Imaging-guided thoracoscopic resection of a ground-glass opacity lesion in a hybrid operating room equipped with a robotic C-arm CT system
Introduction
Lung cancer screening using CT scans is increasingly being used in apparently healthy individuals, leading to an increased detection of small pulmonary nodules (1,2). Because transthoracic or transbronchial biopsy has inherent limitations (3-5), patients with small lung nodules are frequently referred for surgical consultation when a malignancy is suspected. Video-assisted thoracoscopic surgery (VATS) remains the approach of choice for lung resection. However, the identification of small pulmonary nodules through VATS is still challenging. Although preoperative CT-guided nodule localization is frequently required before entering the operating theater (6), the approach carries substantial risks (7). This issue can theoretically be overcome through a single-stage, CT-guided localization and removal of the pulmonary nodule within a hybrid operating room (OR) environment. Here, we report the case of a patient with stage I lung cancer presenting as an area of ground-glass opacity (GGO) in the right upper pulmonary lobe. He successfully underwent a single-stage, CT-guided localization and removal of the pulmonary nodule within a hybrid OR equipped with a robotic C-arm.
Case presentation
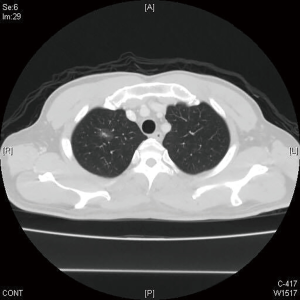
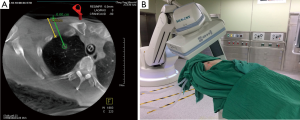
During a routine health examination, a GGO lesion (0.8 cm in size) was identified in the right upper lung field of a 55-year-old man (Figure 1). A follow-up CT scan performed after 3 months revealed a slightly enlarged lesion with an increased local tracer uptake on PET imaging. Lung cancer was suspected, and the patient was offered surgery in a hybrid OR equipped with a robotic C-arm CT (Artis zeego, Siemens Healthcare GmbH, Erlangen, Germany). The patient underwent a double-lumen endotracheal intubation and was subsequently placed into a lateral decubitus position. After successful docking of the C-arm, an initial CT scan with a 6-sec protocol (syngo DynaCT) was acquired for intervention planning. The access path was laid out in the isotropic data set using the syngo Needle Guidance of a syngo X-Workplace (Siemens Healthcare GmbH). The needle path was initially calculated (Figure 2A) and then projected with a laser beam (Figure 2B). While maintaining the lung inflated, ventilation was arrested and a hook wire was positioned under laser-supported guidance. Upon completion of the procedure, a second DynaCT scan with a 5-sec protocol was acquired to confirm the proper placement of the hook wire. A VATS wedge resection was subsequently performed under wire guidance. A frozen section test confirmed the presence of a lung adenocarcinoma, and the patient underwent segmentectomy accompanied by mediastinal lymph node dissection. He had an uneventful postoperative course and was discharged on the third postoperative day. The final pathologic stage was pT1aN0.
Discussion
Owing to the loss of tactile sensing, the identification of small lung nodules during VATS is still challenging especially in presence of minute, nonpalpable GGO lesions. Consequently, large lung parenchyma resections and/or conversion to thoracotomy may be necessary to ensure complete tumor removal (8). Before entering the OR, numerous localization methods (e.g., CT-guided placement of hook wires, use of methyl blue dye, and microcoil localization) have been proposed (9-12) to facilitate the subsequent VATS removal. However, current approaches have considerable limitations. Although the time elapsed between tumor localization and subsequent surgery should be kept as short as possible, an optimal synchronization is not always possible. Importantly, the complication rates (including hemothorax, pneumothorax, hemoptysis, and wire dislodgement) of CT-guided biopsy or CT-guided localization of pulmonary nodules vary between 9.7% and 32% (7,13,14). The inability to detect and manage complications in a timely manner may jeopardize the patient’s safety. In this context, localization and surgery performed in a single stage within a hybrid OR may be a helpful risk-minimizing strategy.
Differently from previous reports focusing on the use of conventional MDCT in hybrid OR, the localization procedure used for our patient was performed through a robotic C-arm CT. The advantages of the latter approach over conventional MDCT include (I) the lack of restriction to a single plane allowing localization to be performed in the lateral decubitus position; and (II) a careful path planning of the needle from the skin toward the target lesion. Unfortunately, the single-stage approach is not without limitations. First, hybrid ORs are not yet widely available because of their high costs. Second, the anesthesia equipment may necessitate a time-consuming and cumbersome repositioning aimed at minimizing the risk of collision with the C-arm. Third, the risk of life-threatening air embolism caused by needle positioning is not negligible and may even increase when general anesthesia is used (15). The incidence rate of systemic air embolism as reported in previous large case series is 0.02–0.06%, with endotracheal anesthesia being an independent risk factor (15-17). Definitive conclusions on the utility of this approach will no doubt be expanded by prospective trials comparing different intraoperative lung localization techniques.
