Clinical factors associated with weaning failure in patients requiring prolonged mechanical ventilation
Introduction
The number of patients requiring mechanical ventilation (MV) has increased worldwide, and the proportion of patients requiring prolonged mechanical ventilation (PMV) has increased concomitantly (1,2). The hospital mortality and overall 1-year mortality rates for patients requiring PMV are also very high (3,4). However, PMV has been variously defined as >24 hours (5), >2 days (6,7), >3 days (8), >14 days (9,10), or >21 days (2,11,12) of MV in different studies. Nonetheless, PMV has been defined recently, by consensus, constituting ≥21 consecutive days of MV for ≥6 hours per day because most patients receiving MV who are transferred to a long-term acute care (LTAC) hospital have received MV for at least 21 days (13).
Weaning success is an important prognostic factor in patients requiring PMV (14,15). However, the rate of weaning success in patients requiring PMV is low, ranging from 38% to 78% (11,16-18). Several studies showed that the incidence of chronic obstructive pulmonary disease (COPD), neuromuscular disease, high body mass index, pneumonia, and high positive end-expiratory pressure were associated with weaning failure in patients requiring PMV (3,19). However, it is unclear which clinical factors influence weaning failure or success because of the different definitions of PMV.
We hypothesized that the assessment of specific clinical factors on day 21 of MV is predictive of weaning outcomes in patients requiring PMV. These clinical factors include the patient’s acute physiology and chronic health evaluation III (APACHE III) score, and sequential organ failure assessment (SOFA) score. The aim of this study was to evaluate the clinical characteristics and parameters associated with weaning failure in patients requiring MV for more than 21 days in the medical intensive care unit (ICU).
Methods
Subjects
We retrospectively reviewed the medical records of patients who stayed for more than 21 days in the medical ICU at Chonnam National University Hospital in South Korea between January 2005 and December 2014. Patients who underwent surgery or experienced trauma were excluded from this study. This retrospective clinical study was approved by the Institutional Review Board of the Chonnam National University Hospital (CNUH-2017-016).
PMV was defined as the need for ≥21 consecutive days of MV for ≥6 hours per day (13).
Data collection
The clinical and demographic characteristics, including age, sex, comorbidities, etiologies underlying ICU admission, presence of sepsis and multiple organ dysfunction syndrome (MODS), duration of MV, length of stay in the ICU and hospital, tracheostomy rate, weaning success rate, and ICU and in-hospital mortality were recorded. Weaning success was defined as the complete liberation from MV for seven consecutive days (13). The APACHE III score was determined at the time of ICU admission and on day 21 of MV. We calculated the SOFA score on day 21 of MV. Sepsis was considered if infection was suspected with evidence of systemic inflammation, based on a recent international consensus conference (20). Organ failure was defined according to the consensus committee of the American College of Chest Physicians and the Society of Critical Care Medicine (21). MODS was defined as the incidence of more than two organ dysfunctions. We followed the guidelines specified for neuromuscular blockade and sedative agents (22), lung protective ventilation (23,24), and spontaneous breathing trials (25).
Statistical analysis
For the sample size calculation, we used a power and sample size calculation program (http://biostat.mc.vanderbilt.edu/wiki/Main/PowerSampleSize). This study design accounted for the low rate of weaning success in patients requiring PMV by assigning a 1:2 ratio of patients for the weaning success to weaning failure groups. There are no previous studies that have compared the differences in APACHE III scores for weaning failure and weaning success in patients with PMV. We based our study design on a previous study in which a high APACHE III score was indicative of a longer duration of MV (26). We estimated that the mean difference of the two groups would be a value of 15 a normal distribution, and a standard deviation of 27 for each group, based on the results of a previous study and the characteristics of our cohort. The calculated minimum sample size of weaning success and weaning failure were 39 and 78, respectively, with 80% power and a type I error frequency of 5%.
The continuous variables were presented as medians or interquartile ranges and compared using the Mann-Whitney U tests. The categorical variables were presented as a number or as a percentage and compared using the Chi-squared tests. Univariate analysis was used to analyze the association of each variable with weaning, and ICU and in-hospital mortality. To determine the predictors of weaning and ICU and in-hospital mortality, the logistic regression analysis was used to perform a multivariate analysis. In the logistic regression analysis, stepwise and backward selection procedures were used to select the variables that were maintained in the final model, with a P value of <0.05 as the criterion for statistical significance. The SOFA score was assessed to predict weaning failure in patients requiring PMV using a receiver operating characteristic (ROC) curve. The Youden index was used to find the optimal cut-off value on the ROC curve. The statistical analyses were performed using SPSS 21.0 (IBM Corporation, Armonk, NY, USA). A P value of <0.05 was considered statistically significant.
