Prognostic factors after pulmonary metastasectomy of colorectal cancers: a single-center experience
Introduction
Colorectal cancer (CRC) is one of the most frequent malignant tumors in western countries (1). Despite improvements in diagnosis and evolutions in the multidisciplinary management, it remains a major cause of cancer-related deaths (2). Lungs are a common site of seeding of colorectal cancers with pulmonary metastasis occurring in about 10% of patients treated by surgical resection of the primary tumor (3). Surgical resection has been widely accepted as the treatment of choice for pulmonary metastases in highly selected patients, showing prolonged survivals after metastasectomy (4). Nevertheless, this practice is not supported by high level evidence for effectiveness, and is mainly based on study of registries or retrospective series, often on heterogeneous and relatively small samples. Thus, there is no standard indication, and suitability for surgery remains controversial. The purpose of this study was to evaluate long-term outcomes and to assess factors influencing survival in consecutive patients who underwent resection of lung metastases from colorectal cancer by a single surgical team, in a relatively short time frame, in the setting of an updated multimodal approach.
Methods
We retrospectively reviewed medical records of all patients who underwent resection of proven lung metastases of colic or rectal primary tumor, in our department, from January 2004 to December 2013. Eligibility criteria for resection of pulmonary metastases of colorectal cancer included single or multiple, one-sided or bilateral, and synchronous or metachronous lesions. Patients with evidence of hepatic metastases and suspicion of nodal involvement were also included. Presence of either extra-thoracic or extra-hepatic lesions, unfeasibility of complete resection (R0) and inadequate predicted postoperative pulmonary function were criteria to consider patients non-suitable for curative surgery. Systemic chemotherapy modalities were decided for each patient by a multidisciplinary board and were categorized for the purpose of this study into three groups: no chemotherapy; FOLFOX (5-fluorouracil/folinic acid + oxaliplatin) and/or FOLFIRI (5-fluorouracil/folinic acid +irinotecan); other regimens.
The surgical procedure was always performed with the aim of achieving complete resection. In case of solitary and peripheral metastasis a video-thoracoscopic approach could be preferred to a postero-lateral thoracotomy which was the standard approach for palpation and resection of multiple lesions and to perform laser or anatomic resections. Mediastinal and hilar lymphadenectomy was usually performed. Non-anatomic resections consisted in wedge, laser or electrosurgical metastasectomy while anatomic resections were segmentectomies, lobectomies or pneumonectomies. Anatomic resections, whose extent was dictated by topography of lesions, were carried out only if non-anatomical resection was not satisfactory in dealing radically with the disease. Anatomic and non-anatomic resections could be associated depending on operative findings and were left to surgeon’s discretion.
Every effort was carried out to obtain follow-up information, through direct telephonic interviews of patients or relatives, family or specialist physicians, as well as by consultation of city registers. Pulmonary recurrence was defined as a pulmonary lesion which didn’t exist at preoperative work-up preceding the first thoracic intervention. Only patients with available survival information were considered suitable for analysis.
Statistical analysis
Survival time was computed from the time of the first lung metastasis surgery to the time of the death [overall survival (OS)] or to the time of the first recurrence or death [recurrence free survival (RFS)]. The end of follow-up was set at December 31st 2014. Data analysis was completed on November 10th 2016. Descriptive statistics were expressed as means ± standard deviations for quantitative variables and as frequencies (percentages) for qualitative variables. Both OS and RFS were evaluated by the Kaplan-Meier method.
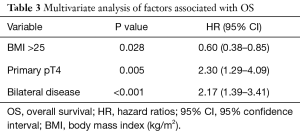
The associations between patient, preoperative and perioperative characteristics and OS were studied using the log-rank test. All variables with a P value <0.05 at univariate analysis were included in a stepwise Cox regression model. Results of multivariate analyses were expressed using hazard ratios (HR) and their 95% confidence interval (95% CI). P value <0.05 was considered to indicate statistical significance.
