Late cardiac tamponade following Nuss procedure for pectus excavatum
Introduction
The Nuss procedure is a recently developed technique for correction of pectus excavatum (1,2). Postoperative complications related to the procedure include pneumothorax, wound seroma, bar displacement, pericarditis, pericardial effusion, and hemothorax. We report on a case of delayed recurrent cardiac tamponade that occurred 16 and 18 months after the patient underwent the Nuss procedure; in this case, we treated the patient with pericardiocentesis the first time and performed pericardial window creation the second time. Regular follow-up in the outpatient department is necessary after surgery.
Case presentation
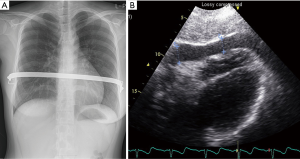
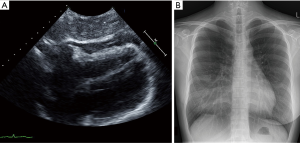
A 23-year-old female patient presented at our emergency department with clinical signs of cardiac tamponade. Sixteen months ago, she underwent the Nuss procedure with a single bar. Her preoperative Haller index was 5. At the 1-month follow-up evaluation the patient presented no specific complains after Nuss operation. The patient presented with aggravation of symptoms such as anorexia, dyspnea on exertion for one month. The patient was not taking any medications, and denied trauma to the chest. The patient appeared to be acutely ill and results of physical examination were as follows: blood pressure, 90/60 mmHg; pulse rate, 125 beats/min; temperature, 38 °C; and respiratory rate, 25/min. A chest radiographic study showed relatively normal cardiac size, but echocardiographic study identified a large amount of pericardial effusion (Figure 1). An electrocardiogram showed low voltage without ST-T wave changes. The laboratory results were as follows: hemoglobin, 14 g/dL; white blood cells, 6,560/mm3; platelets, 220,000/mm3; international normalized ratio of prothrombin time (PT), 1.05; and activated partial thromboplatin time (aPTT), 36.0 seconds. Cardiac enzymes were normal. Urgent echocardiographically guided pericardiocentesis was performed the first time. More than 400 mL of pericardial effusion was drained and central venous catheter was inserted. The pericardial fluid was dark red bloody effusion, with 415,000 red blood cells/mL and 4,000 white blood cells/mL. The drain was removed 4 days later due to significant resolution of the pericardial effusion by follow-up echocardiograms. On day 9, the patient was discharged in an improved condition without bar removal. Two months later, she visited the emergency department for symptoms and clinical signs that were similar to those of the first visit. Emergency echocardiogram showed pericardial effusion with cardiac tamponade physiology (Figure 2A). We performed pericardial window creation and bar removal. The pericardial fluid was 300 mL of dark blood. The pericardial space had localized adhesions in the inferior area. The results of pericardial fluid analysis were similar to those of the first visit. The pericardial biopsy specimen was chronic granulomatous inflammation without evidence of tuberculosis. She was discharged on day 10 in good condition and follow-up chest radiographs showed no fluid collection (Figure 2B). After 1-year follow up, the chest wall deformity was improved.
Discussion
The Nuss procedure for pectus excavatum has become increasingly popular because of its simplicity and good results. A variety of complications can occur, and life-threatening conditions have sometimes been reported (3). Postoperative complications include pneumothorax, wound seroma, bar displacement, pericarditis, pericardial effusion, and hemothorax. The complication rate for pericardial effusion after the Nuss procedure for pectus excavatum is 1.5% (4,5). Cardiac tamponade is rarely observed after this procedure. Transient arrhythmia occurred during Nuss operation. The patient may experience dyspnea on exertion, chest tightness, and, occasionally, pericardial pain. In this case, the etiology of the pericardial effusion and consequent cardiac tamponade appears to be related to postpericardiotomy syndrome. Displacement of the steel bar or trauma to the pericardium when creating the substernal tunnel may cause pericarditis, which induces pericardial effusion. The pathophysiology is hypothesized to be an autoimmune reaction. Damage to the pericardium can cause production of immune complexes, which are deposited on the pericardial surfaces and cause a local inflammatory reaction with exudation. Anti-inflammatory therapy, such as with nonsteroidal anti-inflammatory drugs, is an effective treatment for postpericardiotomy syndrome.
Other possible reasons for production of pericardial effusion are progressive bleeding into the pericardial space due to microperforation of blood vessels and coagulopathy (6). In our case, the pericardial biopsy specimen showed chronic inflammation and pericardial fluid was dark blood, indicating that the steel bar may have injured and irritated the adjacent pericardium.
During the patient’s first consult, cardiac tamponade with hemodynamic compromise was an absolute indication for pericardiocentesis. Under echocardiographic guidance, urgent pericardiocentesis can be performed successfully and safely, and samples of the pericardial fluid can be obtained for diagnostic analyses without performing more invasive procedures. During the second consult, we performed surgical creation of a pericardial window and removed the steel bar. Management during the first admission may not have been optimal. We did not know the exact cause of pericardial effusion. If we thought that Nuss bar caused pericardial effusion, we should have removed Nuss bar at first cardiac tamponade. Combined treatment with oral anti-inflammatory drugs and surgical drainage is effective and safe. The Nuss procedure can lead to life-threatening situations, which may manifest as early or late complications.
Regular follow-up in the outpatient department is necessary after surgery.
Acknowledgements
This work was supported by the 2016 Yeungnam University Research Grant.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Nuss D, Kelly RE, Croitoru DP, et al. A 10-year review of a minimally invasive technique for the correction of pectus excavatum. J Pediatr Surg 1998;33:545-52. [Crossref] [PubMed]
- Park KT, Kim KB, Choi KJ, et al. Early Results of the Nuss Procedure. Korean J Thorac Cardiovasc Surg 2001;34:472-6.
- Hoel TN, Rein KA, Svennevig JL. A life-threatening complication of the Nuss-procedure for pectus excavatum. Ann Thorac Surg 2006;81:370-2. [Crossref] [PubMed]
- Park HJ, Lee SY, Lee CS. Complications associated with the Nuss procedure: analysis of risk factors and suggested measures for prevention of complications. J Pediatr Surg 2004;39:391-5. [Crossref] [PubMed]
- Vegunta RK, Pacheco PE, Wallace LJ, et al. Complications associated with the Nuss procedure: continued evolution of the learning curve. Am J Surg 2008;195:313-6; discussion 316-7. [Crossref] [PubMed]
- Yang MH, Cheng YL, Tsai CS, et al. Delayed cardiac tamponade after the Nuss procedure for pectus excavatum: A case report and simple management. Heart surg forum 2008.E129-31. [Crossref] [PubMed]


