Multicentric study of endobronchial ultrasound-transbronchial needle aspiration for lung cancer staging in Italy
Introduction
Treatment and prognosis of non-small cell lung cancer (NCSLC), the leading cause of cancer death worldwide, requires accurate staging. The 2014 guidelines of the European Society of Thoracic Surgeons indicate endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) as the initial approach for pathological evaluation of mediastinal lymph nodes (1,2). In the last 15 years EBUS-TBNA has increasingly been used for minimally invasive diagnosis of mediastinal-hilar lymph node metastases in patients with NSCLC, and in selected cases this technique has replaced mediastinoscopy, video-thoracoscopy and traditional transbronchial biopsy (2).
The aim of this study is to evaluate the EBUS-TBNA diagnostic performance for staging hilar-mediastinal lymph nodes in an Italian multi-institutional cohort of lung cancer patients, and to analyze some of the factors influencing the diagnostic yield.
Methods
A retrospective, multicenter study of patients with NSCLC undergoing EBUS-TBNA between January 2011 and July 2016 was conducted in the interventional bronchoscopy units of five thoracic surgery centers in northern Italy (Milan, Policlinico Universitario; Bergamo, Clinica Humanitas; Brescia, Spedali Civili; Varese, Università Insubria Ospedale di Circolo; Verona, Ospedale Universitario Borgo Trento). In each participating center the patient inclusion criteria for study were: both genders;
Procedure
The EBUS-TBNA procedures were performed with a linear echo-endoscope by expert interventional pulmonologists or thoracic surgeons according to the usual practice in each center, without pre-defined standards. Conscious sedation with intravenous midazolam and fentanyl was used in all participating institutes. The Doppler function was used in selected patients. Target lymph nodes were identified under direct ultrasound guidance and were sampled using either 21- or 22-Gauge (G) needle, according to the usual practice in each center. Each lymph node was biopsied with at least three needle passes, each pass including 5 to 15 agitations within the targeted node. Specimens were allocated into liquid fixative suitable for cell-block preparations (all centers), or into formalin for core biopsy histology (Varese, Verona and Brescia centers only). Among the five participating centers, specimen rapid on-site evaluation (ROSE) was performed only in selected patients of Brescia and Verona centers. The choice of specimen preparation method was left to the local pathologist’s preference and experience; in some cases a combination of two preparations (cytology slides and cell-block) was used for evaluating the specimen.
Statistical analysis
The EBUS-TBNA performance in diagnosing malignancy was calculated in the pooled series of the five centers, according to standard definitions [sensitivity: true positive/(true positive + false negative); negative predictive value (NPV): true negative/(true negative + false negative); diagnostic accuracy: (true positive + true negative)/(true positive + false positive + true negative + false negative)]. Chi-square test was used to examine the association of two or more categorical variables. Univariate and multivariate analysis were performed to identify among the following factors those influencing the EBUS-TBNA diagnostic yield: needle gauge, specimen processing technique, center. P value <0.05 was considered statistically significant. The statistical analyses were done using MedCalc statistical software version 17.1 (MedCalc Software bvba, Ostend, Belgium; http://www.medcalc.org; 2014).
Results
Altogether in the five participating centers 485 patients undergoing EBUS-TBNA and fulfilling the inclusion criteria of study were identified. The patients’ characteristics are listed in Table 1. The EBUS-TBNA cases contributed by each center were: Milan, n=222; Bergamo, n=98; Varese, n=77; Brescia, n=58; Verona, n=30. Findings in the pooled series of the five centers were as follows: the first node station most frequently sampled was station 4 (45% of cases), followed by station 7 (32%). Station 2 nodes were biopsied in 6% of patients, station 10 in 13%, station 11 in 4%. No major complications were observed. In 49 patients the EBUS-TBNA sampling was found to be inadequate; thus, the rate of adequate samples overall was 90% (436/485). In 301 patients a diagnosis of malignant involvement of mediastinal nodes was obtained (true positive). In 105 cases the EBUS-TBNA result was true negative, in 30 cases it was false negative. In the pooled series of 485 EBUS-TBNAs the sensitivity, NPV and accuracy were respectively 90%, 78% and 93%.
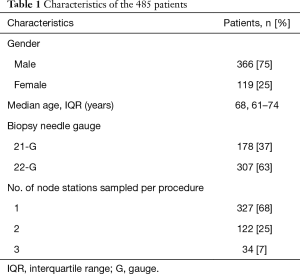
Full table
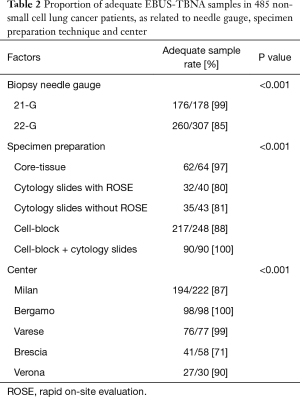
Table 2 summarizes the EBUS-TBNA diagnostic yield (rate of adequate samples) by needle gauge, by specimen processing technique and by center. A significant difference of diagnostic yield was observed comparing 21- vs. 22-G needle (P<0.001), the different specimen preparation techniques (P<0.001), and the five centers (P<0.001).
