Comparing American, European and Asian practice guidelines for aortic diseases
Introduction
The aortic disease comprises a group of different pathologies of high prevalence, seriousness and dynamic by the medical and surgical investigations and innovations that are developed day by day in this field.
Cardiovascular scientific societies have created Task Force on Practice Guidelines (PG) to develop, update and revise PG for cardiovascular diseases and procedures. This documents summarize and evaluate all available evidence, on a particular issue with the aim of help the health professionals to make decisions in their daily practice; and PG represent the official position of these societies on a given topic and are regularly updated.
The level of evidence and the strength of recommendation of particular management options were weighed and graded according to predefined scales (Tables 1,2).

Full table

Full table
In recent years, a great number of PG have been issued in Europe by the European Society of Cardiology (ESC), in USA by American College of Cardiology Foundation and the American Heart Association (ACCF/AHA) and in Asia by the Japanese Circulation Society (JCS).
PG relating to aortic disease
European societies
In 2014, ESC’s PG on the diagnosis and treatment of aortic diseases (ESC-AD 2014) are published in European Heart Journal, a thorough document on acute and chronic thoracoabdominal aortic disease (1). Thus updating its previous document published in 2001. Being the most recent and up-to-date guideline.
American societies
In 2010, ACCF/AHA published in Circulation a PG for the diagnosis and management of Thoracic Aortic Disease (ACCF-TAD 2010) (2). In relation to abdominal aortic disease, the recommendations are covered in the 2013 PG on management of patients with Peripheral Artery Disease (ACCF-PAD 2013) (3). And in 2013, the Society of Thoracic Surgeons (STS) given the updates in the open and endovascular surgical field issued a specific PG on aortic valve and ascending aorta that updated previous PG (STS-AA 2013) (4).
Asian societies
In 2013, JCS published in Circulation Journal the PG for diagnosis and treatment of Aortic Aneurysm and Aortic Dissection (JCS-AD 2011), which updated previous PG of 2006. These guidelines indicate the difference between the interpretation of aortic dissection in Japan and that in Western countries and a high frequency of aortic diseases in comparison with other countries in the world, and a high level of accuracy and much better results in medical practice which surpass those in Western countries (5).
In this document we will try to compare the different recommendations issued in all these guidelines, to highlight common points, discrepancies and gaps that still exist in this field.
Imaging modality
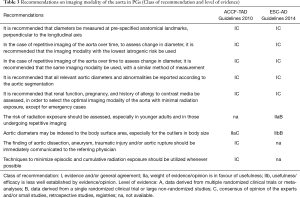
The three PG (ESC-AD, ACCF-TAD and JCS-AD) dedicate a specific chapter to evaluate the different diagnostic tests with very similar conclusions (Table 3).
Full table
Concerning the chest X-ray, it is possible to detect aortic disease, but a normal test does not rule out aortic disease. Therefore, although it is recommended for use in the detection of other aetiologies, it is a technique that does not provide the necessary information for a complete evaluation of these disease (1,2,5).
Ultrasonography is the first test to be performed in screening programmes for aortic disease. Its availability, portability and use for evaluating other heart aspects (ventricular function, valvular disease, pericardial effusion, etc.) make it the first-line technique for acute and chronic disease. All the PG emphasize the superiority of the transesophageal echocardiography (TEE) respect to the transthoracic echocardiography (TTE). However there are limitations in both because they can not visualize all the aortic segments and by the linear artifacts that can be confused with aortic flaps (1,2,5).
Computed tomography (CT) plays a central role in the diagnosis, risk stratification, and management of aortic diseases. Its advantages over other imaging modalities include the short time required for image acquisition and processing, the ability to obtain a complete dataset of the entire aorta, and its widespread availability.
CT is the first-line technique in aortic acute syndromes (AAS) for its speed, availability, sensitivity and specificity. And in SAA always do 1º sin cte to see intramural hematoma (IMH).
Magnetic resonance (MR) is more advantageous than CT in that it requires no X-ray exposure, allows non-contrast imaging and enables the lumen to be evaluated in cases with severely calcified lesions. On the other hand, its disadvantages include lower spatial resolution, inability to visualize osseous structures and difficulty with responding to emergency cases because of the long imaging time. So it is not recommended for diagnosis of acute aortic aneurysm in patients in a poor general medical condition (1,2,5).
The JCS-AD 2011 dedicates a special chapter for Adamkiewicz artery detection presurgery by CT and MR (5).
The ESC-AD 2014 issues information about other techniques such as positron emission tomography in inflammatory or infectious, intravascular ultrasound and assessment of aortic stiffness (1).