Results
Basal characteristics of weaning success and failure groups
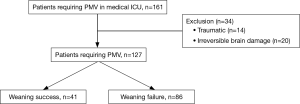
A total of 147 patients were consistent with the definition of PMV; 20 patients with irreversible brain damage were excluded (Figure 1). The basal characteristics of the patients requiring PMV according to weaning success or failure are shown in Table 1. Among the 127 patients requiring PMV, 41 (32.3%) were successfully weaned from MV. The median age of the weaning failure group was higher compared to that of the weaning success group (74.0 vs. 70.0 years; P=0.003). Men were predominant in both groups. There were no significant differences in the incidence of underlying comorbidities between both groups. The most common reasons for ICU admission were respiratory causes, followed by cardiovascular causes in both groups. Pneumonia was the most common respiratory causes for ICU admission in the weaning success group (41.5%) and weaning failure group (70.9%).
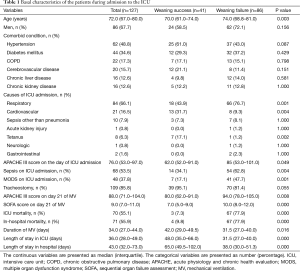
Full table
Respiratory causes of ICU admission were more common in the weaning failure group compared to the weaning success group (76.7% vs. 43.9%; P=0.001). Cardiovascular causes for ICU admission were more common in the weaning success group compared to the weaning failure group (31.7% vs. 9.3%; P=0.004). The median APACHE III scores on the day of ICU admission and on day 21 of MV were higher in the weaning failure group compared to the weaning success group (85 vs. 62, P=0.049; 94 vs. 80, P=0.008; respectively). The presence of sepsis and MODS on ICU admission was more common in the weaning failure group compared to the weaning success group, respectively (62.8% vs. 34.1%, P=0.004; 47.7% vs. 17.1%, P=0.001). Most patients underwent tracheostomy (85.8%), but no significant differences were evident between the groups (P=0.055). Of 39 patients who underwent tracheostomy with weaning success from MV, only 11 (28.2%) could undergo decannulation. The median SOFA score on day 21 of MV was higher in the weaning failure group compared to that of the weaning success group (7 vs. 10; P=0.000). The ICU mortality and in-hospital mortality were 55.1% and 55.9%, respectively. The weaning failure group had a significantly longer duration of ICU and in-hospital stay compared to that of the weaning success group.
Predicting factors for weaning failure in patients requiring PMV
Table 2 shows the results of the univariate and multivariate analysis for identification of predictive factors associated with weaning failure in patients requiring PMV. In the univariate analysis, seven clinical characteristics were associated with weaning failure (all P<0.05): age; respiratory causes; and a high APACHE III score and SOFA score on day 21 of MV. In the multivariate analysis, the respiratory causes of ICU admission [odds ratio (OR), 3.98; 95% confidence interval (CI), 1.29–12.30; P=0.016] and a high SOFA score on day 21 of MV (OR, 1.47; 95% CI, 1.17–1.85; P=0.001) were significantly associated with weaning failure in patients requiring PMV.
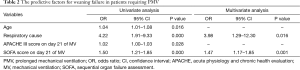
Full table
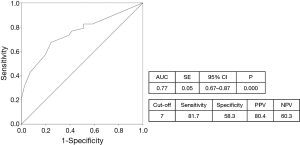
Figure 2 is a ROC curve of the SOFA score on day 21 of MV for predicting weaning failure in patients requiring PMV.
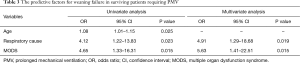
Predicting factors for weaning failure in surviving patients requiring PMV (subgroup analysis)
We performed a subgroup analysis on those who survived during hospitalization. A total of 56 patients survived during hospitalization, and 37 (66.1%) were weaned successfully from MV. Table 3 shows the results of the univariate and multivariate analysis for the identification of the predictive factors associated with weaning failure among the surviving patients requiring PMV. In the multivariate analysis respiratory causes of ICU admission (OR, 4.91; 95% CI, 1.29–18.68, P=0.019), and the presence of MODS on ICU admission (OR, 5.63; 95% CI, 1.41–22.51, P=0.015) were significantly associated with weaning failure in the surviving patients requiring PMV.
