Discordance of physician clinical judgment vs. pneumonia severity index (PSI) score to admit patients with low risk community-acquired pneumonia: a prospective multicenter study
Introduction
Community-acquired pneumonia (CAP) is a common disease and is associated with substantial morbidity, mortality and health care costs (1). Annual incidence of CAP admissions to hospitals has increased significantly in recent years (2). Annual spending for CAP hospital admissions exceeds $8.4 billion in the United States (3), and hospitalization accounts for a substantive portion of the total health care expenditures (4,5). Several clinical practice guidelines have emerged recommending use of a validated severity of illness scores to guide clinical decision-making about inpatient versus outpatient treatment of CAP (6,7). The most commonly recommended severity of illness scores are the pneumonia severity index (PSI) score and the CURB-65 (6,8-11). However, despite these validated severity of illness scores, several cohort studies have reported 26–62% of low risk CAP patients (PSI ≤2 or CURB-65 ≤1) are admitted to the hospital (12-17). High health care resource utilization and incremental costs are driven by these low risk CAP patients (16,18-20).
Several studies have evaluated the reasons why clinicians do not rely solely on pneumonia severity of illness scores to determine inpatient vs. outpatient treatment for CAP patients (16,18,21,22). Previous studies have shown that clinical judgment plays an important role in decision-making because severity of illness scores do not capture all important clinical risk factors to determine that most appropriate site for treatment (11). However, previous studies (12,13,16,21) are limited by several factors: (I) retrospective design; (II) small sample size; (III) different severity of illness scores; (IV) influence of physician preferences; (V) local hospital practices; and (VI) active participation in an intervention trial (23-25).
The objective of our study is to determine the clinical factors that influence physician decision-making to hospitalize low-risk patients (PSI ≤2) with CAP in a multicenter, prospective cohort study. Additionally, we will assess if the reason for admission was associated with poorer clinical outcomes.
Methods
Study design
This is a multicenter, prospective cohort study of patients hospitalized with CAP. Five public hospitals from Spain participated in the study: (I) Hospital A Coruña, a 1,382-bed teaching hospital serving a population of 514,466 people; (II) Complejo Hospitalario de Ourense, a 904-bed teaching hospital serving a population of 257,259; (III) Complejo Hospitalario de Pontevedra, a 622-bed community hospital serving a population of 225,499; (IV) Hospital del Bierzo, a 408-bed community hospital serving a population of ~150,000; and (V) Hospital do Barbanza, a 80-bed community hospital serving a population of 65,387. All patients signed an informed consent for entering into the study. The study protocol was approved by the Institutional Review Board (CEIC de Galicia #078/12).
Study population
Eligible subjects were patients hospitalized for CAP. Inclusion criteria were: (I) age >18 years; (II) diagnosis of CAP based on lower respiratory tract symptoms per guidelines (10); (III) pneumonia confirmed by chest radiograph within 24 h of admission; (IV) PSI score ≤2 indicative of low-severity CAP that should not require hospital admission per guidelines (6,7). Exclusion criteria were: (I) health-care associated pneumonia (26); and (II) admission for comfort care only. We excluded patients with health-care associated pneumonia due to important controversies surrounding this term and the risk of multi-drug resistant pathogens (27). If a patient had >1 admission during the study period, only the first hospitalization was included in the study.
Main objective and data collection
The main objective of our study was to determine the clinical factors that influence physician decision-making to hospitalize low-risk patients. During the study period, the standard approach to clinical decision-making about admission to the hospital was based solely on physician judgment without the use of pneumonia severity of illness scores, such as PSI or CURB-65. Research teams at each site assessed all patients admitted to the hospital with pneumonia from Monday to Friday. If a patient met all inclusion criteria, the principal investigator contacted the admitting physician within 24 hours of admission to collect data on the clinical factors that influenced decision-making to admit the patient despite the low severity of illness.
Data collected were: demographics, comorbidities, previous antibiotic treatment, oral intolerance, physical exam findings, arterial blood gas analysis, laboratory data, and chest radiographs. Additional data collected from the medical record were inpatient antibiotic regimen(s), length of hospital stay, admission to the intensive care unit (ICU), and 30- and 90-day, mortality and readmissions. Oral intolerance was defined as inability to administer oral antibiotic therapy. The PSI and CURB-65 scores were calculated on admission. Another severity of illness tool like the SMART-COP (28) score was calculated after the study finished.
