Bicuspid aortic root spared during ascending aorta surgery: an update of long-term results
Introduction
Bicuspid aortic valve (BAV) is the most common congenital heart defect with an estimated prevalence of 0.5–2% of the general population (1). Relationship between BAV and dilation of proximal aorta is well described in literature and recently defined as “bicuspid aortic valve syndrome”. The clarification of the natural history aspects of BAV disease is fundamental to better understand the clinical outcomes of patients that are, most of the times, young and asymptomatic (1,2). Michelena and co-authors have recently described the natural history of patients with normally-functioning BAV (3). In this large population based study, about 5% of patients underwent isolated aortic surgery during life: in this rare subgroup, an intervention on the ascending aorta was necessary in absence of dysfunction of the BAV. Managing this subcategory of patients faced the cardiac surgeon to the possibility of preserve a not-malfunctioning but congenitally altered root. With this report, we would like to clarify what can we expect from a conservative approach on a bicuspid root.
Patients and methods
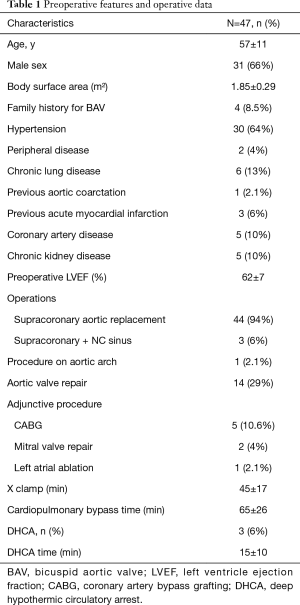
We identified a group of 47 patients (mean age 57±11 y; range, 35–81 y; 31 males) who were treated by means of supracoronary aortic replacement in presence of a normally functioning BAV and not significantly enlarged sinus of Valsalva (mean diameter 41±4 mm) from 1996 to 2015. Among them, three patients underwent Emi-Yacoub procedure for the presence of an asymmetrical dilation of aortic root with a more fragile wall detected only in non-coronary sinus. An adjunctive subcommissural annuloplasty was moreover performed in 14 cases for the presence of a mild aortic regurgitation (AR) due to dilation of sino-tubular junction (no leaflet pathology was present). Table 1 resumes the main preoperative features.
Full table
Study design and statistical analysis
Data from our institutional database regarding preoperative features, intraoperative characteristics and postoperative outcomes were analyzed retrospectively.
Clinical follow-up (mean 93±50 months; range, 21–207) was 98.9% complete. All survivor patients underwent clinical examination and echocardiographic exam during years.
Statistical analysis was performed with Stat View 4.5 (SAS Institute Inc., Abacus Concepts, Berkeley, CA, USA).
Freedom from all-cause mortality, cardiac death (all unknown cause deaths were considered as cardiac), need of new interventions and occurrence of major adverse cardiac and cerebrovascular events during the follow-up period were expressed as mean values plus or minus 1 standard deviation and computed using the Kaplan-Meier method.
Results
Mean aortic clamp was 45±17 min while mean CPB time was 65±26 minutes.
In hospital survival was 100%. Pre-discharge echoes showed no cases of significant AR (>2+) or stenosis.
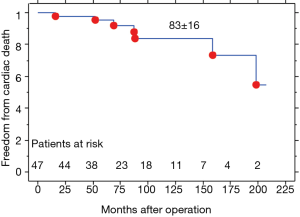
Freedom from cardiac death at 5- (60 months) and 10-year (120 months) was 95%±5% and 83%±16% respectively (Figure 1).
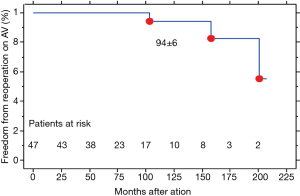
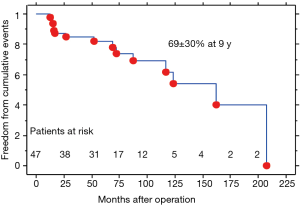
During follow up period, three patients required reoperation for the development of aortic insufficiency [2 cases treated by aortic valve replacement (AVR)] and one for progression of aortic stenosis (AS) which was treated by means of transcatheter aortic valve implantation (TAVI) procedure. Table 2 resumes features of redo operation. Freedom from new procedure on aortic valve was 100% and 94.4%±5.6% at 5- (60 months) and 10-year (120 months) (Figure 2). Freedom from thromboembolic or bleeding events was 100% and 95%±5% at 5- and 10-year. No cases of endocarditis, acute aortic syndromes and new onset of dilation of sinuses on Valsalva were observed. Composite event-free survival (Figure 3) at 5- and 9-year was 82%±18% and 69%±30% (3 cardiac deaths; 2 not cardiac deaths; 3 deaths for unknown causes; 1 ictus cerebri; 3 reoperations; 1 rehospitalization). No differences were detected between patients treated with adjunctive aortic annuloplasty or Emi-Yacoub procedure and those treated just by ascending aorta replacement (AAR). At follow-up, all survivor patients were clinically stable with mean NYHA class 1.3±0.6.

Full table
Discussion
Relationship between BAV and dilation of proximal aorta is well described in literature. Clarify of all the aspects of BAV disease is fundamental for the definition of clinical outcomes of patients (1,2). Michelena and Co-Workers have well described the natural history of patients with normally-functioning BAV. In these series about 5% of patients underwent isolated aortic surgery during life: this is the subcategory of patients that we are focusing on (3).
