Complex multimodality central airway management of aspergillus pseudomembranous tracheobronchitis
Introduction
Invasive tracheobronchial infection with Aspergillus is an extremely serious clinical condition with its pseudomembranous tracheobronchitis (PTB) variant being the most lethal even after appropriate and timely treatment with antifungals. Central airway obstruction due to adherent and extremely hard to remove pseudomembranes adds to the clinical complexities. We describe a challenging case of PTB where step-wise multimodality complex airway treatment played a vital role in achieving desired clinical outcome.
Case presentation
A 69-year-old woman with diffuse large B-cell lymphoma and Sjogren’s syndrome was hospitalized for recurrent pneumonias in the setting of neutropenia two months after completing chemotherapy. She had received six cycles of dose adjusted EPOCH (Etoposide, Prednisone, Vincristine, Cyclophosphamide, Doxorubicin) with Rituximab. The patient was also on hydrocortisone 10 mg in morning and 5 mg in evening for adrenal insufficiency diagnosed 6 weeks prior to presentation. CT chest showed consolidation in bilateral lower lobes and a soft tissue density in the right main stem bronchus with significant narrowing (Figure 1). She didn’t improve with multiple courses of antibiotics including appropriate coverage for Pseudomonas aeruginosa found in sputum and therefore a flexible bronchoscopy was requested. The patient had also developed significant dyspnea by this time and hypoxemia requiring 4 liters of supplemental oxygen. Flexible bronchoscopy revealed yellowish thick adherent membranes in the right main stem with 75% occlusion extending up to bronchus intermedius (Figure 2A). The areas below the level of obstruction were severely inflamed with purulent thick secretions. Attempts to debulk the lesion with Argon Plasma Coagulation (APC) and biopsy forceps met with limited success. The patient was thus intubated with a 10 mm outer diameter (OD) Bryan-DumonTM rigid bronchoscope (small OD scope was used as her overall airway size was small) and the stenotic area was dilated with Controlled radial expansion (CRETM) pulmonary balloon dilator (Boston Scientific, Natick, MA) size 8-9-10 mm up to 9 mm (Figure 2B). Debulking with biopsy forceps (Figure 2C) and balloon dilatation restored patency to the right main stem (Figure 2D). Biopsies of these abnormal areas showed significant acute inflammation and necrosis with fungal organisms consistent with Aspergillus. A diagnosis of Aspergillus PTB with central airway obstruction was made and the patient was started on oral Voriconazole 250 milligram twice a day along with intravenous immune globulin for hypogammaglobulinemia.

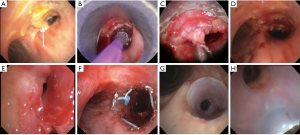
A repeat flexible bronchoscopy was performed 4 weeks later to reassess the impact of therapy. This revealed significant worsening of the central airway stenosis with diffuse yellow thick adherent lesion almost completely obstructing the right main stem bronchus. This was extremely challenging as both the therapeutic flexible and even the pediatric bronchoscopes couldn’t be advanced through this area of narrowing. Additionally biopsy forceps was not helpful in achieving any degree of debulking. Therefore patient was intubated with 10 mm OD Bryan-DumonTM rigid bronchoscope and some debulking was performed using a combination of APC, biopsy forceps and rigid bronchoscope. The stenotic area was initially dilated with a 5 French Fogarty catheter. Then sequential dilatation of right main stem was performed with 8 mm OD rigid bronchoscopes along with a size 8-9-10 CRE pulmonary balloon catheter. Only the proximal right main stem was dilated with the 8 mm OD rigid bronchoscope with inability to advance further distally to the distal right main stem and bronchus intermedius. The right upper lobe opening was also 90% occluded (Figure 2E) and was dilated with 5 French Fogarty catheter. Placement of a peripheral 10-7-7 mm Y silicone stent customized for the right upper lobe opening was attempted several times to maintain patency of right upper lobe along with right main stem with no success due to significant generalized inflammation causing narrowed and abnormal angled right upper lobe opening. Finally, the patient was intubated with a rigid bronchoscope 10 mm OD and an 8 mm × 15 mm covered metallic (hybrid) AERO stent (Alveolus, Inc., NC, USA) was placed in the right main stem (Figure 2F) to maintain patency of the right main stem and to achieve potential dilatation over time due to the radial expansive force of the stent. In addition to increasing the dose of oral Voriconazole to 300 mg twice a day, the patient was also started on 25 mg of aerosolized Amphotericin B once a day. The patient remained on her usual regimen of antihypertensive medications, proton pump inhibitors and maintenance hydrocortisone.