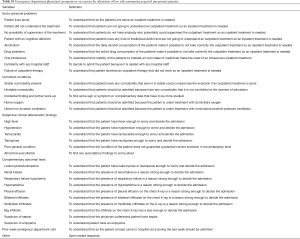
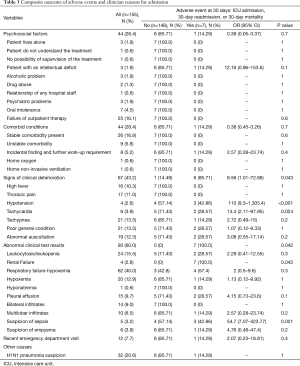
Reasons for admission were categorized into six principal categories with several subcategories (Table S1). The six main categories were: (I) psychosocial factors; (II) comorbid conditions; (III) signs of clinical deterioration findings; (IV) abnormal clinical test results; (V) repeat visit to the emergency department (ED) in the past 2 weeks; and (VI) other causes not included in other categories.
Full table
Clinical outcomes
We also wanted to see if there was a relationship between the specific reasons for admission and adverse events at 30 days (defined as a composite endpoint of ICU admission and 30-day readmission or death), hospital length of stay (LOS) and days of antibiotic therapy. Hospital LOS was calculated as the date of hospital discharge minus the date of hospital admission. Days of antibiotic therapy were calculated as the total number of days of inpatient treatment plus the total number of days of outpatient treatment prescribed at the time of hospital discharge.
Statistical analysis
Absolute numbers and percentages are summarized as categorical variables. Continuous variables are presented as means ± standard deviation (SD) or medians and interquartile ranges (IQR) when non-normally distributed. A prior test for normality of data distribution, the Kolmogorov-Smirnov test, was performed. Chi-squared and Fisher’s exact tests were employed to compare baseline data and reasons for admission with clinical outcomes. The composite outcome was defined as the dependent variable. The relationship between the composite outcome and those variables related with dependent variable were calculated with the Pearson or Spearman, when appropriate, correlation coefficient. All data were statistically analyzed with SPSS (version 18.0, Chicago, IL, USA) and STATA (version 13 STATA Corporation, College Station, TX, USA).
Results
Patient characteristics
During a two-year period, 155 patients were enrolled. Demographics, comorbid conditions, severity of disease, radiographic, physical and laboratory data on admission are summarized in Table 1. Patients were predominantly men (56.1%) with a median age of 45 year (IQR: 19–71). Twenty-five percent of patients had received previous outpatient antibiotic therapy. The most common clinical and laboratory findings on admission were respiratory failure (32%) and pleural effusion (10.3%). All patients had a PSI ≤2, 84.4% [147] had a CURB-65 of 0 or 1, and only 5% had a CURB-65 of 2.

Full table
Antibiotic therapy
Patients received antibiotics for a median of 11 days (IQR: 6–36 days), with two-third patients [101] receiving guideline-concordant treatment. The commonest empiric antibiotic regimen was levofloxacin monotherapy (60%), followed by a combination of a beta-lactam and a macrolide antibiotic (27.7%).
Reason for admission
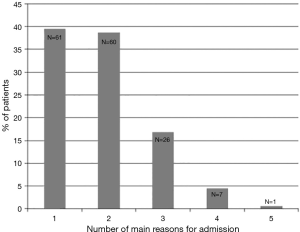
The reasons for admission are shown in Table 2. All patients had at least one primary reason for admission to the hospital according to their treating physician. Most patients had only 1 reason for hospital admission [61 patients (39.4%)], followed by 2 reasons [60 (38.7%)], or ≥3 reasons [34 (21.9%)] (Figure S1).
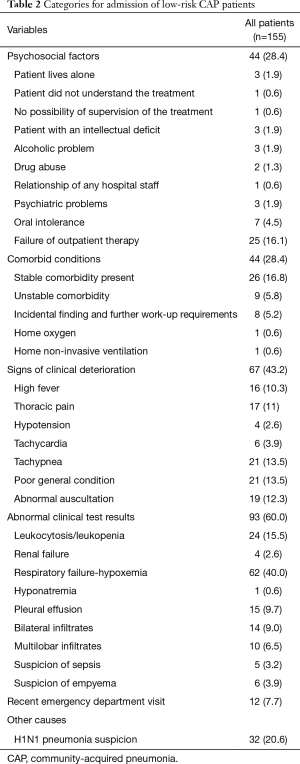
Full table
The most common reason for hospital admission was the presence abnormal clinical test results [93 (60%)], followed by abnormal physical exam findings [67 (43.2%)], comorbid conditions [44 (28.4%)] and psychosocial factors [44 (28.4%)] (Figure 1).