The study was carried out according to principles outlined in the Helsinki declaration and in agreement with French laws on biomedical research: in particular given the retrospective character of this non-interventional study, submission to the Ethical committee was waived. Patients of relatives (in case of deceased patients) gave their informed consent.
Results
Within the study period, 306 patients underwent surgical resection of pulmonary colorectal metastases in our thoracic center. There were 204 (66.7%) men and 102 (33.3%) women. Mean age was 64.0±11.6 years at time of first pulmonary metastasectomy. Mean body mass index (BMI) and forced expiratory volume in 1 second (FEV1) were 25.1±3.9 kg/m2 and 93.5±18.1% of predicted value, respectively. Other patient characteristics are summarized in Table 1.
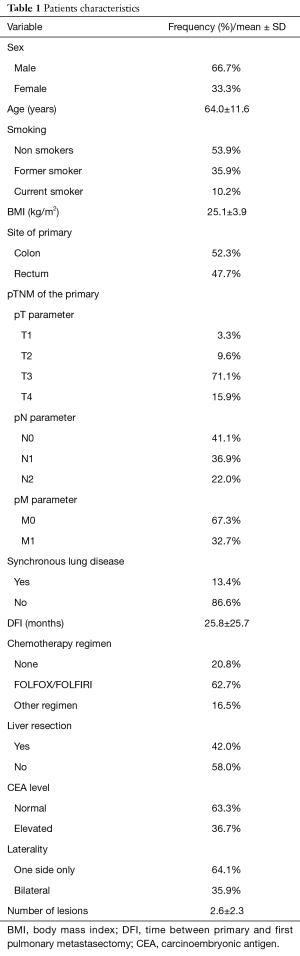
Full table
With respect to pre-thoracotomy chemotherapy, 20.8% did not receive any systemic treatment while most patients (62.7%) were treated with FOLFOX or FOLFIRI protocols, whereas other regimens accounted for the remaining 16.5% of cases.
At preoperative imaging work-up, mean number of lesions at CT scan and nodules with significant FDG-uptake (SUV max >3) at 18F-FDG PET were 2.6±2.3 and 1.39±1.17, respectively.
With respect to surgical procedure, one-sided or bilateral video-thoracoscopic approach was performed in 38 (12.4%) and 8 (2.6%) patients, respectively, whereas the remaining patients had postero-lateral thoracotomy. Ninety-one (29.7%) patients underwent bilateral sequential surgery for an initially unilateral disease, whereas bilateral pulmonary disease was detected in 110 (35.9%) patients at baseline diagnostic work-up. Including first and second side surgery, at least one anatomic resection was performed in 132 (43.1%) patients. Ratios of each largest resection type at first side surgery were: segmentectomy 20.6%, lobectomy 12.9%, bilobectomy 1.2%, pneumonectomy 1.2%, and non-anatomical resection 64.1%.
No in-hospital death occurred. Mean length of hospital stay was 8.2±3.4 days with uneventful early postoperative course occurring in 84.6% of cases.
At pathology, mean number of resected metastasis was 2.6±2.3, ranging 1–12. Resection was complete in 92.5% of patients. Nodal involvement, assessed by analysis of samples from first and second side (when performed), was proven in 40 (12.9%) patients. The initially planned complete resection could not be achieved in 23 (7.5%) cases: 4 patients had R1 resection because of positive resection margins at pathologic analysis, and 2 had macroscopically gross residual disease (R2); 17 further patients did not undergo the initially planned staged surgery, because complete resection was no longer considered feasible at second side preoperative work-up. For analysis purposes, these last patients were pooled with R2 patients.