Acute aortic syndromes (AAS)
All PG of aorta (ESC-AD, ACCF-TAD and JCS-AD) inscribe an extensive chapter to AAS. It is defined as emergency conditions with a common pathway that eventually leads to a breakdown of the intima and media. In ACCF-TAD and ESC-AD PG, AAS consist of 3 interrelated conditions with similar clinical characteristics and include IMH, penetrating atheroesclerotic ulcer (PAU) and aortic dissection (AD). However, JCS-AD PG decided not to use the term IMH in the clinical setting. Socalled IMH, devoid of tears on diagnostic imaging, is clinically regarded as non-communicating aortic dissection (synonymous with the conventional thrombosed type) and dealt with as a type of dissection (1,2,5).
In regard to AD, three PGs accept the Stanford and the DeBakey anatomic classifications. But temporal classification are different (Table 4).

Full table
The diagnostic work-up of acute aortic syndrome in ACCF-AD and ESC-AD suggest that all patients with suspected AAS, pre-test probability assessment is recommended, according to the patient’s condition, symptoms, and clinical features (IB). TTE is recommended as an initial imaging investigation (IC). In unstabled patients with a suspicion of AAS, TEE or CT are the imaging modalities recommended (IC); in stable patients, CT and MR (IC) but TEE (IIaC). In case of initially negative imaging with persistence of suspicion of AAS, repetitive imaging (CT or MRI) is recommended (IC).
The ESC-AD writes about D-dimer levels in case of low clinical probability of AAS, as ruling out the diagnosis (IIaC).
The JCS-AD does not issue specific recommendations with class of recommendation and level of evidence, but in the text proposes a clinical evaluation focused on pain and physical examination, without mention the patient’s conditions. They agree on the use of TTE as initial examination and CT, TEE or MR if high suspicion of AAS (1,2,5).
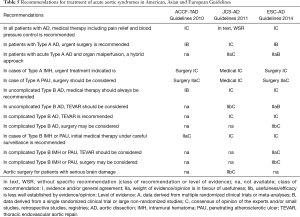
Respecting AAS treatment, PGs broadly coincide with small differences in the level of evidence that supports its recommendations (Table 5).
Full table
The ESC-AD and JCS-AD are more detailed about endovascular or surgical repair in selected cases of type B AD; Which is not present in the ACC guides.
The main discrepant point exists in the IMH type A treatment, the European guidelines recommend surgery (IC), the American also surgery (IIaC) but the Asian advise medical treatment (IIaC) provided that the HIM is <11 mm and the aortic diameter <50 mm. And in the case of HIM type B, all PGs propose medical treatment but ESC proposes as an alternative the TEVAR (IIaC) (Table 5).
The JCS-AD PG dedicated a special section to the recommendations of rehabilitation program for cardiovascular diseases, indicating which patients benefit, type of activity and class of recommendation. There are not information on this matter in the other guidelines (1,2,5).
Aortic aneurysms
Thoracic aortic aneurysms
Screening
Patients with TAA are most often asymptomatic and the diagnosis is made following imaging, performed either for other reasons or for screening purposes. The usefulness of screening patients at risk is well recognized in the case of Marfan syndrome and in patients with a bicuspid aortic valve in all PGs.
Recommendations on medical treatment
The ESC-AD and the JCS-AD express the need for an adequate control of cardiovascular risk factors, emphasizing strict control of blood pressure, both recommend the use of beta-blockers as a first line and the restriction of strenuous physical activity. But it not issue specific recommendations with class of recommendation and level of evidence, nor target LDL cholesterol (1,5).
However, the ACCF-AD give out clear recommendations with class of recommendation and level of evidence (2):
Blood pressure <140/90 and in diabetes or chronic renal disease <130/80. (IB).
To reduce blood pressure with beta blockers and angiotensin-converting enzyme inhibitors or angiotensin receptor blockers. (IIaB).
A statin to achieve a target LDL cholesterol of less than 70 mg/dL. (IIaA).
Smoking cessation. (IB).
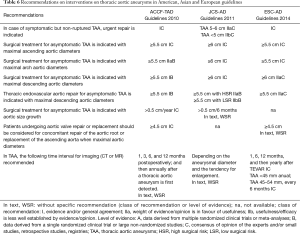
Recommendations on interventions on thoracic aortic aneurysms
The ESC-AD divides its recommendations for root, arch and descending aortic aneurysms, however in the other guides the recommendations are common for the different segments.