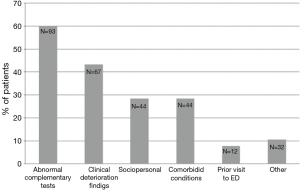
The most frequent reasons for admission within the group of abnormal clinical test results were respiratory failure/hypoxemia [62 (40%)] and leukocytosis [24 (15.5%)] The most common reasons for admission due to abnormal physical exam findings were tachypnea, poor general health condition, and abnormal auscultation findings (13.5%, 13.5%, and 12.3%, respectively). Most common comorbid conditions as the reason for admission were the presence of a stable or decompensated comorbidity (16.8% and 5.8%, respectively). The most frequent psychosocial factors for admission were failure of previously outpatient therapy [25 (16.1%)] and oral intolerance [7 (4.5%)].
Clinical outcomes
The composite outcome was detected in 7 (4.5%) patients [(3 (1.9%) patients were readmitted at 30 days, 4 (2.6%) had an ICU admission, and there were no deaths at 30 days]. The mean LOS in the hospital was 7.14±5.73 days. The calculated median LOS in the hospital was 6 days. No objective clinical parameters registered at the time of hospital admission were associated with the composite outcome (Table S2). Among the reasons for admission, only signs of clinical deterioration (r2=0.18; P=0.043) and abnormal clinical test results (r2=0.18; P=0.042) were associated with the composite outcome (Table 3). Specific reasons for admission associated with the composite outcome were hypotension (r2=0.34), tachycardia (r2=0.28), renal failure (r2=−0.03) and suspicion of sepsis (r2=0.48).

Full table
Full table
Discussion
Our study shows that low-risk CAP patients are often admitted to the hospital for multiple reasons. Several important clinical factors play a role in the clinical decision-making to admit a patient with CAP. However, poor clinical outcomes are not associated with the physicians’ reasons for admission. Most low-risk CAP patients admitted to the hospital had ≥2 reasons for admission according to their physicians. The categories of clinical reasons for admission associated with poorer clinical outcomes were the presence of abnormal clinical test results and signs of clinical deterioration.
Although a correlation has been demonstrated between PSI and CURB-65 scores and 30-day mortality risk, the evidence also suggests that physician judgment plays an important role in clinical decision-making to admit patients with CAP (29). The PSI score was designed to identify patients with CAP at low risk for mortality (30) and guide clinicians to manage these patients as outpatients. However, multiple studies have demonstrated that a considerable proportion of patients with low pneumonia severity of illness scores (PSI ≤2) are still admitted to the hospital (22,31-36). Additionally, cohort studies from different parts of the world, including the United Kingdom (22), Spain (33), and the United State (37), have reported hospitalization rates of low-risk CAP patients (PSI =1–3) to be 55%, 56%, and 66%, respectively. Implementation of evidence-based clinical guidelines has decreased hospitalization of low-risk CAP, but even in the best case scenario, the admission rate for low-risk CAP with PSI ≤2 remains high (23.9%) (14).
Several studies have tried to elucidate why patients are admitted to the hospital despite a low pneumonia severity of illness score. In a single center interventional trial, Halm et al. assessed reasons for admission of low risk CAP patients and showed the presence of active comorbidities (55%) was the main reason for admission (38). The study by Halm et al. included patients older than ours (40% >65 years) and they excluded patients who were considered inappropriate candidates for outpatient care due to an oxygen saturation <90% on room air, inability to take oral medications, recent hospitalization, psychiatric illness, substance abuse, neuromuscular disease, pregnancy, homelessness, or inaccessibility by telephone. Similar to our study, Halm et al. surveyed the physician to assess the reasons for admission of low-risk CAP patients.
