Solitary fibrous tumors of pleura and lung: report of twelve cases
Introduction
Solitary fibrous tumors (SFTs) are uncommon soft tissue tumors. They were reported initially as a pleura-based lesion, but they also have been reported to occur in other sites including the lung, liver, orbit, nasal passages, skin, thyroid, and gastrointestinal tract. The SFTs are masses of mesenchymal origin. The finding of positive staining for CD34 and bcl-2 and negative staining for cytoplasmic keratin can confirm the presence of SFTs. However, positive staining for CD34 and bcl-2 does not always exist in malignant SFTs. These tumors are frequently observed in middle-aged adults, with no sex predilection. Most of them behave as slow-growing, painless masses. Large tumors may give rise to compression symptoms, or cause hypertrophic pulmonary osteoarthropathy (HPO) and refractory hypoglycemia, due to the production of a growth hormone-like substance and an insulin-like growth factor respectively. Usually they are found incidentally on chest radiography. Although most SFTs show benign behavior, some have malignant potential and should be excised. Benign SFTs can be cured by complete surgical resection. Since 1931, only 800 cases of such tumors have been reported (1).
Patients and methods
In this study, we reviewed 12 patients who had undergone surgical resection of benign SFTs of the pleura and lung during a period from 2006 to 2012. Clinical findings and follow-up information were obtained for all patients.
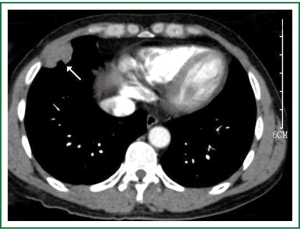
The study involved 7 male and 5 female patients, with a mean age of 47.8 years (range, 31-76 years). The past history of all the patients was unremarkable and none had familial hereditary disease. None had a history of asbestos exposure, but three male patients had a history of smoking. The two patients with cough and one patient who complained of back pain were examined by chest radiography or thoracic computed tomography (CT) respectively during a medical checkup. The other cases were found incidentally on chest radiography. All patients underwent a physical examination, routine blood test, standard chest radiography, electrocardiography and thoracic CT scan. Blood laboratory test results, including the values of CEA, AFP, CA125, CA153, were within normal limits. Three cases were pathologically diagnosed preoperatively and confirmed by transthoracic biopsy. Complete resection was performed through thoracotomy, which for eight cases involved video-assisted thoracic surgery (VATS). Seven cases originated from the right hemithorax and five cases originated from the left. Nine cases involved pedunculated tumors and three were sessile tumors. The tumor size ranged from 1.2 to 14 cm. Ten patients had tumor arising from the visceral pleura, one tumor originated from the parietal pleura and one was intrapulmonary (Figure 1). The tumors were resected with part of the pleura in nine cases with pedunculated tumors. Two cases with sessile tumors were treated by removing the tumor with pulmonary wedge resection. One patient with SFT of intrapulmonary origin was treated by pulmonary lobectomy.
Results
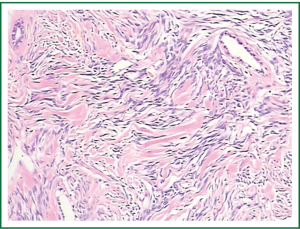
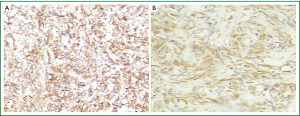
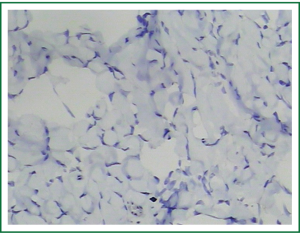
The most essential characteristic on histopathology was the presence of nonatypical spindle-shaped tumor cells on a collagenous background (Figure 2). Keloid-type collagen, hypocellular and hypercellular areas could be observed in all the cases. On immuno-histochemical analysis, we found that mesenchymal markers such as CD34, bcl-2 and vimentin were positive (Figure 3A,B), whereas S-100 protein and desmin were negative (Figure 4). The result for Ki-67 was positive in approximately 5% of the tumor cells, but C-kit protein was not detected. If the result of CD34 was negative, expression of bcl-2 was positive.
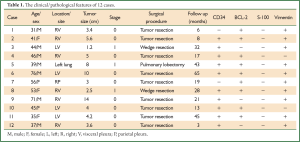
According to the de Perrot staging scheme [stage 0: pedunculated tumor without signs of malignancy; stage I: sessile or “inverted” tumor without signs of malignancy (2)], we judged that 9 cases were stage 0 and 3 cases were stage I. There was no operative morbidity or mortality. The postoperative courses were uneventful, and all the patients have been followed-up for 3-65 (mean 25) months without recurrence (Table 1).
Full Table
Discussion
Most SFTs arise from the submesothelial tissue of the pleura, especially the visceral pleura. They are commonly attached to the pleura by a pedicle. However, they may occur in various anatomical sites as well as the pleura. The frequency is fairly equal in patients of different ages and there is no sex predilection. There is no evidence of the relationship of such tumors with exposure to asbestos, tobacco, or any other environmental agent, and no apparent genetic predisposition.
