 33 had underlying comorbidities, including hypertension, chronic obstructive pulmonary disease and diabetes mellitus.
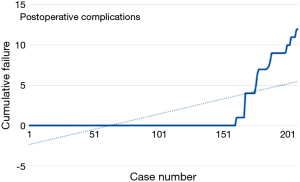
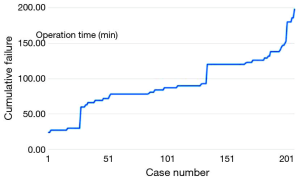
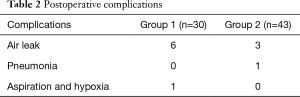
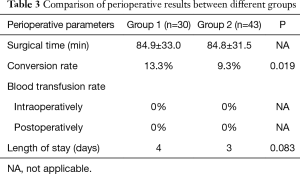
The mean operative time was 84.9±33.0 (group 1) and 84.8±31.5 (group 2) minutes, median time 97.5 (group 1) and 91.3 (group 2) minutes showing a learning reduction (Figure 1). The conversion rate to thoracotomy was 13.3% in the group 1 vs. 9.3% in group 2, showing a significant learning reduction (rho=0.590). The reasons for conversion to thoracotomy were vascular injuries, unfavourable anatomy and tumorous invasion of the pulmonary artery in one case. Blood transfusion rate was 0% intra- and postoperatively. The median intraoperative blood loss was 280 mL for group 1 and 200 mL for group 2. In Table 2 are shown the postoperative complications. Overall morbidity rate was 15.1%. The most common complication consisted in prolonged air leak. Interpolation line of complications showed a significant decrease due to learning curve (rho=0.676) (Figure 2).
Full table
The median length of stay was 4 days in group 1 vs. 3 days in the second group. The 30-day mortality was 3.3% in group 1 (one patient died because of aspiration and hypoxia on the second postoperative day) and 0% in the group 2 (Table 3).
Full table
The limitations of this study are the small number of patients included in the series and its retrospective nature.
Discussion
The feasibility and advantages of uniportal VATS have already been described in the literature, as stated before. With the improvement and further development of the uniportal VATS technique, the indication of this procedure has been largely extended and technical barriers are constantly being overtaken (7). The use of uniportal VATS in more complicated procedures as segmentectomy (8), pneumonectomy (9) and double sleeve lobectomy (10) has also been reported.
Uniportal VATS lobectomies are performed in many centres around the world, but we do not have much information in the literature about the learning curve and about the implications for the patients of starting using this technique.
The introduction of VATS lobectomies in the early 90s was performed by self-taught surgeons experienced in open surgery. The different techniques varied from anterior, inferior to posterior approaches, using 2 to 5 ports (11,12). These surgeons were pioneers, but the next generation learned the technique under guided supervision. The conditions for those surgeons’ learning curves were better due to the possibility of learning under supervision by an experienced VATS surgeon and a better possibility for selecting cases suitable for a training surgeon (13). The length of the learning curve has been suggested to consist of 50 VATS lobectomies, but several factors influence the length of the learning curve. For example, the size of the centre and the potential number of VATS lobectomies to be performed influence the length of the learning curve, as it is an advantage to perform many operations within a short time frame at the beginning of the learning curve (14). The experience of the surgeon in training is another important factor, as understanding the anatomy of the lung with the many anatomical variations makes the learning curve shorter. Okyere et al. (15) state that the learning curve for multiportal VATS lobectomy is not eliminated by prior experience in open lobectomy and that junior surgeons with less experience in open lobectomy are able to demonstrate similar outcomes and similar learning curves to their more experienced counterparts (11). Is this true also for the switch from multiportal to uniportal? Is the learning curve for uniportal VATS lobectomy affected by prior experience in VATS lobectomy? Experience with other VATS procedures is an advantage and performing more than 100 VATS procedures is an advantage as the surgeon will get familiar with the port placement and working with the VATS tools in a monitor based setting (14). This is also shown in the results of our study, since all surgeons in our institution were already experienced in performing basic and advanced VATS procedures. In our study, the comparison between the two groups shows that the median length of stay, operative time, conversion rate and 30-day mortality statistically significantly improved in the second group (established phase) in comparison with the first group (learning phase). Conversion rates were significantly reduced during the second half of the study, indicating an improved ability to avoid and manage problems. Also, complications like prolonged air leak (meaning air leak lasting beyond postoperative day 5, as described in recent literature) were decreasing in the established phase.
Another general recommendation is to take uniportal VATS courses and visit clinics with experience in uniportal VATS lobectomy to observe the procedure or alternatively to do a fellowship in a clinic with a high volume in uniportal VATS lobectomy.