In a retrospective observational study, Arnold et al. defined the clinical factors associated with admission of low-risk CAP patients with a PSI ≤2 (16). The main reasons for admission were psychosocial factors (45%) and comorbid conditions that required hospitalization (43%). This study differs from ours because the reasons for admission were adjudicated made by a committee retrospectively. Additionally, our study demonstrated that abnormal clinical test results were a primary reason for admission, rather than concern for comorbidities or psychosocial factors. For example, hypoxemia was the reason for admission in 63 (40.6%) patients in our study, compared with only 1 (1.5%) in Arnold’s study. Rosón et al. suggested that respiratory failure and pleural complications were the most common reasons for admission of low-risk CAP patients (39). Rosón et al. (39) concluded that 40% of low-risk CAP patients had no compelling reason for admission. Aujesky et al. (13) found that the presence of comorbidities was the main reason for admission in 71% of the patients with low-risk CAP defined as a PSI ≤3. In our study, we were able to differentiate at the time of admission if the comorbid conditions were stable vs. unstable, and if a new abnormal finding was detected, whether further work-up was indicated. Although it was prospective, the Aujesky et al. (13) study was an interventional trial and active participation in the trial could alter the results. Furthermore, study investigators contacted the ED a week after the hospitalization leading to potential recall bias, while our study investigators made contact with the ED in <24 hours. Recall bias may also explain why more patients in our study had >2 reasons for admission compared to the Aujesky study (21.9% vs. 15.7%) (13).
We would also like to highlight that the second most common reason for admission, after respiratory failure, was the suspicion of H1N1 Influenza A virus as the causative microorganism of pneumonia. Although this reason for admission was not listed in the original study protocol, it was frequently reported in the “other” category for admission. We have to remember that our study was conducted during the worldwide H1N1 influenza pandemic.
We believe that clinical judgement is influenced by the experience and the knowledge of the staff that admitted pneumonia patients. In our cohort most of the admitting physicians were not residents (70%), and most of them were specialist in internal medicine (45%), followed by pulmonologist (22%).
Our study has some limitations to recognize. Even though this was a multicenter study, all of the hospitals were in Spain, and this data may have limited applicability to other populations, countries, or healthcare systems. Second, the admitting physicians were requested to explain all reasons for admission but ranking of the reasons was not performed. Third, although it was a multicentre study in five hospitals attending an important population, the number of patients included was low (n=155); this can be explained by (I) we only included patients that were specifically admitted to the investigator hospital ward, so it could be a proportion of admitted patients in another services that we did not evaluated; (II) with the aim of selecting the pneumonias with the lowest severity we excluded patients with PSI =3, patients that similar studies has mostly times included; and (III) we excluded weekend admissions. Finally, selection bias may be present because of two aspects, first one is that the decision of admission was not based on the use of clinical scales meaning a poor implementation of objective severity scores but reflecting a real scenario in clinical practice; and second, weekend admissions were excluded; however, we do not feel this is a major limitation because the same physicians were admitting patients during the weekdays and weekends.
Conclusions
Our study is the first multicentre prospective study, specially focused on detecting the causes for admission in low risk CAP patients which demonstrates that there are multiples reasons for admission of low-risk CAP patients despite a low PSI score. These reasons for admission are not accounted for by the severity of illness scores for CAP. Abnormal clinical test results and signs of clinical deterioration are two specific reasons for admission that may be associated with poorer clinical outcomes in certain patients. Additional studies are needed to assess the generalizability of our results to other populations and healthcare systems.
Acknowledgements
The investigators would like to acknowledge the Sociedade Galega do Aparato Respiratorio (SOGAPAR) with their “Annual Research Awards” for their contribution to the development of the study.
Funding: Dr. Restrepo is partially protected by Award Number K23HL096054 from the National Heart, Lung, And Blood Institute.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the Institutional Review Board (CEIC de Galicia #078/12) and written informed consent was obtained from all patients.