More than 50% of benign SFTs of the pleura are asymptomatic (3). Other patients may show various clinical signs such as intrathoracic symptoms (dyspnea, chest pain, hemoptysis), systemic symptoms (hypoglycemia, HPO), or nonspecific symptoms (fever, weight loss, fatigue). Chest pain occurs more commonly in patients whose tumor originates in the parietal pleura. Larger tumors may cause compression of the bronchi and lead to atelectasis, with symptoms such as hemoptysis. Paraneoplastic syndromes such as HPO and hypoglycemia are uncommon, and these syndromes can be relieved by resection of the tumor.
Chest radiography is not specific but it is usually initial diagnostic test for SFTs. There are also no specific characteristics for the diagnosis of SFTs on chest CT scan, but it can show the size and location of the tumor clearly and help in surgical planning. About two thirds of the tumors can be enhanced by contrast medium because of increased vascularity of the tumor. It is more difficult to differentiate these tumors from bronchogenic carcinoma when they arise in an interlobar fissure surrounded by lung parenchyma. Given that the clinical features and radiographic appearance are not specific, SFTs are commonly misdiagnosed as other diseases, such as thymic neoplasia, teratoma, neurogenic tumor, malignant pleural mesothelioma or lung cancer. The specific method used to obtain a definitive diagnosis before operation is percutaneous transthoracic needle biopsy of the mass, although this does not influence the choice of surgery as treatment. Sung and his colleagues (4) have reported that the rate of obtaining a definitive preoperative diagnosis for SFTs by application of fine-needle aspiration (FNA) was 43%. However, because the risk of morbidity and mortality associated with the operation is very low and surgical resection involves simultaneous diagnosis and treatment, repeated FNA is not required even when a definitive preoperative pathologic result has not been obtained.
Immuno-histochemistry is the most important method used to differentiate SFTs from mesotheliomas and other sarcomas, because of the presence of specific biomarkers: CD34 is positive in most SFTs and negative in most other pulmonary tumors. The SFTs are generally vimentin positive and cytokeratin negative; In contrast, mesothelioma is cytokeratin positive and often vimentin negative. In addition, bcl-2 is strongly expressed in SFTs, and can be treated as a significant marker in CD34-negative tumors to confirm the diagnosis of SFT. Although hemangiopericytomas are CD34-positive tumors, bcl-2 is not expressed or only poorly expressed. In addition, most SFTs are CD99 positive and S-100 negative (2).
The primary therapy for all SFTs is complete surgical resection. Pedunculated tumors can be excised safely with VATS. To prevent the transfer of tumor cells and metastases, great caution should be exercised to avoid any contact of the tumor with the VATS port sites. Some cases, such as those involving sessile tumors of the visceral pleura or tumors within the lung parenchyma, require the excision of a large portion of the lung parenchyma, to reduce the likelihood of local tumor recurrence. Frozen sections should be made to ensure that the resected margins are free of tumor. However, those sessile tumors arising from the parietal pleura of the chest wall, diaphragm, or mediastinum require wide local extra-pleural excision.
The prognosis of benign SFTs of the pleura with complete surgical resection can be excellent, while careful follow-up is still necessary (5). The median survival for patients with all types of SFT has been reported to be 24 years (6). Significant differences can be found in recurrence and survival according to the gross morphologic and pathologic findings. Recurrence rates have been reported to be 63% for those in the malignant sessile group, 14% for the malignant pedunculated group, 8% in the benign sessile group and 2% in the benign pedunculated group (2). In the case of local recurrence, re-resection has been strongly recommended as a potentially curative treatment.
Conclusions
Most SFTs of pleura and lung are benign. Immunohistochemistry is extremely useful in differentiating SFTs from mesotheliomas and other sarcomas. Morphological and histological characteristics are important in predicting their clinical behaviour. Although patients with SFTs can be cured by complete resection of the tumor, they need long-term follow-up owing to the possibility of recurrence.
Acknowledgements
The authors are very grateful to Dr David Cushley, International Science Editing, for assistance with editing the manuscript.
Disclosure: The authors declare no conflict of interest.
References
- Robinson LA. Solitary fibrous tumor of the pleura. Cancer Control 2006;13:264-9. [PubMed]
- De Perrot M, Fischer S, Bründler MA, et al. Solitary fibrous tumors of the pleura. Ann Thorac Surg 2002;74:285-93. [PubMed]
- Magdeleinat P, Alifano M, Petino A, et al. Solitary fibrous tumors of the pleura: clinical characteristics, surgical treatment and outcome. Eur J Cardiothorac Surg 2002;21:1087-93. [PubMed]
- Sung SH, Chang JW, Kim J, et al. Solitary fibrous tumors of the pleura: surgical outcome and clinical course. Ann Thorac Surg 2005;79:303-7. [PubMed]
- Lu C, Ji Y, Shan F, et al. Solitary fibrous tumor of the pleura: an analysis of 13 cases. World J Surg 2008;32:1663-8. [PubMed]
- Harrison-Phipps KM, Nichols FC, Schleck CD, et al. Solitary fibrous tumors of the pleura: results of surgical treatment and long-term prognosis. J Thorac Cardiovasc Surg 2009;138:19-25. [PubMed]


