The management of the advanced colorectal cancer: management of the pulmonary metastases
Introduction
During last two decades there have been such significant advances in surgical oncology that surgical interventions considered ineffective, unnecessary or even dangerous, can now be successfully performed not only for palliation, but in order to improve the prognosis, and secure better survival and better quality of life. In this change the evolution of imaging, medical oncology, and surgical techniques played a major role. Thus, this change has been produced by the attitude of team approach and interdisciplinary collaboration.
An important development is the introduction of PET, which can detect metabolically active metastatic disease (with reduced sensitivity when the lesions are less than 9 mm). The new generations of CT and MRI scanners can give more precise information on the location and extent of the disease, while the targeted oncology treatments can achieve improved responsiveness, so that the resection of the lesion turns to be possible. The combination of surgical resection with new cytotoxic drugs such as oxaliplatin, irinotecan and bevacizumab can ensure long survival in the majority of patients, and even permanent cure in a small proportion of them (1).
On the other hand, there has been an excellent progress in surgical techniques with the introduction of laparoscopic and thoracoscopic techniques. These allow the diagnosis and treatment of primary and metastatic disease with minimal surgical trauma, no risk of cancer dissemination and faster patient recovery with the possibility of adjuvant treatment shortly after surgery, while the patient develops less immunosuppression (2).
General principles
The presence of systemic metastases usually predisposes to poor prognosis in cancer patients. Nevertheless, limited lung metastases do not mean that the patient is beyond rescue possibility. By controlling the primary tumor and in the absence of disseminated disease in many organs, the resection of pulmonary metastases may prolong survival, improve the quality of life and in some cases to ensure cure.
In 1947 Alexander and Haight published series of pulmonary metastasectomies and were the first to describe aggressive control of metastatic disease in the chest by carrying successive metastectomies. They still are leaders to the description of the most established criteria in relation to pulmonary metastases: (I) Control primary tumor; (II) Absence of extra thoracic disease and (III) Sufficient pulmonary reserve (3).
Selected patients with colorectal cancer metastatic to the liver and lungs can benefit from metastasectomy. Generally, patients with resectable pulmonary metastases can achieve with surgery 5-year survival nearly 30% (4), although in other series the survival reaches levels greater than 50%.
The majority of patients with pulmonary metastases have non-resectable locally advanced disease or concurrent metastases to other organs, which excludes therapeutic metastasectomy. In autopsy series of patients who died from extrathoracic malignancies, 20-50% had pulmonary metastasis when died (5). Among these patients, 10% to 15% had metastatic disease limited to the lungs. Resectability rates in these patients is low and only 1% of these patients have resectable disease. The number of metastases varies depending on the histology of the primary tumor. Patients with osteosarcomas and soft tissue sarcomas are more likely to have solitary pulmonary metastases than patients with colon or breast cancer.
Pathophysiology
The majority of pulmonary metastases considered to be derived from cancer cells that enter the lungs through the pulmonary arteries and disperse in alveolar capillaries. Although most of these cancer cells are able to adhere to the endothelium of the capillaries, the cell survival is ultimately determined by local and oncology factors. Apparently most of these malignant cells do not survive. Those that survive penetrate the endothelium of the capillaries and install in the pulmonary parenchyma, where they form parenchymal pulmonary localizations. After installation in the parenchyma, they can be further developed either locally or extensively invading pleura, chest wall or mediastinum.
Rarely, pulmonary metastases occur as a consequence of lymphatic spreading. In this case, the cells derived from the primary tumor, extend to regional lymph nodes and continue to the lymphatic of the lung. It follows a retrograde extension from pulmonary and hilar lymph to the lung parenchyma. Invasion of mediastinal lymph nodes is seen more frequently in melanoma, breast, colon, and kidney cancer (4).
Metastases yet can be developed directly in the bronchial tree. The autopsy series show 18% with disease that affects the bronchi, but less than 3% of patients have disease in primary, lobar or segmental bronchi accessible to bronchoscopic evaluation and identification. Cough and hemoptysis was the usual symptoms, while there was no predisposition to a specific part of the bronchial tree, although some consider frequent location the upper lobe (4).
