Rupture of right sinus of Valsalva aneurysm protruding into the pulmonary artery with aortic and pulmonary valve endocarditis
Introduction
A sinus of Valsalva aneurysm (SVA) is a relatively rare cardiac disease, which may be congenital or acquired (1).The congenital form is frequently associated with a ventricular septal defect (VSD), aortic valve dysfunction, and/or other cardiac abnormalities.
It can become complicated with rupture or infection (2-5). Although all three aortic sinuses can rupture, the right aortic sinus does so most commonly, and the receiving chamber is right-sided, resulting in a left-to-right shunt. The most common receiving chamber is the right ventricle; a ruptured right aortic sinus aneurysm draining into the pulmonary artery is extremely rare (6). We present a case of SVA rupture into the pulmonary artery with aortic and pulmonary valve endocarditis.
Case presentation
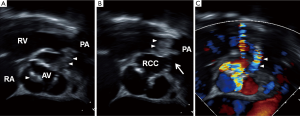
A 42-year-old man was admitted to the emergency room with severe dyspnea and fever of 1-day duration. When he was 13 years old, he received a diagnosis of VSD. The patient had been diagnosed with SVA and grade III aortic valve regurgitation 1 year previously. On admission, he appeared acutely ill; his vital signs included a blood pressure of 90/50 mmHg, a heart rate of 87 beats/min, a respiratory rate of 18 breaths/min, and a body temperature of 38 °C. The heart rate was regular, and systolic and diastolic murmurs were heard over the right sternal border. Laboratory examination revealed that white blood cell count was 31,530/uL and C-reactive protein level was 10.65 mg/dL, but the erythrocyte sedimentation rate was normal. Echocardiography revealed multiple vegetations attached the aortic valve (Figure 1A) and the pulmonary valve (Figure 1B) with left-to-right shunting from the aneurysmal right aortic sinus to the pulmonary artery (Figure 1C). The aortic root diameter was 45 mm. The degree of aortic regurgitation was grade 4 and tricuspid regurgitation was grade 2. A small VSD had formed from the right coronary cusp side of the left ventricular outflow tract to just inferior of the pulmonary valve. A blood culture at the time of emergency room admission grew Streptococcus anginosus. The patient showed severe malnutrition; his serum albumin was 2.3 g/dL. He was relatively stable with supportive medications, and thus, operation was delayed for a week, during which nutritional support and antibiotics were provided. Antibiotics were changed from a 3rd generation cephalosporin to amoxicillin/clavulanic acid and an aminoglycoside, in accordance with susceptibility test results. Elective surgery was performed using the dual exposure technique, and the aorta and pulmonary trunk were opened. The right aortic sinus was ruptured with fenestration and vegetation. Pulmonary valve leaflets were severely damaged with densely attached vegetation (Figure 2A).
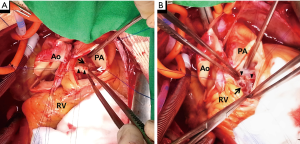
The wall of the right aortic SVA was exposed from the RV after pulmonary arteriotomy. After removal of all aneurysmal sacs, we found that the base of the aneurysmal sac was just beneath the pulmonary valve (Figure 2B). The defect caused by the aneurysmal sac opening and the VSD were too close to repair separately. We directly closed the base of the sac and widely covered the right aortic sinus wall and the VSD with a Gore-Tex (polytetrafluoroethylene; Gore Medical, Arizona, USA) patch as in the right ventricular side. Through the aortotomy with an approach from the left ventricle, the VSD was closed with another Gore-Tex patch. We decided to implant mechanical valves due to the patient age and he didn’t want repeat operation. The severely damaged aortic and pulmonary valves were resected and replaced with mechanical valves (aortic valve, 22 mm; pulmonary valve, 26 mm, Medtronic ATS Medical, Minneapolis, MN). Tricuspid valve annuloplasty was performed using DeVega’s method. Aortic cross clamp time was 175 minutes. No complication was encountered during hospitalization, and antibiotics were administered for 5 weeks. Follow-up echocardiography demonstrated no residual shunt and satisfactory functioning of both replaced valves. After discharge, the patient was followed for 2 years, during which he showed no problems or recurrence of endocarditis.
