SIRS, qSOFA and new sepsis definition
A 2016 task force convened by national societies including the Society of Critical Care Medicine (SCCM) and the European Society of Intensive Care Medicine (ESICM) proposed a new definition of sepsis, termed Sepsis-3 (1). The new proposal defines sepsis as life-threatening organ dysfunction caused by a dysregulated host response to infection (1-3). The new definition abandoned use of host inflammatory response syndrome criteria (SIRS) in identification of sepsis and eliminated the term severe sepsis. An earlier sepsis definition, Sepsis-1, was developed at a 1991 consensus conference (4) in which SIRS criteria were established. Four SIRS criteria were defined, namely tachycardia (heart rate >90 beats/min), tachypnea (respiratory rate >20 breaths/min), fever or hypothermia (temperature >38 or <36 °C), and leukocytosis, leukopenia, or bandemia (white blood cells >1,200/mm3, <4,000/mm3 or bandemia ≥10%). Patients who met two or more of these criteria fulfilled the definition of SIRS, and Sepsis-1 was defined as infection or suspected infection leading to the onset of SIRS. Sepsis complicated by organ dysfunction was termed severe sepsis, which could progress to septic shock, defined as “sepsis-induced hypotension persisting despite adequate fluid resuscitation.” A 2001 task force (5) recognized the limitations with these definitions, but did not offer alternatives due to a lack of supporting evidence. However, they did expand the list of diagnostic criteria, resulting in the introduction of Sepsis-2. Therefore, in order to be diagnosed with sepsis under the Sepsis-2 definition, as with Sepsis-1, an individual must have at least 2 SIRS criteria and a confirmed or suspected infection (4-6). In effect, the definitions of sepsis and septic shock remained unchanged for more than two decades.
As part of the 2016 SCCM/ESICM evaluation of criteria for identifying septic patients, the task force compared traditional SIRS criteria to other methods, including the Logistic Organ Dysfunction System (LODS) and Sequential Organ Failure Assessment (SOFA) scoring. Based on this analysis, the authors recommended use of SOFA scoring to assess the severity of organ dysfunction in a potentially septic patient (Table 1). The predictive validity of SIRS criteria and SOFA scoring for mortality in sepsis patients were compared by analyzing health record data from the University of Pittsburgh and Kaiser Permanente databases (3). Among critically ill patients with suspected sepsis, the predictive validity of the SOFA score for in-hospital mortality was superior to that of the SIRS criteria (area under the receiver operating characteristic curve 0.74 versus 0.64). Patients who fulfill SOFA score have a predicted mortality of ≥10%. Although the predictive capacity of SOFA and LODS were similar, SOFA is considered easier to calculate, and was therefore recommended by the task force (1-3). Other studies have supported the idea that SIRS is not an ideal marker for sepsis. Kaukonen et al. (8) evaluated the presence of SIRS criteria in 109,663 patients with infection and organ failure. In this study, 12% of patients were classified as having SIRS-negative sepsis (i.e. <2 SIRS criteria). Furthermore, SIRS criteria are present in many hospitalized patients, including those who never develop infection and never incur adverse outcomes (9,10).
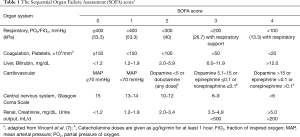
Full table
Use of SOFA scoring in clinical trials is already commonly performed and constitutes a routine component of data collection for clinical trials in the intensive care unit (ICU). However, the complexity of the method, the lack of requisite data for many patients, and concerns that it may result in late identification relative to other methods raise the possibility that its use according to the Sepsis-3 method may prove impractical in clinical practice. Recognizing these practical limitations, the 2016 SCCM/ESICM task force described a simplified method termed “quick SOFA” to facilitate easier identification of patients potentially at risk of dying from sepsis (1-3). This score is a modified version of the Sequential (Sepsis-related) Organ Failure Assessment score (SOFA). qSOFA consists of only three components that are each allocated one point (Table 2). A qSOFA score of ≥2 points indicates organ dysfunction.
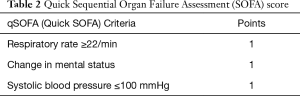
Full table
Criticism of these new methods does exist and data has emerged illustrating the limitations of the new definitions, particularly in early detection of sepsis. Williams et al. (11) recently carried out a prospective database study in a tertiary Australian medical center that aimed to determine the prognostic impact of SIRS and compare the diagnostic accuracy of SIRS and qSOFA. In this study of 8871 emergency room patients, of whom 4,176 (47.1%) had SIRS, SIRS was associated with an increased risk of organ dysfunction (RR 3.5) and mortality in patients without organ dysfunction (OR 3.2). SIRS and qSOFA showed similar discrimination for organ dysfunction (AUROC 0.72 vs. 0.73). qSOFA was specific but poorly sensitive for organ dysfunction (96.1%, 29.7% respectively). Another study in Greece where 3346 infections outside the ICU and 1,058 infections in the ICU were analyzed, qSOFA score provided inadequate sensitivity for early risk assessment (12). This clearly shows that use of qSOFA score risks missing early identification of sepsis when treatment is most effective. Prognostic accuracy for in-hospital mortality between SIRS criteria and qSOFA score is area of debate. A new large retrospective cohort analysis among 184,875 patients in 182 Australian and New Zealand intensive care units (ICUs) found SOFA score had superiority in prediction of in-hospital mortality but it showed SIRS criteria has greater prognostic accuracy for in-hospital mortality than qSOFA score (13). Other Emergency room study among 879 patients presenting to the emergency department with suspected infection found the use of qSOFA resulted in greater prognostic accuracy for in-hospital mortality than did either SIRS or severe sepsis (14).