However, as most pulmonary metastases are asymptomatic, their diagnosis occurs either at first diagnostic investigation on the occasion of primary tumor’s discovery, either in follow-up work-up after treatment of the primary tumor. Cough, pain and hemoptysis are symptoms of hilar localization, especially when metastases are compressing or infiltrating bronchus. When metastasis has peripheral localization rarely pneumothorax may occur because of disruption of visceral pleura.
Management of metastases from colorectal cancer
The colon cancer disperses either locally or systemically in the liver and lungs. The appearance of pulmonary nodules in patients with a history of colon cancer requires a thorough study of extrapulmonary metastatic sites, with particular attention to the liver. Levels of carcinoembryonic antigen (CEA) is necessary to be examined. If presence of other metastatic lesions is excluded, patients with solitary pulmonary localizations can undergo surgical resection with good results.
Pulmonary metastases in this type of cancer are observed in 10-20% of all patients (6). Unfortunately, pulmonary metastases without extrathoracic disease are even less common, and only 1% of all patients will fulfill the criteria resectability of Alexander and Haight (3,7). It is characteristic that in Pastorino’s series it was the second most common cancer (6).
In the results of the series of Memorial Sloan-Kettering it was demonstrated that total resection was the only significant variable (8). In this series of 144 selected patients treated with pulmonary metastasectomy, the 5-year survival was 44% and the ten-year 25%. Chemotherapy alone for colorectal metastases in the lung without metastasectomy, had no survival beyond 24 months (8).
Because of the good results published from aggressive treatment of hepatic and pulmonary metastases with surgical excision, such an approach is worthy in selected patients, due to failure to achieve cure with chemotherapy based on the 5-fluorouracil (9).
Significant favorable prognostic factors predisposing to better survival are the presence of a solitary metastasis, disease-free interval greater than 36 months, and normal preoperative CEA level. Survival rates were better in patients without hilar or mediastinal lymph node invasion, while patients who had previously undergone resection of liver metastases did not differ significantly on the survival from patients without previous liver disease (10).
Even in series with repetitive lung metastasectomies, in cases where removal of liver metastasis had to be done the five-year survival was recorded up to 43%, while when there was no liver participation reached 60% (11). The prognosis of pulmonary metastases 12 months or more after hepatic metastasectomy is similar to that observed in patients without liver metastases (12). An important parameter that differentiates the prognosis is whether the existence—and surgery—of hepatic and pulmonary metastasis is synchronous or metachronous: the metachronous hepatic and pulmonary resection has significantly better survival compared to the synchronous (13,14).
The current interest is focused on the prognostic evaluation of histopathologic features. More specifically the size of metastases, the presence of floating cancer cell clusters, the bronchial, vascular, lymphatic or pleural infiltration and lymph node invasion have been studied (15). Furthermore, the existence of histological type different than the well differentiated adenocarcinoma appears to be unfavorable prognostic factor (16).
The introduction of a new generation of chemotherapeutic agents and targeted therapies has made it possible to improve survival in patients with metastatic colorectal cancer. The use of these agents is promising for patients with resectable pulmonary metastases, since a significant proportion of patients have complete or partial response to chemotherapy, which greatly facilitates the action of the surgery that follows.
It is also noteworthy that the practice of repeated pulmonary resections for recurrent pulmonary metastases is well documented and indicated as effective treatment from the literature. Important prognostic factor in repeat resections has proven to be the hilar or mediastinal lymph node infiltration. For this reason, it has been emphasized the importance of preoperative evaluation of lymph nodes on both the first and the recurrent pulmonary metastasectomies. The aggressive repetitive resection is justified in carefully selected patients (16).
In a retrospective multicenter study of 19 Japanese centers, it has been demonstrated that in patients undergoing total resection of lung metastases from colorectal cancer, significant predictors of adverse survival are stage T4 for primary site and the presence of N2 disease, metastases number higher than 3, bilateral distribution of pulmonary lesions, disease-free interval of less than 2 years, and CEA levels greater than 5 ng/mL before resection. As a consequence, indications for metastasectomies is proposed to be made with consideration of the T and N primary tumor, level of CEA, and disease free survival (17). Other parameters that need to be taken into account, in addition to CEA, according to another retrospective multicenter study of 26 Japanese centers, are the number of metastases, the size, the radical resection and the nodal attack (18). Additionally, as influencing factors are also suggested induction chemotherapy (19), intravascular microemboli during histopathological examination (20), age and male gender (21). Chemotherapy is considered to favorably influence the survival without causing increased operative complications (22).