The surgeons in our institution adopted a systematic approach to learn the technique. Although it is tempting, especially for experience VATS surgeons, to move from three ports to single port with little preparation, mostly based on watching heavily edited videos, we do not recommend this approach.
At the beginning of our experience, we spent a week in a high-volume centre; it was invaluable to see several surgeons performing the technique and also observe entire cases. Armed with this knowledge two consultant surgeons assisted each other for the first 20 cases. We found that such approach allows overcoming technical difficulties, provides mutual reassurance and facilitates management of complications that required conversion.
Another recommendation is to standardise the surgical approach. Although it s tempting to move the incision according to the lobe to be resected, we made the access incision always on the 5th intercostal space in front of the latissimus dorsi muscle. The camera was almost always in the upper part of the incision, instruments in the middle and stapler in the bottom. Once overcome the initial feeling of moving things around all the time, this approach is the easiest and the one that offers the least amount of conflict between instruments. Another recommendation is to resist the temptation of inserting more instruments than necessary through the wound in the attempt to achieve a good visualisation. Thoracoscope, sucker and energy devices, together with a lung grasper are enough to achieve excellent visualisation. If the view is suboptimal we repositioned the instruments rather than add few more. Although quite time consuming at first, once familiarised with the new angles everything became easier. The last point we would like to make relates to the fact that single port VATS is a completely different technique from three ports. The surgical view, stapler angle and retraction technique are different and require a different set of skills and the patience to learn them.
In conclusion, the uniportal VATS lobectomy technique can be performed safely from experienced surgeons without major complications and with an acceptable mortality rate.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: As this was a retrospective review for service evaluation and there was no modification in patients’ care (no prospective randomised study), we did not need the ethic approval in our institution.
References
- Bedetti B, Scarci M, Gonzalez-Rivas D. Technical steps in single port video-assisted thoracoscopic surgery lobectomy. J Vis Surg 2016;2:45. [Crossref]
- Salati M, Brunelli A, Rocco G. Uniportal video-assisted thoracic surgery for diagnosis and treatment of intrathoracic conditions. Thorac Surg Clin 2008;18:305-10. vii. [Crossref]
- Anile M, Diso D, Mantovani S, et al. Uniportal video assisted thoracoscopic lobectomy: going directly from open surgery to a single port approach. J Thorac Dis 2014;6:S641-3.
- Jutley RS, Khalil MW, Rocco G. Uniportal vs standard three-port VATS technique for spontaneous pneumothorax: comparison of post-operative pain and residual paraesthesia. Eur J Cardiothorac Surg 2005;28:43-6. [Crossref]
- Bertolaccini L, Rocco G, Viti A, et al. Geometrical characteristics of uniportal VATS. J Thorac Dis 2013;5 Suppl 3:S214-6.
- Blackstone EH. Breaking down barriers: helpful breakthrough statistical methods you need to understand better. J Thorac Cardiovasc Surg 2001;122:430-9. [Crossref]
- Tu CC, Hsu PK. Global development and current evidence of uniportal thoracoscopic surgery. J Thorac Dis 2016;8:S308-18.
- Cheng K, Zheng B, Zhang S, et al. Feasibility and learning curve of uniportal video-assisted thoracoscopic segmentectomy. J Thorac Dis 2016;8:S229-34.
- Gonzalez-Rivas D, Delgado M, Fieira E, et al. Uniportal video-assisted thoracoscopic pneumonectomy. J Thorac Dis 2013;5 Suppl 3:S246-52.
- Gonzalez-Rivas D, Delgado M, Fieira E, et al. Double sleeve uniportal video-assisted thoracoscopic lobectomy for non-small cell lung cancer. Ann Cardiothorac Surg 2014;3:E2.
- McKenna RJ Jr, Houck W, Fuller CB. Video-assisted thoracic surgery lobectomy: experience with 1,100 cases. Ann Thorac Surg 2006;81:421-5; discussion 425-6. [Crossref]
- Hansen HJ, Petersen RH, Christensen M. Video-assisted thoracoscopic surgery (VATS) lobectomy using a standardized anterior approach. Surg Endosc 2011;25:1263-9. [Crossref]
- Petersen RH, Hansen HJ. Learning curve associated with VATS lobectomy. Ann Cardiothorac Surg 2012;1:47-50.
- McKenna RJ Jr. Complications and learning curves for video-assisted thoracic surgery lobectomy. Thorac Surg Clin 2008;18:275-80. [Crossref]
- Okyere S, Attia R, Toufektzian L, et al. Is the learning curve for video-assisted thoracoscopic lobectomy affected by prior experience in open lobectomy? Interact Cardiovasc Thorac Surg 2015;21:108-12. [Crossref]