Full table
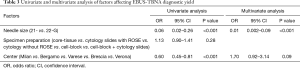
At multivariate analysis, 21-G needle correlated with better diagnostic yield, whereas specimen processing technique and center were not independent factors of EBUS-TBNA diagnostic yield (Table 3).
Full table
Discussion
In our pooled series of 485 lung cancer patients undergoing mediastinal staging for suspect N2 involvement, the EBUS-TBNA technique had 90% sensitivity, 78% NPV and 93% accuracy. To our knowledge this is the largest Italian series of analyzed EBUS-TBNA results, consisting exclusively of NSCLC patients with clearly defined criteria for study entry. Our results are well within the range of EBUS-TBNA sensitivity (52–92%), NPV (57–93%) and accuracy (84–96%) calculated from the data reported in a recent systematic review and meta-analysis (5). The generally high accuracy of EBUS-TBNA has led to wide diffusion of this technique for minimally invasive diagnosis and staging of NSCLC. For this purpose the ACCP evidence-based practice guidelines recommend EBUS-TBNA as the first choice method (6), while mediastinoscopy and other surgical approaches for mediastinal node biopsy are indicated for EBUS-TBNA negative cases at high risk of lung cancer metastases (7). Consequently, the number of mediastinoscopies has dropped significantly after the introduction of EBUS-TBNA for mediastinal staging of lung cancer (8).
In our pooled series of NSCLC patients undergoing mediastinal staging by EBUS-TBNA, the specimen processing technique and the center were not independent factors influencing diagnostic yield, in agreement with previous reports of EBUS-TBNA performance in heterogeneous populations of neoplastic and non-neoplastic patients (9,10). Needle 21-G independently correlated with the EBUS-TBNA diagnostic yield.
Regarding the needle gauge, our rate of adequate samplings with 21-G needle (99%) and with 22-G needle (85%) was higher than the respective rates reported in the literature (72% and 78%) (11). This difference is likely contributed to by the fact that our study population consisted exclusively of NSCLC patients. In our pooled series, the specimen adequacy rate was significantly higher with 21- relative to 22-G needle, in contrast with other authors’ findings (11-13).
ROSE of samples in our study was used in only 40 EBUS-TBNA cases in total, cumulated in Brescia and Verona centers, and this technique provided no significant advantage. However, our limited experience with ROSE does not allow firm conclusions about the role of this technique. A recent review indicates that ROSE does not modify EBUS-TBNA diagnostic yield and does not affect the number of needle passes, the duration of the procedure, nor the complication rate (9). Conversely, ROSE reduces the number of additional lymph node samplings, especially when EBUS-TBNA represents the first diagnostic procedure in case of suspect lung cancer (9).
Regarding the specimen processing techniques, cell-block was the most frequently used method in the pooled series. The other methods adopted for processing EBUS-TBNA specimens were cytology slides and core-tissue. In our study and in the literature, the comparison of cytology slides, core-tissue and cell-block methods showed that none of these preparation techniques was superior to the others (9,10). The combined reading of specimens prepared with two techniques (cytology slides and cell-block) leads to better diagnostic results, but it has the disadvantage of being more expensive and more time-consuming (14,15).
Concerning patient sedation, all centers in our study used conscious sedation with fentanyl and midazolam, obtaining overall an adequate sample rate of 90%, similar to that reported in the literature (16,17).
This study has limitations, mostly due to its retrospective nature. First, the five centers participating in the study did not follow a standardized EBUS-TBNA procedure, thus increasing the variability of diagnostic findings. Second, the results were obtained in a selected cohort entirely consisting of cancer patients; this selection may likely account for the high sensitivity of EBUS-TBNA that was recorded, because the diagnostic performance correlates with the prevalence of malignancy (18,19).
Conclusions
In this Italian multicentric study of patients with NSCLC, the EBUS-TBNA technique showed high sensitivity and accuracy as a diagnostic tool for mediastinal staging. Multivariate analysis showed significant correlation between use of 21-G needle and EBUS-TBNA diagnostic yield. Center and specimen processing method did not independently affect diagnostic yield, suggesting that these procedural steps could be decided according to the bronchoscopist’s and pathologist’s usual practice.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Ethical approval was not required, as this study was observational. De-identified data were used for analyzing the results. Individual patient consent was waived due to the retrospective nature of the study.