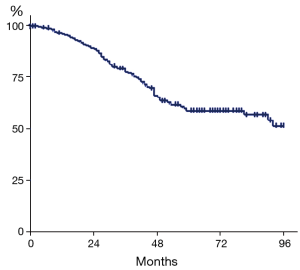
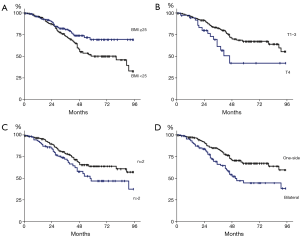
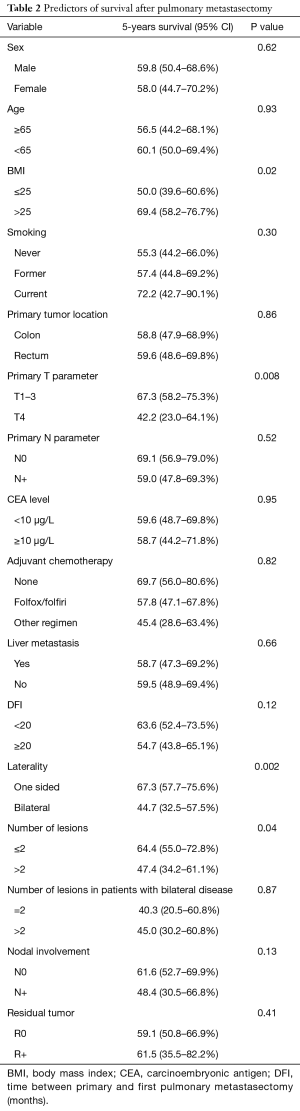
Mean follow-up was 3.06±2.36 years. OS estimates were 77.8% (95% CI, 72.7–82.7%), 59.0% (95% CI, 51.2–66.4%), and 56.9% (95% CI, 48.4–65.0%) at 3, 5 and 7 years, respectively (Figure 1). At univariate analysis, bilateral lung metastases (P=0.002), pT4 primary tumor (P=0.008), BMI ≤25 (P=0.02) and number of lesions at CT scan evaluation (P=0.04) were significantly associated with shorter survival (Figure 2). Synchronous disease, presence of liver metastases, abnormal preoperative CEA level, age, nodal involvement, and R+ resection were not significantly associated with OS (Table 2). At multivariate analysis, including pT parameter of the primary tumor, number of lesions, one-sided versus bilateral lung disease, and BMI, only bilateral disease (P<0.001) and pT4 primary (P=0.005) were independent pejorative prognostic factors whereas BMI ≥25 was protective (P=0.028) (Table 3).
Full table
Full table
After the first sequence of lung metastasectomy (unilateral or bilateral, depending on initial presentation), and excluding incomplete resections, 55.7% of patients experienced at least one recurrence. Location of recurrence was pulmonary or extra-pulmonary in 72.4% and 27.6% of cases, respectively. In patients who experienced a pulmonary recurrence, 43.9% underwent re-do surgical metastasectomy while the others were treated with chemotherapy (50.8%), local non-surgical treatment (3%) or close follow-up only (2.3%). There was no perioperative death after repeated metastasectomy.
Kaplan-Meier analysis revealed that recurrence-free survival (RFS) was 76.3% (95% CI, 71–80.7%), 38.9% (95% CI, 33–44.7%), 28.3% (95% CI, 22.5–34.4%) and 22.7% (95% CI, 16.5–29.5%) at 1, 3, 5 and 7 years, respectively.