Fate of BAV spared at the time of surgery was analyzed by Veldtman and co-workers on a series of 21 patients, reporting a 95% freedom from reoperation at 5 years follow-up (4).
Recently we have reported a series of 40 consecutive patients treated by means of AAR with conservative approach on BAV and sinus of Valsalva. In our previous series two surviving patients (5%) required reoperation for the development of aortic insufficiency during follow-up (median 62 months; range, 7–175) with a freedom from AVR of 100% and 90%±10% respectively at 5 and 10 years, no need of new intervention on sinus of Valsalva and a linear risk of adverse event of about 1.2–1.5% per year (5). Based on our findings, sparing a BAV during proximal aorta surgery is a reasonable option with a low risk of the progression of pathology and reoperation during a long-term period of follow-up (5,6).
In these reports, we have analysed data of 47 patients, treated in an eighteen years period, with a mean follow up of 93±50 months.
This report represents an important update of previous described experience and strongly confirms that the bicuspid aortic root, if non-dilated at the time of surgery without area of localized alteration of aortic wall and in presence of a really normally functioning valve (no increased gradient, <3+ AR), can be spared with optimal long-term integrity. The elongation of follow-up elsewhere described showed an improvement of freedom from new procedure on aortic valve and absence of new occurrence of root dilation.
It is very interesting that we have also described a case of progression of AS that was successfully treated by TAVI. To the best our knowledge this is the longest follow-up report of such progression of disease in this particular situation and the first time that TAVI solution was proposed and successfully applied. In presence of a possible severe progression of pathology of a BAV after many years from first surgical operation, we believe that TAVI is a reasonable therapeutic strategy (7).
In the present series, we did not observe significant enlargement of spared sinus of Valsalva needing for new intervention. This evidence suggests that, during management of bicuspid aortic aneurysm, when an isolated ascending phenotype is detected, long-term durability of root and valve are similar to a biological valved graft and represents a good option especially in older patient.
This data seems to be in line with the more specific criteria included in the 2012 European Society of Cardiology/European Association for CardioThoracic Surgery guidelines for management of valve diseases regarding the indication for ascending aorta pathology (8). The cut-off is set at 55 mm, or 50 mm in the case of associated coarctation, family history of dissection, hypertension or growth rate greater than 2 mm/year, or 45 mm in the case of valve surgery. However, the level of evidence supporting current recommendations is still inadequate and guidelines are mostly derived from expert consensus. In our work, the average aortic root diameter is in all cases clearly below 4.5 cm, hence no recommendation exists for our population and the absence of new reoperation of aortic root is in favour of this approach.
Unfortunately, no independent risk factors for reoperation emerged during statistical analysis.
Our study has several limitations: first of all, it is retrospective and not randomized one. Moreover, we just performed a clinical follow-up and not an echocardiographic or radiologic FU. We would like also to assess that at 10 years patients at risk were about 20% of the population and for this reason further studies with larger number of patients and longer follow-up are necessary to better understand the real nature of this pathology.
Conclusions
In conclusion, our data show that, although in the setting of a BAV aortopathy, aortic root integrity seems to remain stable during long term follow up with low rate of reoperation and occurrence of new adverse event (valve and aortic related). TAVI could be a possible option for the “redo” procedure. Conservative approach on bicuspid aortic root is a reasonable option for patients with BAV aortopathy and isolated ascending aorta phenotype.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Siu SC, Silversides CK. Bicuspid aortic valve disease. J Am Coll Cardiol 2010;55:2789-800. [Crossref] [PubMed]
- Della Corte A, Body SC, Booher AM, et al. Surgical treatment of bicuspid aortic valve disease: knowledge gaps and research perspectives. J Thorac Cardiovasc Surg 2014;147:1749-57, 1757.e1.
- Michelena HI, Desjardins VA, Avierinos JF, et al. Natural history of asymptomatic patients with normally functioning or minimally dysfunctional bicuspid aortic valve in the community. Circulation 2008;117:2776-84. [Crossref] [PubMed]
- Veldtman GR, Connolly HM, Orszulak TA, et al. Fate of bicuspid aortic valves in patients undergoing aortic root repair or replacement for aortic root enlargement. Mayo Clin Proc 2006;81:322-6. [Crossref] [PubMed]
- Russo M, Bertoldo F, Nardi P, et al. Fate of Normally Functioning Bicuspid Aortic Valve in Patients Undergoing Ascending Aorta Surgery. J Heart Valve Dis 2015;24:570-6. [PubMed]
- Nardi P, Pellegrino A, Russo M, et al. Midterm results of different surgical techniques to replace dilated ascending aorta associated with bicuspid aortic valve disease. Ann Thorac Surg 2013;96:1648-54. [Crossref] [PubMed]
- Nardi P, Russo M, Saitto G, et al. Transcatheter aortic valve replacement for a bicuspid aortic valve following replacement of the ascending aorta. J Card Surg 2017;32:355-7. [Crossref] [PubMed]
- Joint Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology (ESC). Guidelines on the management of valvular heart disease (version 2012). Eur Heart J 2012;33:2451-96. [Crossref] [PubMed]