References
- Almirall J, Bolibar I, Vidal J, et al. Epidemiology of community-acquired pneumonia in adults: a population-based study. Eur Respir J 2000;15:757-63. [Crossref] [PubMed]
- Fry AM, Shay DK, Holman RC, et al. Trends in hospitalizations for pneumonia among persons aged 65 years or older in the United States, 1988-2002. JAMA 2005;294:2712-9. [Crossref] [PubMed]
- Niederman MS, McCombs JS, Unger AN, et al. The cost of treating community-acquired pneumonia. Clin Ther 1998;20:820-37. [Crossref] [PubMed]
- Lave JR, Lin CCJ, Fine MJ, et al. The cost of treating patients with community-acquired pneumonia. Semin Respir Crit Care Med 1999;20:189-97. [Crossref]
- Kozma CM, Dickson M, Raut MK, et al. Economic benefit of a 1-day reduction in hospital stay for community-acquired pneumonia (CAP). J Med Econ 2010;13:719-27. [Crossref] [PubMed]
- Mandell LA, Wunderink RG, Anzueto A, B, et al. Infectious Diseases Society of America/American Thoracic Society Consensus Guidelines on the Management of Community-Acquired Pneumonia in Adults. Clin Infect Dis 2007;44:S27-72. [Crossref] [PubMed]
- Woodhead M, Blasi F, Ewig S, et al. Guidelines for the management of adult lower respiratory tract infections. Eur Respir J 2005;26:1138-80. [Crossref] [PubMed]
- Woodhead M, Blasi F, Ewig S, et al. Guidelines for the management of adult lower respiratory tract infections. Clin Microbiol Infect 2011;17:E1-59. [Crossref] [PubMed]
- Carratalà J, Fernandez-Sabe N, Ortega L, et al. Outpatient care compared with hospitalization for community-acquired pneumonia: a randomized trial in low-risk patients. Ann Intern Med 2005;142:165-72. [Crossref] [PubMed]
- Singanayagam A, Chalmers JD. Severity assessment scores to guide empirical use of antibiotics in community acquired pneumonia. Lancet Respir Med 2013;1:653-62. [Crossref] [PubMed]
- Labarere J, Stone RA, Obrosky DS, et al. Comparison of outcomes for low-risk outpatients and inpatients with pneumonia: A propensity-adjusted analysis. Chest 2007;131:480-8. [Crossref] [PubMed]
- Aliberti S, Ramirez J, Cosentini R, et al. Low CURB-65 is of limited value in deciding discharge of patients with community-acquired pneumonia. Respir Med 2011;105:1732-8. [Crossref] [PubMed]
- Aujesky D, McCausland JB, Whittle J, et al. Reasons Why Emergency Department Providers Do Not Rely on the Pneumonia Severity Index to Determine the Initial Site of Treatment for Patients with Pneumonia. Clin Infect Dis 2009;49:e100-8. [Crossref] [PubMed]
- Renaud B, Coma E, Labarere J, et al. Routine use of the Pneumonia Severity Index for guiding the site-of-treatment decision of patients with pneumonia in the emergency department: a multicenter, prospective, observational, controlled cohort study. Clin Infect Dis 2007;44:41-9. [Crossref] [PubMed]
- Seymann G, Barger K, Choo S, et al. Clinical Judgment versus the Pneumonia Severity Index in Making the Admission Decision. J Emerg Med 2008;34:261-8. [Crossref] [PubMed]
- Arnold FW. Hospitalization for Community-Acquired Pneumonia: The Pneumonia Severity Index vs Clinical Judgment. Chest 2003;124:121-4. [Crossref] [PubMed]
- Restrepo MI, Mortensen EM, Velez JA, et al. A Comparative Study of Community-Acquired Pneumonia Patients Admitted to the Ward and the ICU. Chest 2008;133:610-7. [Crossref] [PubMed]
- Sanz F, Restrepo MI, Fernandez E, et al. Is it possible to predict which patients with mild pneumonias will develop hypoxemia? Respir Med 2009;103:1871-7. [Crossref] [PubMed]
- Menéndez R, Cremades MJ, Martinez-Moragon E, et al. Duration of length of stay in pneumonia: Influence of clinical factors and hospital type. Eur Respir J 2003;22:643-8. [Crossref] [PubMed]
- Marcos PJ, Restrepo MI, Sanjuan P, et al. Community-acquired pneumonia team decreases length of stay in hospitalized, low-risk patients with pneumonia. Hosp Pract (1995) 2013;3:7-14. [PubMed]