Discussion
In this large single-center study, we showed that, in selected patients with CRC, pulmonary metastasectomy allows satisfactory oncological results with an overall 5-year survival of almost 60% and no perioperative death, even in patients with repeated lung surgery. Multivariate analysis revealed that bilateral lung metastases, BMI <25, and pT4 primary tumor were strong and independent factors of poor survival, differently from the number of lesions. Although the number of lesions (≤2 vs. >2) was associated with worse survival at univariate analysis (P=0.04), it lost significance at multivariate analysis. This is confirmed by subgroup analysis of patients with bilateral disease at diagnosis, in whom the number of lesions was not associated with survival, even at univariate analysis (P=0.87). The number of pulmonary lesions has been often cited as a reliable prognostic factor and thus used as selection criterion (5,6). In our series, more than a cut-off for number of metastasis to indicate surgery, we employed feasibility of complete resection (R0) at preoperative work-up as fundamental criterion for patients’ eligibility. Our results support this choice, demonstrating that number of lesions is not an independent prognostic factor unlike bilateralism which is probably a superior indicator for eligibility. The influence of bilateralism on survival may be due to the disease progression during the interval between interventions, but is more likely to reflect the whole aggressiveness of the metastatic disease. Indeed, we consider that the potential pejorative prognostic factor of bilateralism shouldn’t preclude, to date, patients from benefiting surgical treatment, which is associated with high survival, as shown in a well-conducted meta-analysis (7). In this kind of surgery, interpretation of survival and prognostic factors must be very careful and it is important to recognize that results of metastasis surgery are submitted to many selection biases. Indeed, patients are referred to surgical departments after being previously selected on inherent favorable clinical criteria and response to variable systemic treatments (8,9).
The effect of patient selection on survival is sometimes responsible for counterintuitive results such as the reported higher 5-year survival in patients undergoing both liver and lung resection versus liver metastasectomy only (10). Our results do not corroborate this latest observation, but revealed another paradoxical effect of patient selection: among patients with bilateral disease, there was no difference in prognosis according to R0 or R+ resection. Indeed, such outcome is very confusing because it is contrary to the admitted rational principle of curative cancer surgery or to results of other institutional studies, and probably reflects the difficulties in choosing a surgical or non-surgical treatment and in assessing respective results in patients who have general eligibility criteria for lung surgery (fitness, no other site of metastatic spread, otherwise satisfactory control of disease) in spite of bilateral disease (11). In this light, among criteria for eligibility, patient-related factors, more than merely tumor-related factors should be also taken into account to allow a decision of surgery based on a global clinical-pathological evaluation: for instance we found that higher body-mass index was independently associated with good long-term outcome as already demonstrated in primary lung cancer resection (12).
Among other preoperative factors associated with prognosis, CEA level is very often reported and thus used as a selection criterion for surgery (13,14). Despite the probable value of CEA level in predicting CRC extension, our series did not demonstrate any significant association between preoperative CEA level and survival. Maybe, heterogeneity in methods of assessment in the 10-year frame period of the study was responsible for this lack of prognostic significance.
Another prognostic factor which has to be discussed is the intra-thoracic nodal involvement: in our series significance could not be reached, and prognostic value is controversial in literature (15,16), suggesting the necessity of specifically designed prospective studies to assess the need of systematic hilar and mediastinal lymph node dissection in CRC metastasis surgery.
More than half patients from our cohort experienced recurrences of the metastatic disease with frequent pulmonary relapses which could be safely treated by iterative surgery. Even if we were not able to show any significant influence of re-do resection on OS, it seems legitimate to perform iterative metastasectomy in order to allow the disease become “chronic”. Welter et al. focused on repeated lung resection in CRC and reported a satisfying 53.8% 5-year survival (17). However, these encouraging results must be interpreted carefully in the light of possible even stronger selection bias.
Besides the possible selection bias, our study has some other limitations, mainly derived from its retrospective and monocentric character. In addition, follow-up methods were variable, depending on each referring center policies. Thus, some prognostic data, like recurrence free interval, may be subjected to criticism.
In conclusion, many factors like bilateralism and primary tumor local extension influence the prognosis of patients surgically treated for pulmonary CRC metastases and must be taken into account for eligibility. Yet, the presence of numerous selection biases highlights the need for prospective or randomized trials in order to determine the true value and reliability of pulmonary metastasectomy from CRC in terms of survival and quality of life (18).
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was carried out according to principles outlined in the Helsinki declaration and in agreement with French laws on biomedical research: in particular given the retrospective character of this non-interventional study, submission to the Ethical committee was waived. Patients of relatives (in case of deceased patients) gave their informed consent.