The doubling time has been described in many tumors as parameter for development and progression of malignancy. This size certainly plays an important role in the development of lung metastases from colorectal cancer. One way of tracking doubling time is proposed by execution in regular intervals CT scans to have information through volumetric analysis of larger pulmonary nodule, which is presumed to be the first pulmonary metastasis (23).
A meta-analysis of the recently published surgical treatment series of lung metastases from colorectal cancer between 2001-2011 with more than 40 patients each suggested that the factors correlated with increased survival is prolonged disease free interval between the primary tumor and metastatic spread, normal CEA before thoracotomy, absence of lymph nodes filtration in the chest, and solitary lung lesion (24).
Treatment requirements
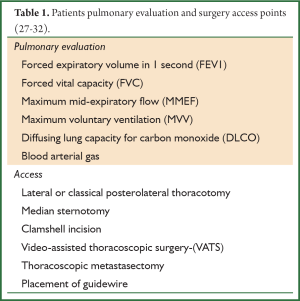
It is necessary to check the patient’s cardiorespiratory reserves in order to confirm the suitability for the surgery scheduled. It is important to assess cardiac function, the presence of coronary heart disease or valvulopathy, and evaluate respiratory functional reserves in the pulmonary functional tests, including spirometry for forced vital capacity (FVC), forced expiratory volume in the first second (FEV1), maximum mid-expiratory flow (MMEF), maximum voluntary ventilation (MVV), diffusing lung capacity for carbon monoxide (DLCO) and arterial blood gases. Lung perfusion ventilation scanning may be necessary depending upon the extent of the scheduled resection and the pulmonary function of the patient (25).
Access and type of resection
Access
Most surgeons prefer the lateral or classical posterolateral thoracotomy, preferably sequentially in successive operations to treat bilateral lesions, although others prefer median sternotomy ensuring easy access to the lungs, with the exception of the left lower lobe. Another option in open access is anterior transverse thoracotomies with or without transverse opening of the sternum (clamshell incision), with which it is easy to have access in both lungs at once, with very good aesthetic result for women due to localization of the incision in the submammary line, but with large traumatic surfaces (26). Recent publication highlighted the role of bilateral posterior thoracotomy at the same time for metastases with posterior peripheral localization (27). Much interest has been developed on thoracoscopic accesses (video-assisted thoracoscopic surgery-VATS), which are preferred due to less pain and better cosmetic effect, but invite criticism due to impossibility of localization of all existing metastatic lesions that are not shown in the preoperative investigation because of small size, as finger palpation is absent. In a prospective study of McCormack and collaborators from the Memorial Sloan-Kettering Cancer Center 15 patients underwent thoracoscopic metastasectomy of nodules revealed on chest CT. However, on the same patients malignant nodules were found in 56% (10/18) with additional thoracotomy that were not visualized on the CT scan or were not apparent by the VATS resection. This study has provided a strong argument against the VATS and stopped prematurely after recording 18 patients, because statistically significant benefit was in favor of thoracotomy (28). But, this series used old technology CT scanners with reduced ability to detect metastases. It is considered that with the helical scan of the new generation, accuracy can be increased. Moreover, according to recent work, both open access by thoracotomy and the thoracoscopy are anyway imperfect interventions, while finger palpation plays a limited role in improving the clinical outcome in patients with pulmonary metastasis from colorectal cancer (29). That is why the thoracoscopic surgery is considered justified, because in thoracotomy all metastatic foci are not removed, while existing published series show no survival difference between the two techniques (30).