Full table
Discussion
In this retrospective study, we evaluated the factors associated with weaning outcomes in patients requiring PMV. Respiratory causes of ICU admission and a high SOFA score on day 21 of MV were associated with weaning failure in these patients.
Among the reasons for ICU admission, 66% of the patients had respiratory causes, and most of them were diagnosed with pneumonia in this study. A previous study showed that the incidence of chronic pulmonary diseases, with exception to COPD, postoperative acute respiratory failure, and pneumonia, was associated with difficult and prolonged weaning in patients with MV (27). COPD was not associated with weaning failure following a multivariate analysis in the present study. These findings could have resulted from the relatively small number of patients with COPD (17%) in the present study. Therefore, further studies are required to determine whether COPD reduces weaning success in patients requiring PMV.
The SOFA scoring system, which was introduced in 1994, is a reliable predictive factor of mortality during ICU stay (28). Gnanapandithan et al. reported that the value of the baseline SOFA scores at baseline was related to successful extubation from MV (29). Additionally, Tseng et al. reported that high SOFA score was also associated with an increased ventilator dependence in patients with VAP (30). In our study, a high SOFA score on day 21 of MV was associated with weaning failure in patients requiring PMV. The area under the ROC curve of the SOFA score on day 21 of MV for the prediction of weaning failure was 0.77 (95% CI, 0.67–0.87; P=0.000). In this study, the high SOFA score on day 21 of MV was also associated with ICU mortality (OR, 1.66; 95% CI, 1.30–2.12; P=0.000). Although the clinical predictive factors are multifactorial in patients requiring PMV, the SOFA score on day 21 of MV can also be predictive of both weaning failure and ICU mortality. However, SOFA score was not predictive weaning failure among in surviving patients. Because SOFA score was associated with both weaning failure and ICU mortality in this study, the predictability of SOFA score as weaning failure may decrease after exception of those non-survivors. Further multi-center prospective studies are necessary to validate the utility of assessing the SOFA score on day 21 of MV.
Recently, LTAC hospitals have been introduced for patients who require a longer hospital stay that can be accommodated in acute-care hospitals. LTAC hospitals are defined as acute-care hospitals with a mean length of stay of more than 25 days (31). Although LTAC facilities can reduce the length of ICU stay and hospital costs, survival and functional independence 1 year after discharge from the ICU are poor (32). There are also respiratory intermediate care units (RICU) and specialized regional weaning centers (WCs) available to patients who require additional care. The sequential admission to RICU and WCs can further improve the weaning success rate of difficult-to-wean patients (33). Unfortunately, our hospital does not offer the services associated with LTAC, RICU or WCs. This limitation might result in the lower rate of weaning success observed in the present study.
Most patients in this study (85.8%) underwent tracheostomy; however, only 32.3% of the patients were successfully weaned from MV. Tracheostomy may reduce the incidence of VAP, the duration of MV, and the length of ICU stay (34,35). However, the optimal timing of tracheostomy is still undefined. Early tracheostomy resulted in a decreased risk of mortality and increased weaning success in some studies (36-38). In contrast, early tracheostomy did not significantly alter the mortality rate or the duration of MV in other studies (39,40). In the present study, the interval from intubation to tracheostomy did not significantly differ between the weaning success and failure groups (a median day of 16 days vs. 15 days; P=0.725). Most patients requiring PMV eventually require tracheostomy to maintain their airways. However, it was apparent that tracheostomy failed to improve the weaning success of patients requiring PMV. Furthermore, PMV care must also be considered when tracheostomy is first proposed (13).
There were several limitations to this study. First, the number of patients included in this study was small as a single-center study. Additionally, there was also the possible risk of over-fitting due to the small number of enrolled patients and the presence of inter-dependent covariates that may have limited the statistical power of this study. Second, we could not completely follow up the patients who were transferred to other hospitals. Some patients who were successfully weaned from MV following a transfer to another hospital may have been excluded from our analysis. Third, although there are various factors associated with weaning failure, we could not fully examine the factors such as respiratory physiological parameters, MV modes, endocrine and metabolic dysfunction, ICU-acquired weakness, or diaphragm dysfunction, because this study was performed retrospectively. Therefore, future prospective multi-center studies of patients requiring PMV are necessary.
