Severe intraoperative complications during VATS Lobectomy compared with thoracotomy lobectomy for early stage non-small cell lung cancer
Introduction
The technique of video-assisted thoracic surgery (VATS) has evolved from the use in biopsy or wedge resection to lobectomy, now regularly performed including complex cases such as sleeve resection (1). With the safety of VATS established, more and more thoracic surgeons have learned VATS lobectomy, and the percentage of lobectomies performed by VATS continues to increase (2). Recent studies have confirmed that VATS possesses clear advantages compared to thoracotomy, such as shorter hospital stay, less perioperative complications and less pain (3-6). Recent meta-analysis studies suggest improved outcomes for VATS in terms of systemic recurrence and 5-year overall survival when compared to open thoracotomy for selected patients with early stage non-small cell lung cancer (NSCLC) (7,8). However, most of these studies have concentrated on postoperative complications and prognosis, while the concerning of severe intraoperative complications was limited (9). In this study, we retrospectively compared the intra-operative complication during lobectomy underwent through VATS or open thoracotomy in single center.
Patients and methods
This study was approved by the ethics committee of the China-Japan Friendship Hospital. From February 2008 to June 2012, all of patients with postoperative stage Ia-IIa NSCLC who underwent lobectomy in China-Japan Friendship Hospital were included. The operative approach related to surgeon’s experience and hobby, included open thoracotomy, VATS and VATS converted to open. Open thoracotomies were performed through regular posterior-lateral incision. VATS was performed through 2 or 3 ports. Incision of converted open cases was performed based to the position of VATS ports. Systemic lymph nodes dissection was performed in all malignant cases. All surgeons who performed the procedures were skilled with open thoracotomy but in different phase of VATS learning curve (10). A severe complication was defined as an event that resulted in an additional unplanned major surgical procedure other than the planned lobectomy. Sex, age, type of histology, resected lobe, operative time, blood loss and severe intraoperative complication were compared between groups.
Statistical analysis was performed with SPSS version 19.0 (SPSS Inc., Chicago, IL, USA). T tests and χ2 test were computed to examine intergroup differences in operative time, blood loss volume and severe intraoperative complication.
Results
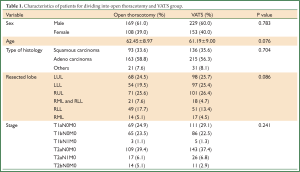
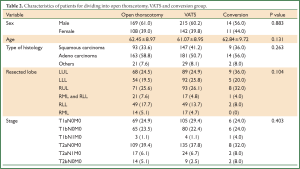
During this period, 659 lobectomies were performed. Among these, 277 performed through open thoracotomy, 357 performed through VATS, and 25 performed through VATS converted to open (Table 1). The VATS group was further divided into two subgroups, the completed VATS group and conversion group, and the compared data are shown in Table 2. There were no deaths. Ten severe intraoperative complications were identified, 4 occurred in open group, 6 occurred in VATS group.
Full Table
Full Table
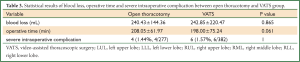
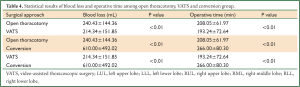
In our study, the operative time which was defined from cutting skin to the last stitch finished, did not have statistical difference comparing between VATS lobectomy and open thoracotomy approach even the conversion cases were included in VATS group (208.05±61.97 vs. 198.00±75.24, P=0.061) (Table 3), but the complete VATS group was significant shorter than the open group (193.24±72.64 vs. 208.05±61.97, P<0.01), and the open group was significant shorter than the conversion group (208.05±61.97 vs. 266.00±80.30, P<0.01) (Table 4). For blood loss, VATS group (including conversion cases) had similar statistical result comparing with open group (242.85±220.47 vs. 240.43±144.36, P=0.865) (Table 3), also the complete VATS group was significant less than open group (214.34±151.85 vs. 240.43±144.36, P<0.01), and the open group was significant less than the conversion group (240.43±144.36 vs. 610.00, and t, P<0.01) (Table 4).
Full Table
Full Table
Six severe intraoperative complications during VATS lobectomy occurred. There was an equal distribution of severe intraoperative complications among all 4 surgeons at different phases of learning curve.
Patient 1 was undergoing a right upper lobectomy. Transection of right upper lobe vein was performed successfully. Bleeding ensued in the process of dissection of pulmonary truncal artery secondary to severe adhesions. Thoracotomy was performed. On inspection, a portion of the wall of the pulmonary artery had been damaged, necessitating intrapericardial proximal arterial control. The rupture was overseen and right upper lobectomy was completed. Patient 2 was ongoing left upper lobectomy. An injury to the first branch of pulmonary artery was occurred during dissection, resulted in a tear that required a thoracotomy to control and repair. Left upper lobectomy was completed subsequently. Patient 3 was ongoing left lower lobectomy. Transection of inferior pulmonary vein was performed successfully. The posterior segmental branch of the pulmonary artery was injured during dissection of inferior bronchus since severe adhesion. Conversion was performed and bleeding was controlled. Then left lower lobectomy was completed.