Great assistance to the exact location of the node through thoracoscopic access is provided by placement of guidewire to the nodule on CT before metastasectomy, radiolabeled microspiral needle or platinum, marking with methylene blue, palpation of the finger through one of the holes of assisted thoracoscopy intervention, as well as utilization of technology of ultrasound intraoperatively (31). Furthermore, there has been tested three dimensional reconstruction of the image of the lung on computer tomography, with the vessels, the bronchial tree, the anatomical parts and the tumor in order to “map” with precision the surgical dissection of metastasis (32) (Table 1).
Relapse
More than half of patients develop metastatic disease after metastasectomy. The re-resection of metastases is a practice well established and can be repeated in some cases (16). In published series up to 4 times lung metastasectomies have been reported (11). Repetitive metastasectomy after VATS can be done again through thoracoscopic access (29).
Type of resection
Regarding the type of resection, the wedge resection or atypical resection is surgery of choice in pulmonary metastases combined with systemic lymphadenectomy of the mediastinal lymph nodes. Considering that in series the mediastinal lymph node metastasis is becoming steadily significant predictor (sometimes even the only one), systematic lymphadenectomy is imperative. It is remarkable that both the CT scan, and the CEA, but the PET also have a low sensitivity in the detection of mediastinal lymph node metastases (only 35% for PET), which makes surgical staging of mediastinal lymph nodes absolutely necessary (33).
Larger or centrally localized tumors may require lobectomy or bilobectomy. The pneumonectomy should be performed in exceptional cases, when it cannot be prevented by bronchoplastic/angioplastic lung preserving techniques. The use of laser provides the possibility of lung parenchyma preserving by excision of the central and multiple metastases. Extensive resections with resection of the chest wall, diaphragm, pericardium, atrium or vena cava may be performed when appropriate and not contraindicated. However, in surgery of metastases, we should always choose the technique that preserves the greatest amount of pulmonary parenchyma to make feasible further resection in the future, in case of local recurrence (26,34).
Tissue vaporization with RF (radiofrequency ablation-RFA)
The mechanism of radiofrequency action consists in the stimulation of ions, the cauterization of tissue and its necrosis at the end. The method was first used for the treatment of primary liver tumors.
The principle is based on the temperature increase into the liver tumors. Today there is the possibility of creating hyperthermic foci >1.5-2 cm in diameter by entering only one needle into the lesion.
The estimated three-year survival with the application of the method is about 50% (35).
Prognostic factors include the existence of extrapulmonary metastases and tumor size undergoing RFA.
In small metastases (<3 cm) and absence of extrapulmonary sites the three-year survival is approximately 78%.
The selection criteria for application of the method are the following:
- Primary tumor controlled or controllable;
- Helical scan with thin slices on computed tomography;
- Limited number of metastases (3 or less);
- Tumor of not more than 5 cm;
- Patient inappropriate as surgical candidate;
- Tumors located at the external 2/3 of the lung and not adjacent to the mediastinum;
- Chest disease susceptible to RFA.
Complications of the method are:
- Pneumothorax (40%);
- Pleural effusion (15%);
- Empyema (1%);
- Hemoptysis, pain and cough;
- Pulmonary abscess;
- Residual tumor not damaged. It is reported that the RFA has achieved complete necrosis of the lesion in 91% of tumors with a diameter up to 47 mm, while failure was recorded when the vaporization around the tumor was not sufficient, because of proximity to large vessel (diameter >3 mm). But when RFA was applied by open thoracotomy and a subsequent surgical excision of the lesion was performed, the histopathological examination showed complete necrosis of tumor cells in 38% of cases (36);
- Intrapulmonary recurrence (38-47%). More than half of the patients require repeat application of the method, while the rate of disease progression after RFA is 35%, while in tumors >3 cm the progress can be up to 75%. Major complications are observed in 6%. Size of metastasis >3 cm and CEA >5 ng/mL one month after RFA are factors associated with reduced time free of disease progression (37,38).
In conclusion, for these reasons, this method should be restricted to palliative indications alone, while patients, who fulfill the criteria (oncology and medical) for curative resection, should undergo surgical resection of their pathology (39).