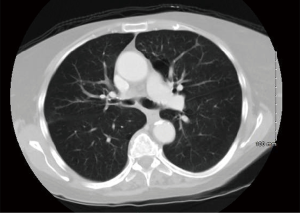
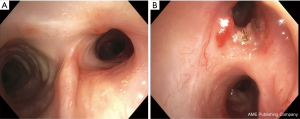
Flexible bronchoscopy was repeated 2 weeks later. The patient had again developed worsening of dyspnea. The right main stem patency was maintained by the stent but the right upper lobe bronchus had almost completely occluded with a barely <4 mm opening. The patient was intubated with 10 mm OD rigid bronchoscope and the AERO stent was removed. The right main stem bronchus maintained better luminal patency as compared to that observed during the previous bronchoscopy likely due to the AERO stent. The right upper lobe opening was sequentially dilated to 8 mm using a 2 mm × 6 mm biliary balloon, a 7 French Fogarty catheter, and a 2 mm × 8 mm biliary balloon respectively. The right main stem and bronchus intermedius were dilated to 10 mm using an 8-9-10 mm CRETM balloon. A customized 10-7-7 mm Y silicone stent (Lengths: right main stem—15 mm, bronchus intermedius—5 mm and right upper lobe—5 mm) without studs (Hood Laboratories, Pembroke, MA) was then successfully deployed as the right main stem was more patent and allowed us to overcome the technical difficulties that we encountered earlier (Figure 2G,H). The patients’ symptoms improved significantly after placement of the peripheral Y stent. Follow up CT showed patent airways (Figure 3) and surveillance bronchoscopies performed at monthly intervals twice did not show any evidence of recurrent central airway stenosis. The peripheral Y stent was removed after one year without any evidence of abnormal infected mucosa underneath and the pseudomembranes had completely resolved. The right-sided involved airway had developed fibrosis and some stenosis but still maintained its patency at approximately 70% of the original size (Figure 4) and this was also noted on subsequent CT of the chest (Figure 3). The patient completed one year of oral Voriconazole therapy and remained asymptomatic with good performance status without any further clinical deterioration or recurrence of infection.
Discussion
Aspergillus is a ubiquitous fungus and the aerosolized spores frequently get inhaled and get deposited in the human airways. In healthy people, innate immunological and mucociliary defenses effectively eliminate the spores. However invasive aspergillosis can be seen in people with defective immunity like those with neutropenia, hematological malignancies, organ transplant, diabetes mellitus, long-term corticosteroid use etc. Similarly this condition can also be encountered in those with structural lung disease and defective mucociliary mechanism like those with chronic obstructive lung disease and sarcoidosis (1). A small fraction of patient (approximately 10%) with invasive aspergillosis may be immunocompetent. Aspergillus can cause invasive tracheobronchial disease, which ultimately requires a bronchoscopy for diagnosis and tracheobronchial invasive involvement is subcategorized into ulcerative, obstructive and pseudomembranous variants (1). Pseudomembrane tracheobronchitis (PTB) is caused by invasion of tracheobronchial mucosa by aspergillus with necrosis and sloughing off of tissue into airway and is the variant with the most aggressive clinical course and a high fatality rate in spite of treatment and irrespective of immune status of the patient (2-4). Currently there is no system of classification of severity of PTB but literature suggests that the subgroup the patients who require mechanical ventilation have the lowest chance of survival (3,4). As the obstructing pseudomembranes may be responsible for poor antifungal penetration and also for development of respiratory failure, therefore maintaining the patency of the central airway to prevent progressive respiratory failure and allowing more time for the antifungal medications to work may be an extremely critical factor in such patients.