References
- Silvestri GA, Gonzalez AV, Jantz MA, et al. Methods for staging non-small cell lung cancer: Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2013;143:e211S-50S.
- De Leyn P, Dooms C, Kuzdzal J, et al. Revised ESTS guidelines for preoperative mediastinal lymph node staging for non-small-cell lung cancer. Eur J Cardiothorac Surg 2014;45:787-98. [Crossref] [PubMed]
- Goldstraw P, Crowley JJ. IASLC International Staging Project. The International Association for the Study of Lung Cancer International Staging Project on Lung Cancer. J Thorac Oncol 2006;1:281-6. [Crossref]
- Sanz-Santos J, Andreo F, Serra P, et al. False positive endobronchial ultrasound-guided real-time transbronchial needle aspiration secondary to bronchial carcinoma in situ at the point of puncture: a case report. J Cardiothorac Surg 2012;7:74. [PubMed]
- Dhooria S, Aggarwal AN, Gupta DA, et al. Utility and safety of endoscopic ultrasound with Bronchoscope-Guided Fine-Needle aspiration in mediastinal lymph node sampling: systematic review and Meta-Analysis. Respir Care 2015;60:1040-50. [Crossref] [PubMed]
- Detterbeck FC, Lewis SZ, Diekemper R, et al. Executive Summary: Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2013;143:7S-37S.
- Rusch VW. Mediastinoscopy: an obsolete procedure? J Thorac Cardiovasc Surg 2011;142:1400-2. [Crossref] [PubMed]
- Guarize J, Pardolesi A, Donghi S, et al. Endobronchial ultrasound for mediastinal staging in lung cancer patients. Multimed Man Cardiothorac Surg 2014.2014. [PubMed]
- van der Heijden EH, Casal RF, Trisolini R, et al. Guideline for the acquisition and preparation of conventional and endobronchial ultrasound-guided transbronchial needle aspiration specimens for the diagnosis and molecular testing of patients with known or suspected lung cancer. Respiration 2014;88:500-17. [Crossref] [PubMed]
- Wahidi MM, Herth F, Yasufuku K, et al. Technical aspects of endobronchial Ultrasound-Guided transbronchial needle aspiration CHEST guideline and expert panel report. Chest 2016;149:816-35. [Crossref] [PubMed]
- Oki M, Saka H, Kitagawa C, et al. Randomized Study of 21-gauge Versus 22-gauge Endobronchial Ultrasound-guided Transbronchial Needle Aspiration Needles for Sampling Histology Specimens. J Bronchology Interv Pulmonol 2011;18:306-10. [Crossref] [PubMed]
- Yarmus LB, Akulian J, Lechtzin N, et al. Comparison of 21-gauge and 22-gauge aspiration needle in endobronchial ultrasound-guided transbronchial needle aspiration: results of the American College of Chest Physicians Quality Improvement Registry, Education, and Evaluation Registry. Chest 2013;143:1036-43. [Crossref] [PubMed]
- Nakajima T, Yasufuku K, Takahashi RA, et al. Comparison of 21-gauge and 22-gauge aspiration needle during endobronchial ultrasound-guided transbronchial needle aspiration. Respirology 2011;16:90-4. [Crossref] [PubMed]
- Toth JW, Zubelevitskiy K, Strow JA, et al. Specimen processing techniques for endobronchial ultrasound-guided transbronchial needle aspiration. Ann Thorac Surg 2013;95:976-81. [Crossref] [PubMed]
- Rotolo N, Cattoni M, Crosta G, et al. Comparison of multiple techniques for endobronchial ultrasound-transbronchial needle aspiration specimen preparation in a single institution experience. J Thorac Dis 2017. [Epub ahead of print].
- Aswanetmanee P, Limsuwat C, Kabach M, et al. The role of sedation in endobronchial ultrasound-guided transbronchial needle aspiration: Systematic review. Endosc Ultrasound 2016;5:300-6. [Crossref] [PubMed]
- Yarmus LB, Akulian JA, Gilbert C, et al. Comparison of moderate versus deep sedation for endobronchial ultrasound transbronchial needle aspiration. Ann Am Thorac Soc 2013;10:121-6. [Crossref] [PubMed]
- Kennedy MP, Jimenez CA, Morice RC, et al. Factors Influencing the Diagnostic Yield of Endobronchial Ultrasound-guided Transbronchial Needle Aspiration. J Bronchology Interv Pulmonol 2010;17:202-8. [Crossref] [PubMed]
- Evison M, Crosbie P, Navani N, et al. How should performance in EBUS mediastinal staging in lung cancer be measured? Br J Cancer 2016;115:e9. [Crossref] [PubMed]