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Gonzalez M, Ris HB, Krueger T, et al. Colorectal cancer and thoracic surgeons: close encounters of the third kind. Expert Rev Anticancer Ther 2012;12:495-503. [PubMed]
- Berger AC. Introduction: role of surgery in the diagnosis and management of metastatic cancer. Semin Oncol 2008;35:98-9. [PubMed]
- Alexander J, Haight C. Pulmonary resection for solitary metastatic sarcomas and carcinomas. Surg Gynecol Obstet 1947;85:129-46. [PubMed]
- Quiros RM, Scott WJ. Surgical treatment of metastatic disease to the lung. Semin Oncol 2008;35:134-46. [PubMed]
- Crow J, Slavin G, Kreel L. Pulmonary metastasis: a pathologic and radiologic study. Cancer 1981;47:2595-602. [PubMed]
- Pastorino U, Buyse M, Friedel G, et al. Long-term results of lung metastasectomy: prognostic analyses based on 5206 cases. The International Registry of Lung Metastases. J Thorac Cardiovasc Surg 1997;113:37-49. [PubMed]
- Sakamoto T, Tsubota N, Iwanaga K, et al. Pulmonary resection for metastases from colorectal cancer. Chest 2001;119:1069-72. [PubMed]
- McCormack PM, Burt ME, Bains MS, et al. Lung resection for colorectal metastases. 10-year results. Arch Surg 1992;127:1403-6. [PubMed]
- Reddy RH, Kumar B, Shah R, et al. Staged pulmonary and hepatic metastasectomy in colorectal cancer--is it worth it? Eur J Cardiothorac Surg 2004;25:151-4. [PubMed]
- Saito Y, Omiya H, Kohno K, et al. Pulmonary metastasectomy for 165 patients with colorectal carcinoma: A prognostic assessment. J Thorac Cardiovasc Surg 2002;124:1007-13. [PubMed]
- Welter S, Jacobs J, Krbek T, et al. Long-term survival after repeated resection of pulmonary metastases from colorectal cancer. Ann Thorac Surg 2007;84:203-10. [PubMed]
- Inoue M, Ohta M, Iuchi K, et al. Benefits of surgery for patients with pulmonary metastases from colorectal carcinoma. Ann Thorac Surg 2004;78:238-44. [PubMed]
- Kawano D, Takeo S, Tsukamoto S, et al. Prediction of the prognosis and surgical indications for pulmonary metastectomy from colorectal carcinoma in patients with combined hepatic metastases. Lung Cancer 2012;75:209-12. [PubMed]
- Zabaleta J, Aguinagalde B, Fuentes MG, et al. Survival after lung metastasectomy for colorectal cancer: importance of previous liver metastasis as a prognostic factor. Eur J Surg Oncol 2011;37:786-90. [PubMed]
- Shiono S, Ishii G, Nagai K, et al. Histopathologic prognostic factors in resected colorectal lung metastases. Ann Thorac Surg 2005;79:278-82; discussion 283. [PubMed]
- Kanzaki R, Higashiyama M, Oda K, et al. Outcome of surgical resection for recurrent pulmonary metastasis from colorectal carcinoma. Am J Surg 2011;202:419-26. [PubMed]
- Hirosawa T, Itabashi M, Ohnuki T, et al. Prognostic factors in patients undergoing complete resection of pulmonary metastases of colorectal cancer: a multi-institutional cumulative follow-up study. Surg Today 2013;43:494-9. [PubMed]
- Iida T, Nomori H, Shiba M, et al. Prognostic Factors After Pulmonary Metastasectomy for Colorectal Cancer and Rationale for Determining Surgical Indications: A Retrospective Analysis. Ann Surg 2013;257:1059-64. [PubMed]
- Marín C, Robles R, López Conesa A, et al. Outcome of strict patient selection for surgical treatment of hepatic and pulmonary metastases from colorectal cancer. Dis Colon Rectum 2013;56:43-50. [PubMed]
- Le Pimpec Barthes F, Fabre-Guillevin E, Foucault C, et al. Lung metastasis surgery, yesterday and now. Rev Mal Respir 2011;28:1146-54. [PubMed]
- Blackmon SH, Stephens EH, Correa AM, et al. Predictors of recurrent pulmonary metastases and survival after pulmonary metastasectomy for colorectal cancer. Ann Thorac Surg 2012;94:1802-9. [PubMed]
- Hawkes EA, Ladas G, Cunningham D, et al. Peri-operative chemotherapy in the management of resectable colorectal cancer pulmonary metastases. BMC Cancer 2012;12:326. [PubMed]
- Poullis M, Littler J, Gosney J. Biology of colorectal pulmonary metastasis: implications for surgical resection. Interact Cardiovasc Thorac Surg 2012;14:140-2. [PubMed]
- Gonzalez M, Poncet A, Combescure C, et al. Risk factors for survival after lung metastasectomy in colorectal cancer patients: a systematic review and meta-analysis. Ann Surg Oncol 2013;20:572-9. [PubMed]
- Brunelli A. Preoperative evaluation of lung resection candidates. Preface. Thorac Surg Clin 2008;18:xi. [PubMed]
- Grunenwald D. Surgery of lung metastasis for colorectal cancer: how far can we push the limits? Proceedings of the Postgraduate Course, 15TH European Conference on General Thoracic Surgery, European Society of Thoracic Surgeons (ESTS), 3 June 2007, Leuven, Belgium, p.9-11.