Conclusions
Patients requiring PMV have a low weaning success rate and poor outcomes. Although the predictive factors associated with weaning failure in patients requiring PMV are multifactorial, respiratory causes of ICU admission and a high SOFA score on day 21 of MV could be predictive of weaning failure in these patients.
Acknowledgements
Funding: This study was supported by a grant (CRI16005-1) from Chonnam National University Hospital.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This retrospective clinical study was approved by the Institutional Review Board of the Chonnam National University Hospital (CNUH-2017-016) and written informed consent was waived from all patients.
References
- Cox CE, Carson SS. Medical and economic implications of prolonged mechanical ventilation and expedited post-acute care. Semin Respir Crit Care Med 2012;33:357-61. [Crossref]
- Lone NI, Walsh TS. Prolonged mechanical ventilation in critically ill patients: epidemiology, outcomes and modelling the potential cost consequences of establishing a regional weaning unit. Crit Care 2011;15:R102. [Crossref]
- Mamary AJ, Kondapaneni S, Vance GB, et al. Survival in Patients Receiving Prolonged Ventilation: Factors that Influence Outcome. Clin Med Insights Circ Respir Pulm Med 2011;5:17-26. [Crossref]
- Damuth E, Mitchell JA, Bartock JL, et al. Long-term survival of critically ill patients treated with prolonged mechanical ventilation: a systematic review and meta-analysis. Lancet Respir Med 2015;3:544-53. [Crossref]
- Spicher JE, White DP. Outcome and function following prolonged mechanical ventilation. Arch Intern Med 1987;147:421-5. [Crossref]
- Chelluri L, Im KA, Belle SH, et al. Long-term mortality and quality of life after prolonged mechanical ventilation. Crit Care Med 2004;32:61-9. [Crossref]
- Clec'h C, Alberti C, Vincent F, et al. Tracheostomy does not improve the outcome of patients requiring prolonged mechanical ventilation: a propensity analysis. Crit Care Med 2007;35:132-8. [Crossref]
- Cox CE, Carson SS, Holmes GM, et al. Increase in tracheostomy for prolonged mechanical ventilation in North Carolina, 1993-2002. Crit Care Med 2004;32:2219-26. [Crossref]
- Karir V, Hough CL, Daniel S, et al. Sedation practices in a cohort of critically ill patients receiving prolonged mechanical ventilation. Minerva Anestesiol 2012;78:801-9.
- Hough CL, Caldwell ES, Cox CE, et al. Development and Validation of a Mortality Prediction Model for Patients Receiving 14 Days of Mechanical Ventilation. Crit Care Med 2015;43:2339-45. [Crossref]
- Rose L, Fraser IM. Patient characteristics and outcomes of a provincial prolonged-ventilation weaning centre: a retrospective cohort study. Can Respir J 2012;19:216-20. [Crossref]
- Loss SH, de Oliveira RP, Maccari JG, et al. The reality of patients requiring prolonged mechanical ventilation: a multicenter study. Rev Bras Ter Intensiva 2015;27:26-35. [Crossref]
- MacIntyre NR, Epstein SK, Carson S, et al. Management of patients requiring prolonged mechanical ventilation: report of a NAMDRC consensus conference. Chest 2005;128:3937-54. [Crossref]
- Engoren M, Arslanian-Engoren C, Fenn-Buderer N. Hospital and long-term outcome after tracheostomy for respiratory failure. Chest 2004;125:220-7. [Crossref]
- Bigatello LM, Stelfox HT, Berra L, et al. Outcome of patients undergoing prolonged mechanical ventilation after critical illness. Crit Care Med 2007;35:2491-7. [Crossref]
- Scheinhorn DJ, Hassenpflug MS, Votto JJ, et al. Ventilator-dependent survivors of catastrophic illness transferred to 23 long-term care hospitals for weaning from prolonged mechanical ventilation. Chest 2007;131:76-84. [Crossref]
- Rojek-Jarmuła A, Hombach R, Gierek D, et al. A single-centre seven-year experience with mechanical ventilation weaning. Anaesthesiol Intensive Ther 2015;47:204-9.