- Choudhury G, Chalmers JD, Mandal P, A, et al. Physician judgement is a crucial adjunct to pneumonia severity scores in low-risk patients. Eur Respir J 2011;38:643-8. [Crossref] [PubMed]
- Singanayagam A, Chalmers JD, Hill AT. Admission hypoglycaemia is associated with adverse outcome in community-acquired pneumonia. Eur Respir J 2009;34:932-9. [Crossref] [PubMed]
- Marcos PJ, Restrepo MI, Verea H. Community acquired pneumonia: severity scores as an adjunct to clinical judgement. Eur. Respir J 2012;39:509. [Crossref] [PubMed]
- Bewick T, Cooper VJ, Lim WS. Does early review by a respiratory physician lead to a shorter length of stay for patients with non-severe community-acquired pneumonia? Thorax 2009;64:709-12. [Crossref] [PubMed]
- Menéndez R, Torres A, Zalacain R, et al. Guidelines for the treatment of community-acquired pneumonia: predictors of adherence and outcome. Am J Respir Crit Care Med 2005;172:757-62. [Crossref] [PubMed]
- American Thoracic Society. Infectious Diseases Society of America. Guidelines for the Management of Adults with Hospital-acquired, Ventilator-associated, and Healthcare-associated Pneumonia. Am J Respir Crit Care Med 2005;171:388-416. [Crossref] [PubMed]
- Chalmers JD, Rother C, Salih W, et al. Healthcare-associated pneumonia does not accurately identify potentially resistant pathogens: a systematic review and meta-analysis. Clin Infect Dis 2014;58:330-9. [Crossref] [PubMed]
- Charles PG, Wolfe R, Whitby M, et al. SMART-COP: a tool for predicting the need for intensive respiratory or vasopressor support in community-acquired pneumonia. Clin Infect Dis 2008;47:375-84. [Crossref] [PubMed]
- Chalmers JD, Rutherford J. Can we use severity assestment tools to increase outpatient management of community-acquired pneumonia. Eur J Intern Med 2012;23:398-406. [Crossref] [PubMed]
- Fine MJ, Auble TE, Yealy DM, et al. A prediction rule to identify low-risk patients with community-acquired pneumonia. N Engl J Med 1997;336:243-50. [Crossref] [PubMed]
- Marrie TJ, Lau CY, Wheeler SL, et al. A controlled trial of a critical pathway for treatment of community-acquired pneumonia. CAPITAL Study Investigators. Community-Acquired Pneumonia Intervention Trial Assessing Levofloxacin. JAMA 2000;283:749-55. [Crossref] [PubMed]
- Arnold FW, Brock GN, Peyrani P, et al. Predictive accuracy of the pneumonia severity index vs CRB-65 for time to clinical stability: Results from the Community-Acquired Pneumonia Organization (CAPO) International Cohort Study. Respir Med 2010;104:1736-43. [Crossref] [PubMed]
- Menéndez R, Torres A, Reyes S, et al. Compliance with Guidelines-Recommended Processes in Pneumonia: Impact of Health Status and Initial Signs. PLoS One 2012;7:e37570. [Crossref] [PubMed]
- Restrepo MI, Mortensen EM, Pugh JA, et al. COPD is associated with increased mortality in patients with community-acquired pneumonia. Eur Respir J 2006;28:346-51. [Crossref] [PubMed]
- Buising KL, Thursky KA, Black JF, et al. A prospective comparison of severity scores for identifying patients with severe community acquired pneumonia: reconsidering what is meant by severe pneumonia. Thorax 2006;61:419-24. [Crossref] [PubMed]
- Marcos PJ, Restrepo MI, Anzueto A. Community-Acquired Pneumonia Requiring Hospitalization. N Engl J Med 2015;373:2380-1. [Crossref] [PubMed]
- Jain S, Self WH, Wunderink RG, et al. Community-Acquired Pneumonia Requiring Hospitalization among U.S. Adults. N Engl J Med 2015;373:415-27. [Crossref] [PubMed]
- Halm EA, Atlas SJ, Borowsky LH, et al. Understanding physician adherence with a pneumonia practice guideline: effects of patient, system, and physician factors. Arch Intern Med 2000;160:98-104. [Crossref] [PubMed]
- Rosón B, Carratalà J, Dorca J, et al. Etiology, reasons for hospitalization, risk classes, and outcomes of community-acquired pneumonia in patients hospitalized on the basis of conventional admission criteria. Clin Infect Dis 2001;33:158-65. [Crossref] [PubMed]