References
- Jemal A, Bray F, Center MM, et al. Global cancer statistics. CA Cancer J Clin 2011;61:69-90. [Crossref] [PubMed]
- American Cancer Society. Cancer Facts & Figures 2009. Accessed October1, 2009. Available online: https://www.cancer.org/research/cancer-facts-statistics/all-cancer-facts-figures/cancer-facts-figures-2009.html
- McCormack PM, Burt ME, Bains MS, et al. Lung resection for colorectal metastases. 10-year results. Arch Surg 1992;127:1403-6. [Crossref] [PubMed]
- Pfannschmidt J, Dienemann H, Hoffmann H. Surgical resection of pulmonary metastases from colorectal cancer: a systematic review of published series. Ann Thorac Surg. 2007;84:324-38. [Crossref] [PubMed]
- Onaitis MW, Petersen RP, Haney JC, et al. Prognostic factors for recurrence after pulmonary resection of colorectal cancer metastases. Ann Thorac Surg 2009;87:1684-8. [Crossref] [PubMed]
- Girard P, Spaggiari L, Baldeyrou P, et al. Should the number of pulmonary metastases influence the surgical decision? Eur J Cardiothorac Surg 1997;12:385-91. [Crossref] [PubMed]
- Pfannschmidt J, Hoffmann H, Dienemann H. Reported outcome factors for pulmonary resection in metastatic colorectal cancer. J Thorac Oncol 2010;5:S172-8. [Crossref] [PubMed]
- Fiorentino F, Treasure T. Pulmonary metastasectomy: are observational studies sufficient evidence for effectiveness? Ann Thorac Surg 2013;96:1129-31. [Crossref] [PubMed]
- Åberg T, Malmberg KÅ, Nilsson B, et al. The effect of metastasectomy: fact or fiction? Ann Thorac Surg 1980;30:378-84. [Crossref] [PubMed]
- Brouquet A, Vauthey JN, Contreras CM, et al. Improved survival after resection of liver and lung colorectal metastases compared with liver-only metastases: a study of 112 patients with limited lung metastatic disease. J Am Coll Surg 2011;213:62-9. [Crossref] [PubMed]
- Zampino MG, Maisonneuve P, Ravenda PS, et al. Lung metastases from colorectal cancer: analysis of prognostic factors in a single institution study. Ann Thorac Surg 2014;98:1238-45. [Crossref] [PubMed]
- Hervochon R, Bobbio A, Guinet C, et al. Body Mass Index and Total Psoas Area Affect Outcomes in Patients Undergoing Pneumonectomy for Cancer. Ann Thorac Surg 2017;103:287-95. [Crossref] [PubMed]
- Carcinoembryonic antigen: its role as a marker in the management of cancer. Summary of an NIH consensus statement. Br Med J (Clin Res Ed) 1981;282:373-5. [Crossref] [PubMed]
- Stangl R, Altendorf-Hofmann A, Charnley RM, et al. Factors influencing the natural history of colorectal liver metastases. Lancet 1994;343:1405-10. [Crossref] [PubMed]
- Hamaji M, Cassivi SD, Shen KR, et al. Is lymph node dissection required in pulmonary metastasectomy for colorectal adenocarcinoma? Ann Thorac Surg 2012;94:1796-800. [Crossref] [PubMed]
- Veronesi G, Petrella F, Leo F, et al. Prognostic role of lymph node involvement in lung metastasectomy. J Thorac Cardiovasc Surg 2007;133:967-72. [Crossref] [PubMed]
- Welter S, Jacobs J, Krbek T, et al. Long-term survival after repeated resection of pulmonary metastases from colorectal cancer. Ann Thorac Surg 2007;84:203-10. [Crossref] [PubMed]
- Fiorentino F, Treasure T. Pulmonary metastasectomy for colorectal cancer: making the case for a randomized controlled trial in the zone of uncertainty. J Thorac Cardiovasc Surg. 2013;146:748-52. [Crossref] [PubMed]