The overall effect of the 2016 SCCM/EISCM task force recommendations is elimination of the concept of sepsis without organ dysfunction, redefinition of the clinical criteria for identifying genuine sepsis cases, and redefinition of the clinical criteria for septic shock. This is likely to improve accuracy of sepsis epidemiology and hospital coding and may improve outcomes.
The introduction of the Sepsis-3 definition is still relatively new to the critical care literature, but given the ease of SOFA calculation and high specificity of SOFA/qSOFA scores, it is likely to be adopted as a consensus definition for future clinical research. However, as highlighted by Williams et al. (11), one limitation of the new definition is the poor sensitivity of the qSOFA scoring system, which likely excludes its use as a screening tool for early sepsis, the stage in which treatment is most effective. Although SOFA score has the most prognostic accuracy for in-hospital mortality but which one SIRS criteria or qSOFA score has more prognostic accuracy of mortality is not clear yet and it needs more research. In addition, many healthcare facilities currently use the previous sepsis definition as part of emergency room and ICU protocol and implementation of the new recommendations will require funding to facilitate amendment of protocols and retraining of healthcare providers.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Singer M, Deutschman CS, Seymour CW, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016;315:801-10. [Crossref] [PubMed]
- Shankar-Hari M, Phillips GS, Levy ML, et al. Developing a New Definition and Assessing New Clinical Criteria for Septic Shock: For the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016;315:775-87. [Crossref] [PubMed]
- Seymour CW, Liu VX, Iwashyna TJ, et al. Assessment of Clinical Criteria for Sepsis: For the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016;315:762-74. [Crossref] [PubMed]
- Bone RC, Balk RA, Cerra FB, et al. Definitions for Sepsis and Organ Failure and Guidelines for the Use of Innovative Therapies in Sepsis. Chest 1992;101:1644-55. [Crossref] [PubMed]
- Levy MM, Fink MP, Marshall JC, et al. 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit Care Med 2003;31:1250-6. [Crossref] [PubMed]
- Peach BC. Implications of the new sepsis definition on research and practice. J Crit Care 2017;38:259-62. [Crossref] [PubMed]
- Vincent JL, Moreno R, Takala J, et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med 1996;22:707-10. [Crossref] [PubMed]
- Kaukonen KM, Bailey M, Pilcher D, et al. Systemic inflammatory response syndrome criteria in defining severe sepsis. N Engl J Med 2015;372:1629-38. [Crossref] [PubMed]
- Whippy A, Skeath M, Crawford B, et al. Kaiser Permanente's performance improvement system, part 3: multisite improvements in care for patients with sepsis. Jt Comm J Qual Patient Saf 2011;37:483-93. [Crossref] [PubMed]
- Churpek MM, Zadravecz FJ, Winslow C, et al. Incidence and Prognostic Value of the Systemic Inflammatory Response Syndrome and Organ Dysfunctions in Ward Patients. Am J Respir Crit Care Med 2015;192:958-64. [Crossref] [PubMed]
- Williams JM, Greenslade JH, McKenzie JV, et al. SIRS, qSOFA and organ dysfunction: insights from a prospective database of emergency department patients with infection. Chest 2017;151:586-596. [Crossref] [PubMed]
- Giamarellos-Bourboulis EJ, Tsaganos T, Tsangaris I, et al. Validation of the new Sepsis-3 definitions: proposal for improvement in early risk identification. Clin Microbiol Infect 2017;23:104-9. [Crossref] [PubMed]
- Raith EP, Udy AA, Bailey M, et al. Prognostic accuracy of the sofa score, sirs criteria, and qsofa score for in-hospital mortality among adults with suspected infection admitted to the intensive care unit. JAMA 2017;317:290-300. [Crossref] [PubMed]
- Freund Y, Lemachatti N, Krastinova E, et al. Prognostic Accuracy of Sepsis-3 Criteria for In-Hospital Mortality Among Patients With Suspected Infection Presenting to the Emergency Department. JAMA 2017;317:301-8. [Crossref] [PubMed]