American and European guidelines indicate interventionism in cases of operable symptomatic TAA (IC). However, in Japanese guidelines these patients have lower class of recommendation (IIaC if >5 cm and IIbC if <5 cm). In addition, in asymptomatic cases without elastopathy, the American (IC) and European (IIaC) guidelines indicate intervention if TAA diameter exceeds 5.5 cm and Japanese (IC) if exceeds 6 cm (Table 6) (1,2,5).
Full table
Abdominal aortic aneurysms
Screening
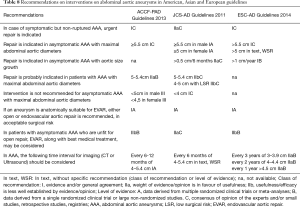
Table 7 shows the recommendation of screening for detection of abdominal aortic aneurysms with physical examination and ultrasound in high risk population.

Full table
Recommendations on medical treatment
The three PGs recognize the adequate control of cardiovascular risk factors, but except in the smoking cessation which both coincide (IB), in other matters there are differences.
The JCS-AD and ESC-AD recommend statins or angiotensin-converting enzyme inhibitors to prevent progression of AAA (IIbB), this information is not present in ACCF-PAD.
On the other hand, the ACCF-PAD recommends beta blockers (IIbB), however the JCS-AD consider Propranolol is not indicated (III) and recommend Doxycycline/Roxithromycin (IIaB). These drugs are not referred to in the ESC-AD (1,3,5).
Recommendations on interventions on thoracic aortic aneurysms
All guidelines recommend repair for aortic abdominal diameters >5.5 cm (IB), the main differences are the indication in Asian PG for women with> 5 cm (IA), indication for aneurysm growth >0.5 cm/6 months in JCS-AD and >1 cm/year in ESC-AD, and the contraindication of intervention in diameters <4 cm in JCS-AD and <5 cm in males and <4.5 cm in females of the ACCF-PAD (Table 8) (1,3,5).
Full table
Genetic diseases affecting the aorta
The three PGs write a specific chapter to the genetic diseases affecting the aorta (syndromics and non-syndromics). And both dedicate a widespread section to Marfan syndrome (especially in JCS-AD).
Marfan syndrome
Diagnosis and follow-up imaging studies
The American guideline recommend an echocardiogram at the time of diagnosis to determine the aortic root and ascending aortic diameters and 6 months thereafter to determine the rate of enlargement of the aorta (level of evidence: IC). And annual imaging if stability of diameters; but if the maximal aortic diameter is ≥4.5 cm or significant growth, more frequent imaging should be considered (IC) (2).
The ESC guideline of grown-up congenital heart disease 2010 (6) expose that stable patients need a yearly visit with echocardiography. MR should be performed at baseline and repeated at least once in 5 years if the aortic size beyond the root is normal. In the case of root aneurysm formation, MR should be repeated at least yearly (without level of evidence).
The JCS guideline recommend regular cardiovascular assessment by imaging (IC) without specific dates or diagnostic test (5).
Prophylactic therapeutics
All the guidelines recommend beta blockers to be able to reduce either the progression of the aortic dilation in patients with AA and Marfan (ACCF-TAD:IB; JCS-AD IC; ESC-AD: In text without specific recommendation). American and European Guidelines propose Losartan (ACCF-TAD: IIaB; ESC-AD: in text, without specific recommendation). But it not present in the Asian guidelines. The JCS guideline suggest exercise limitation (IC), not in the other guidelines (2,5,6).
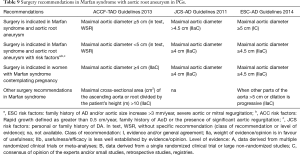
Surgery indications
American and European guidelines recommend surgery when aortic root aneurysm has a maximal aortic diameter ≥5 cm with Marfan syndrome (IC), or ≥4.5 cm with family history of AD and/or aortic size increase >3 mm/year, severe aortic or mitral regurgitation (IIaC); nonetheless the JCS guideline indicate surgery with maximal aortic diameter ≥4.5 cm (IIaC) or >4 cm with family history of AD.
For women with Marfan syndrome contemplating pregnancy, in American and Asian guideline it is reasonable to prophylactically replace the aortic root and ascending aorta if the diameter exceeds 4 cm (IIaC); however in European guideline should be considered in patients who have aortic root aneurysm ≥4.5 cm (IIaC) (Table 9) (2,5,6).
Full table
Atherosclerotic lesions of the aorta
American and European PGs issue that oral anticoagulation or antiplatelet therapy may be considered in stroke patients with aortic arch atheroma (ACCF-TAD: IIbC and ESC-AD: IIaC), and the ACCF-TAD also considers the statin in aortic arch atheroma (IIaC). This section does not appear in JCS guidelines (1,2,5).