Conclusions
Hook wire localization and surgery in a single stage within a hybrid OR equipped with C-arm CT may be a helpful risk-minimizing strategy in patients with small pulmonary nodules.
Acknowledgements
Funding: This work was supported by grants CMRPG3F1811 from Chang Gung Memorial Hospital, Taiwan.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Henschke CI. Early lung cancer action project: overall design and findings from baseline screening. Cancer 2000;89:2474-82. [Crossref] [PubMed]
- Callol L, Roig F, Cuevas A, et al. Low-dose CT: a useful and accessible tool for the early diagnosis of lung cancer in selected populations. Lung Cancer 2007;56:217-21. [Crossref] [PubMed]
- Mazzone P, Jain P, Arroliga AC, et al. Bronchoscopy and needle biopsy techniques for diagnosis and staging of lung cancer. Clin Chest Med 2002;23:137-58. ix. [Crossref] [PubMed]
- Griffin JP, Zaman MK, Niell HB, et al. Diagnosis of lung cancer: a bronchoscopist's perspective. J Bronchology Interv Pulmonol 2012;19:12-8. [Crossref] [PubMed]
- Tochigi N, Dacic S, Ohori NP. Bronchoscopic and transthoracic cytology and biopsy for pulmonary nonsmall cell carcinomas: performance characteristics by procedure and tumor type. Diagn Cytopathol 2012;40:659-63. [Crossref] [PubMed]
- Hsu HH, Shen CH, Tsai WC, et al. Localization of nonpalpable pulmonary nodules using CT-guided needle puncture. World J Surg Oncol 2015;13:248. [Crossref] [PubMed]
- Ichinose J, Kohno T, Fujimori S, et al. Efficacy and complications of computed tomography-guided hook wire localization. Ann Thorac Surg 2013;96:1203-8. [Crossref] [PubMed]
- Suzuki K, Nagai K, Yoshida J, et al. Video-assisted thoracoscopic surgery for small indeterminate pulmonary nodules: indications for preoperative marking. Chest 1999;115:563-8. [Crossref] [PubMed]
- McConnell PI, Feola GP, Meyers RL. Methylene blue-stained autologous blood for needle localization and thoracoscopic resection of deep pulmonary nodules. J Pediatr Surg 2002;37:1729-31. [Crossref] [PubMed]
- Powell TI, Jangra D, Clifton JC, et al. Peripheral lung nodules: fluoroscopically guided video-assisted thoracoscopic resection after computed tomography-guided localization using platinum microcoils. Ann Surg 2004;240:481-8; discussion 488-9. [Crossref] [PubMed]
- Miyoshi K, Toyooka S, Gobara H, et al. Clinical outcomes of short hook wire and suture marking system in thoracoscopic resection for pulmonary nodules. Eur J Cardiothorac Surg 2009;36:378-82. [Crossref] [PubMed]
- Mayo JR, Clifton JC, Powell TI, et al. Lung nodules: CT-guided placement of microcoils to direct video-assisted thoracoscopic surgical resection. Radiology 2009;250:576-85. [Crossref] [PubMed]
- Dendo S, Kanazawa S, Ando A, et al. Preoperative localization of small pulmonary lesions with a short hook wire and suture system: experience with 168 procedures. Radiology 2002;225:511-8. [Crossref] [PubMed]
- Poulou LS, Tsagouli P, Ziakas PD, et al. Computed tomography-guided needle aspiration and biopsy of pulmonary lesions: a single-center experience in 1000 patients. Acta Radiol 2013;54:640-5. [Crossref] [PubMed]
- Freund MC, Petersen J, Goder KC, et al. Systemic air embolism during percutaneous core needle biopsy of the lung: frequency and risk factors. BMC Pulm Med 2012;12:2. [Crossref] [PubMed]
- Richardson CM, Pointon KS, Manhire AR, et al. Percutaneous lung biopsies: a survey of UK practice based on 5444 biopsies. Br J Radiol 2002;75:731-5. [Crossref] [PubMed]
- Tomiyama N, Yasuhara Y, Nakajima Y, et al. CT-guided needle biopsy of lung lesions: a survey of severe complication based on 9783 biopsies in Japan. Eur J Radiol 2006;59:60-4. [Crossref] [PubMed]