- Fernández E, Molins L, Fibla JJ, et al. Simultaneous bilateral posterior thoracotomy with the patient in the prone position for resection of bilateral posterior lung metastases. Interact Cardiovasc Thorac Surg 2011;13:437-9. [PubMed]
- McCormack PM, Bains MS, Begg CB, et al. Role of video-assisted thoracic surgery in the treatment of pulmonary metastases: results of a prospective trial. Ann Thorac Surg 1996;62:213-6; discussion 216-7. [PubMed]
- Nakajima J, Murakawa T, Fukami T, et al. Is finger palpation at operation indispensable for pulmonary metastasectomy in colorectal cancer? Ann Thorac Surg 2007;84:1680-4. [PubMed]
- Chao YK, Chang HC, Wu YC, et al. Management of lung metastases from colorectal cancer: video-assisted thoracoscopic surgery versus thoracotomy--a case-matched study. Thorac Cardiovasc Surg 2012;60:398-404. [PubMed]
- Daniel TM. A proposed diagnostic approach to the patient with the subcentimeter pulmonary nodule: techniques that facilitate video-assisted thoracic surgery excision. Semin Thorac Cardiovasc Surg 2005;17:115-22. [PubMed]
- Akiba T, Marushima H, Kamiya N, et al. Thoracoscopic surgery for pulmonary metastases after chemotherapy using a tailor-made virtual lung. Gen Thorac Cardiovasc Surg 2011;59:413-7. [PubMed]
- Hamaji M, Cassivi SD, Shen KR, et al. Is lymph node dissection required in pulmonary metastasectomy for colorectal adenocarcinoma? Ann Thorac Surg 2012;94:1796-800. [PubMed]
- Friedel G. Lung metastasis resections: surgical and technological aspects. Proceedings of the Postgraduate Course, 15TH European Conference on General Thoracic Surgery, European Society of Thoracic Surgeons (ESTS), 3 June 2007, Leuven, Belgium, p.16.
- Petre EN, Jia X, Thornton RH, et al. Treatment of pulmonary colorectal metastases by radiofrequency ablation. Clin Colorectal Cancer 2013;12:37-44. [PubMed]
- Schneider T, Reuss D, Warth A, et al. The efficacy of bipolar and multipolar radiofrequency ablation of lung neoplasms - results of an ablate and resect study. Eur J Cardiothorac Surg 2011;39:968-73. [PubMed]
- Yan TD, King J, Sjarif A, et al. Treatment failure after percutaneous radiofrequency ablation for nonsurgical candidates with pulmonary metastases from colorectal carcinoma. Ann Surg Oncol 2007;14:1718-26. [PubMed]
- von Meyenfeldt EM, Prevoo W, Peyrot D, et al. Local progression after radiofrequency ablation for pulmonary metastases. Cancer 2011;117:3781-7. [PubMed]
- Gillams AR. The use of radiofrequency in cancer. Br J Cancer 2005;92:1825-9. [PubMed]