Other aortic diseases
The GPs discuss other aortic diseases such as aortitis, tumors, infectious or the aorta in porcelain without addressing issues in detail (1,2,5).
The aortitis is treated in depth by the ACCF-TAD with specific recommendations on Takayasu arteritis. The infective aortic aneurysm is present in all three GPs but only the JCS-AD makes specific recommendations.
The Aortic tumors appear in American and European guidelines without specific recommendations neither levels of evidence.
The porcelain aorta is developed in American and European PGs. And the ESC-AD dedicate a section to the coral reef aorta (very rare calcifying stenotic disease of the juxtarenal and suprarenal aorta).
Special considerations in pregnant patients with aortic disease
ACCF-TAD confer a specific chapter to recommendations for counseling and management of chronic aortic diseases in pregnancy (2).
Women with aortic disease should be counseled about the risk of aortic dissection as well as the heritable nature of the disease prior to pregnancy; strict blood pressure control, monthly or bimonthly echocardiographic until birth; MRI for imaging of pregnant women with aortic dilatation and delivered where cardiothoracic surgery is available (IC).
Fetal delivery via cesarean section is reasonable for patients with significant aortic enlargement, dissection or severe aortic valve regurgitation (IIaC).
If progressive aortic dilatation and/or advancing aortic valve regurgitation are documented, prophylactic surgery may be considered (IIbC).
ESC and JCS PG only talk about pregnancy to reduce the threshold of maxim aortic diameter in Marfan.
Conclusions
The aortic disease comprises a group of different pathologies of high prevalence, seriousness and ever changing by the medical and surgical investigations. Therefore cardiovascular scientific societies in USA, Europe and Asia have created Task Force on PG to develop, update and revise PG for aortic diseases.
American PG (ACCF-TAD 2010) is the oldest of these guides so it has been supplemented with later PGs that deal with AAA (3) or BAV (7). However, it is comprehensive tool whose main recommendations remain valid, and with exclusive sections such as management of pregnant or aortitis.
The Asian PG (JCS-AD 2011) focuses on AD and aortic aneurysms. In general, its recommendations coincide with Western PGs, but with peculiarities such as lower aortic repair thresholds in Marfan but higher thresholds in asymptomatic TAA. And with a special consideration to the HIM separately from AAS and with medical treatment.
The European PG (ESC-AD 2014) is the latest and update document. It detail all aortic disease (thoracic and abdominal), with special sections dedicated to genetic syndromes (Marfan), atherosclerosis, BAV, etc. Nonetheless, there are gaps in matters such as AAA in women, pregnancy or medical therapy in chronic aortic diseases.
In our opinion these PGs are interesting and appropriate documents at present. They issue recommendations based on evidence (mostly consensus opinion of experts, level C) that help the clinician and surgeon in their daily approach to aortic pathology. However, it is important recalled that PGs are general indications and that each case must be adequately individualized to provide our patients the best decisions at any particular moment.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflict of interest to declare.
References
- Erbel R, Aboyans V, Boileau C, et al. 2014 ESC Guidelines on the diagnosis and treatment of aortic diseases. Kardiol Pol 2014;72:1169-252. [Crossref] [PubMed]
- ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with Thoracic Aortic Disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, American Association for Thoracic Surgery, American College of Radiology, American Stroke Association, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of Thoracic Surgeons, and Society for Vascular Medicine. Circulation 2010;121:e266-369. [PubMed]
- Rooke TW, Hirsch AT, Misra S, et al. Management of patients with peripheral artery disease (compilation of 2005 and 2011 ACCF/AHA Guideline Recommendations): a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2013;61:1555-70. [Crossref] [PubMed]
- Svensson LG, Adams DH, Bonow RO, et al. Aortic Valve and Ascending Aorta Guidelines for Management and Quality Measures. Ann Thorac Surg 2013;95:S1-66. [Crossref] [PubMed]
- JCS Joint Working Group. Guidelines for Diagnosis and Treatment of Aortic Aneurysm and Aortic Dissection (JCS 2011) - Digest Version. Circ J 2013;77:789-828. [Crossref] [PubMed]
- Baumgartner H, Bonhoeffer P, De Groot NM, et al. ESC Guidelines for the management of grown-up congenital heart disease (new version 2010). Eur Heart J 2010;31:2915-57. [Crossref] [PubMed]
- Hiratzka LF, Creager MA, Isselbacher EM, et al. Surgery for Aortic Dilatation in Patients With Bicuspid Aortic Valves: A statemet of clarification from the American College of Cardiology/American heart Association task Force on Practice Guidelines. J Am Coll Cardiol 2016;67:724-31. [Crossref] [PubMed]