- Mifsud Bonnici D, Sanctuary T, Warren A, et al. Prospective observational cohort study of patients with weaning failure admitted to a specialist weaning, rehabilitation and home mechanical ventilation centre. BMJ Open 2016;6:e010025. [Crossref]
- Pan C, Qiu H. Improve survival from prolonged mechanical ventilation: beginning with first step. J Thorac Dis 2015;7:1076-9.
- Levy MM, Fink MP, Marshall JC, et al. 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit Care Med 2003;31:1250-6. [Crossref]
- Knaus WA, Draper EA, Wagner DP, et al. Prognosis in acute organ-system failure. Ann Surg 1985;202:685-93. [Crossref]
- Slomka J, Hoffman-Hogg L, Mion LC, et al. Influence of clinicians' values and perceptions on use of clinical practice guidelines for sedation and neuromuscular blockade in patients receiving mechanical ventilation. Am J Crit Care 2000;9:412-8.
- dos Santos CC, Slutsky AS. Protective ventilation of patients with acute respiratory distress syndrome. Crit Care 2004;8:145-7. [Crossref]
- Gillette MA, Hess DR. Ventilator-induced lung injury and the evolution of lung-protective strategies in acute respiratory distress syndrome. Respir Care 2001;46:130-48.
- Epstein SK. Decision to extubate. Intensive Care Med 2002;28:535-46. [Crossref]
- Seneff MG, Zimmerman JE, Knaus WA, et al. Predicting the duration of mechanical ventilation. The importance of disease and patient characteristics. Chest 1996;110:469-79. [Crossref]
- Peñuelas O, Frutos-Vivar F, Fernández C, et al. Characteristics and outcomes of ventilated patients according to time to liberation from mechanical ventilation. Am J Respir Crit Care Med 2011;184:430-7. [Crossref]
- Rapsang AG, Shyam DC. Scoring systems in the intensive care unit: A compendium. Indian J Crit Care Med 2014;18:220-8. [Crossref]
- Gnanapandithan K, Agarwal R, Aggarwal AN, et al. Weaning by gradual pressure support (PS) reduction without an initial spontaneous breathing trial (SBT) versus PS-supported SBT: a pilot study. Rev Port Pneumol 2011;17:244-52. [Crossref]
- Tseng CC, Huang KT, Chen YC, et al. Factors predicting ventilator dependence in patients with ventilator-associated pneumonia. ScientificWorldJournal 2012;2012:547241.
- Carson SS. Know your long-term care hospital. Chest 2007;131:2-5. [Crossref]
- Nasraway SA, Button GJ, Rand WM, et al. Survivors of catastrophic illness: outcome after direct transfer from intensive care to extended care facilities. Crit Care Med 2000;28:19-25. [Crossref]
- Carpenè N, Vagheggini G, Panait E, et al. A proposal of a new model for long-term weaning: respiratory intensive care unit and weaning center. Respir Med 2010;104:1505-11. [Crossref]
- Bouderka MA, Fakhir B, Bouaggad A, et al. Early tracheostomy versus prolonged endotracheal intubation in severe head injury. J Trauma 2004;57:251-4. [Crossref]
- Rumbak MJ, Newton M, Truncale T, et al. A prospective, randomized, study comparing early percutaneous dilational tracheotomy to prolonged translaryngeal intubation (delayed tracheotomy) in critically ill medical patients. Crit Care Med 2004;32:1689-94. [Crossref]
- Freeman BD, Borecki IB, Coopersmith CM, et al. Relationship between tracheostomy timing and duration of mechanical ventilation in critically ill patients. Crit Care Med 2005;33:2513-20. [Crossref]
- Combes A, Luyt CE, Nieszkowska A, et al. Is tracheostomy associated with better outcomes for patients requiring long-term mechanical ventilation? Crit Care Med 2007;35:802-7. [Crossref]
- Koch T, Hecker B, Hecker A, et al. Early tracheostomy decreases ventilation time but has no impact on mortality of intensive care patients: a randomized study. Langenbecks Arch Surg 2012;397:1001-8. [Crossref]
- Griffiths J, Barber VS, Morgan L, et al. Systematic review and meta-analysis of studies of the timing of tracheostomy in adult patients undergoing artificial ventilation. BMJ 2005;330:1243. [Crossref]
- Meng L, Wang C, Li J, et al. Early vs late tracheostomy in critically ill patients: a systematic review and meta-analysis. Clin Respir J 2016;10:684-92. [Crossref]