Discussion
Patients with infective endocarditis have been reported to present with ruptured SVA. Sources have described bacterial endocarditis leading to rupture of sinus of Valsalva (5) and sinus of Valsalva rupture caused by infective endocarditis (3,4).
The described case is unusual; regarding the findings that the patient had simultaneous pulmonary and aortic valve endocarditis with a ruptured right SVA. Generally, SVA and VSD are considered leading factors for the occurrence of endocarditis (2). Our patient had been diagnosed as having a VSD when he was a child; therefore, we presume that the aneurysm and the VSD had predisposed the patient to infective endocarditis, subsequently involving the aortic and pulmonary valves through the ruptured aneurysm.
The timing of operation is important for eradication of the vegetation and for restoration of hemodynamic stability due to the left-to-right shunt or valvular dysfunction. If the patient has an unstable hemodynamic status or overwhelming sepsis, immediate surgical treatment is needed. Our patient was relatively stable with supportive medications, but showed severe malnutrition. Thus, operation was delayed for a week, for which nutritional support and administration of antibiotics were performed.
In ruptured cases, the common surgical technique is “dual exposure/repair technique”, in which both the chamber of rupture and the aorta are opened (7). The aneurysmal sac is excised and repaired using patch closure or direct suturing, depending on the location and the size of the defect. If coexisting lesions are present, such as a VSD, they are repaired using the same methods. Recently, the prognosis after surgical repair has been reported to be excellent, with a 10-year survival rate of 90% (8).
Rupture of the right aortic SVA draining to the pulmonary artery is a very rare case (6) and to our knowledge, this is the first such case with associated aortic and pulmonary valve endocarditis resulting in valve replacement. Here, we report an unusual case of SVA rupture draining to the pulmonary artery with aortic and pulmonary valve endocarditis. The patient had a satisfactory outcome after double valve replacement using the dual chamber approach.
Acknowledgements
This work was supported by the 2014 Yeungnam University Research Grant.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Ott DA. Aneurysm of the sinus of valsalva. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu 2006.165-76. [Crossref] [PubMed]
- Patra KP, Vanchiere JA, Bocchini JA Jr, et al. Endocarditis with ruptured sinus of Valsalva aneurysm caused by nonvaccine Streptococcus pneumoniae serotype 21. Tex Heart Inst J 2012;39:277-80. [PubMed]
- Vereckei A, Vándor L, Halász J, et al. Infective endocarditis resulting in rupture of sinus of Valsalva with a rupture site communicating with both the right atrium and right ventricle. J Am Soc Echocardiogr 2004;17:995-7. [Crossref] [PubMed]
- Encarnacion CO, Loranger AM, Bharatkumar AG, et al. Bacterial Endocarditis Caused by Lactobacillus acidophilus Leading to Rupture of Sinus of Valsalva Aneurysm. Tex Heart Inst J 2016;43:161-4. [Crossref] [PubMed]
- Ikeda A, Nakajima T, Konishi T, et al. Infective endocarditis of an aorto-right atrial fistula caused by asymptomatic rupture of a sinus of Valsalva aneurysm: a case report. Surg Case Rep 2016;2:43. [Crossref] [PubMed]
- Afshar AH, Kolesnikov S, Pourafkari L, et al. Right Valsalva Sinus Aneurysm Protruding Into the Right Ventricle: A Case Report. J Cardiovasc Thorac Res 2015;7:126-8. [Crossref] [PubMed]
- Vural KM, Sener E, Taşdemir O, et al. Approach to sinus of Valsalva aneurysms: a review of 53 cases. Eur J Cardiothorac Surg 2001;20:71-6. [Crossref] [PubMed]
- Yan F, Abudureheman M, Huo Q, et al. Surgery for sinus of Valsalva aneurysm: 33-year of a single center experience. Chin Med J (Engl) 2014;127:4066-70. [PubMed]