Our case demonstrates several complexities of management of central airway obstruction of the patients with PTB. First of all, our patients had genetically smaller airways making them more prone to be completely obstructed with tissue debris and we had to use relatively smaller rigid bronchoscope and smaller balloons to dilate the airway including the use of Fogarty catheters and biliary balloons. Understanding the utility of accessories available with our gastroenterology colleagues was helpful. Secondly the difficulty in removal of extensive thick and sticky obstructive debris is well described. Even thermal techniques like APC, electrocautery, laser and cryotherapy may not work well as seen in this case although combination with rigid bronchoscopic debulking was helpful. Thirdly, extreme caution needs to be exercised when removing these membranes as patient death has been reported from massive pulmonary artery bleed during removal of obstructive infective tissue (5). Careful review of CT imaging may be of some help to know the relationship of involved airway with major blood vessels and to assess the risk of major bleeding. Additional imaging modalities like CT pulmonary angiography, digital subtraction angiography and endobronchial ultrasound or interventions like embolization prior to bronchoscopic procedures in high risk cases may be helpful but have not been well described in literature. We cautiously removed some debris to obtain the patency of right main stem and placed an AERO hybrid stent to slowly dilate the right main stem over several days, as we were not able to initially place a peripheral Y stent, which could have allowed us to maintain the patency of right upper lobe. Fourthly, there is limited literature on the appropriate selection of airway stents for PTB. The deployment of metallic or hybrid airway stent has been reported in post-transplant tracheobronchial stump stenosis due to aspergillus infection (2,6). The use of silicone stents has been described only on rare occasions in the setting of Aspergillus tracheobronchial infection including one case for airway stenosis after treatment of bronchomediastinal fistula and another for post-tuberculosis tracheal stricture with superimposed PTB (7,8). Finally, the issue of placing an airway stent in the setting of infection is a subject of debate (8). Pornsuriyasak et al. described a case of PTB superimposed on post-tubercular tracheal stricture. They dilated the trachea with rigid bronchoscope and avoided placing a stent in the setting of acute infection. The patient showed clinical improvement flexible bronchoscopy a week later showed improved pseudomembranes. The patient developed recurrent tracheal stricture in the absence of PTB and a silicone stent was placed. In our case, the patient likely had more severe and more extensive PTB and there was clinical deterioration in spite of appropriate antifungal therapy and there was no choice but to place a stent to prevent further worsening of respiratory status. The obstructive exudates still progressed and obstructed the right upper lobe with clinical deterioration but the hybrid stent kept the right main stem bronchus patent. This also possibly allowed us to achieve some slow right main stem dilatation and finally placement of a peripheral silicone Y stent. Finally, to the best of our knowledge, a peripheral Y stent has never been placed in the setting of PTB and was an additional unique and challenging aspect of this case. The techniques of peripheral Y stents have been described previously (9,10) but usual anatomical factors can pose significant challenges in deployment (11). We were able to successfully deploy a peripheral Y stent even in the setting of diffuse airway obstruction by PTB. This was not only associated with immediate clinical improvement but also allowed the antifungal therapy to take effect thus allowing our patient a better chance at survival.
In summary, we describe the challenges faced in the complex multimodality management of central airway obstruction of a patient with PTB. We believe that thoughtful, cautious and determined airway management may help in slowing the clinical deterioration of this aggressive airway infection, which may offer a chance of improved survival to some patients.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Patterson KC, Strek ME. Diagnosis and treatment of pulmonary aspergillosis syndromes. Chest 2014;146:1358-68. [Crossref] [PubMed]
- Karnak D, Avery RK, Gildea TR, et al. Endobronchial fungal disease: an under-recognized entity. Respiration 2007;74:88-104. [Crossref] [PubMed]
- Li Y, Yu F, Parsons C, et al. Pseudomembranous Aspergillus tracheobronchitis: a potential for high mortality in low-risk patients. Am J Med Sci 2013;346:366-70. [Crossref] [PubMed]
- Tasci S, Glasmacher A, Lentini S, et al. Pseudomembranous and obstructive Aspergillus tracheobronchitis - optimal diagnostic strategy and outcome. Mycoses 2006;49:37-42. [Crossref] [PubMed]
- Putnam JB Jr, Dignani C, Mehra RC, et al. Acute airway obstruction and necrotizing tracheobronchitis from invasive mycosis. Chest 1994;106:1265-7. [Crossref] [PubMed]
- Xie BX, Zhu YM, Chen C, et al. Outcome of TiNi stent treatments in symptomatic central airway stenoses caused by Aspergillus fumigatus infections after lung transplantation. Transplant Proc 2013;45:2366-70. [Crossref] [PubMed]
- Argento AC, Wolfe CR, Wahidi MM, et al. Bronchomediastinal fistula caused by endobronchial aspergilloma. Ann Am Thorac Soc 2015;12:91-5. [Crossref] [PubMed]
- Pornsuriyasak P, Murgu S, Colt H. Pseudomembranous aspergillus tracheobronchitis superimposed on post-tuberculosis tracheal stenosis. Respirology 2009;14:144-7. [Crossref] [PubMed]
- Oki M, Saka H, Kitagawa C, et al. Silicone y-stent placement on the carina between bronchus to the right upper lobe and bronchus intermedius. Ann Thorac Surg 2009;87:971-4. [Crossref] [PubMed]
- Oki M, Saka H. Silicone Y-Stent Placement on the Secondary Left Carina. Respiration 2015;90:493-8. [Crossref] [PubMed]
- Harris K, Dhillon SS, Alraiyes AH. Personalized bronchial stent therapy. Ann Am Thorac Soc 2015;12:451-4. [Crossref] [PubMed]