Patient 4 was undergoing right upper lobectomy. Transection of the superior pulmonary vein, bronchus, and truncus artery were performed successfully. The posterior ascending branch of the pulmonary artery was injured during dissection secondary to adherent lymph nodes. Thoracotomy was performed to suture the artery and right upper lobectomy was completed subsequently.
Patient 5 underwent a right upper lobectomy. The azygos vein was inadvertently injured during dissection of hilum. Thoracotomy was performed. The rupture of azygos vein was too serious to repair and transection was completed. Then, right upper lobectomy was performed successfully.
Patient 6 underwent left lower lobectomy. Transection of the inferior pulmonary vein and artery was performed successfully. The left main stem bronchus was inadvertently transected, instead of the left lower lobe bronchus, even after the test of inflating the lung. A thoracotomy was performed. The left lower lobectomy was completed. The bronchial staple lines of the left main stem bronchus and the left upper lobe branch were removed. A primary anastomosis of the left upper lobe branch to the left main stem bronchus was performed, sparing the left upper lobe.
Four severe intraoperative complications in open thoracotomy group were all related to pulmonary artery when upper lobectomies were performed. One was during right upper lobectomy, when the first branch of pulmonary artery was injured at the junction to the right main pulmonary artery, necessitating intrapericardial proximal arterial control. The rupture was oversewn and right upper lobectomy was completed. The other 3 patients were undergoing left upper lobectomy. The conjunctions of first branches of the pulmonary artery to the left main pulmonary artery were injured since adhesion. Intrapericardial proximal arterial control was needed in two cases. All ruptures were oversewn and left upper lobectomies were completed.
Discussion
Severe intraoperative complications of VATS lobectomy occur infrequently, hence seldom mentioned in studies comparing VATS and the open procedure. The conversion of VATS to open lobectomy to manage bleeding may assign these patients to the open group for analysis, but converted patients should be analyzed with the VATS group (11,12). On the contrary, for open group, cases would be included even severe intraoperative complication occurred. If inappropriately analyzed, the safety of VATS lobectomy would be overestimated due to selection bias. In addition, severe intraoperative complication during VATS group usually needs VATS to be converted to the open thoracotomy, and manage on inspection, the operative time and blood loss could be increased compared with open procedures. Therefore, the severe intraoperative complication during VATS lobectomy should be focused more carefully, rather than eliminated as a fortuitous event.
Our study demonstrated the incidence of severe intraoperative complications during VATS lobectomy and open lobectomy were 1.57% (6/382) and 1.44% (4/277), respectively. There was no significant difference statistically. This result demonstrated the safety of VATS lobectomy was similar to open procedure preliminary, although the overall sample size was limited. Beside one unexpected injury on main stem of bronchus, others severe intraoperative complications were all related to the injury of vessels (9/10). Major of these complication occurred during upper lobectomy (8/10), only 2 occurred during lower lobectomy, which indicated more branches of pulmonary artery for upper lobe and varied pulmonary artery to upper lobe could be one of the most important reason of severe intraoperative complication during lobectomy no matter through VATS or thoracotomy approach. In VATS group, 3 severe intraoperative complications occurred since severe adhesion and 2 since adherent calcified lymph nodes, which indicate adhesion and calcified lymph nodes which adherent to pulmonary artery could be another important reason for severe intraoperative complication during VATS lobectomy.
Flores and colleagues (13) performed a retrospective study of catastrophic intraoperative complications during VATS lobectomy, including injury of vessels (8/12), bronchus (3/12) and abdominal organs. Overall incidence of catastrophic intraoperative complications was 1%, which was similar to our result. 7 of 8 cases of vessel injury were occurred during upper lobectomy, which was also similar to our result, indicated varied vessel of upper lobe induced more frequently injury during upper lobectomy. In Kim’s study (14), the incidence rate of severe complications was also similar to our data (1.49%, 11/740), which included 10 cases of pulmonary arterial hemorrhage and 1 case of main bronchial injury.
We tried to find the relationship between the severe intraoperative complications during VATS lobectomy and the level of surgeon’s experience or learning curve. 6 severe intraoperative complications during VATS lobectomy occurred. There was an equal distribution of severe intraoperative complications among all 4 surgeons at different phases of learning curve. Hence, we could not build up the relation between severe intraoperative complication during VATS lobectomy and the level of surgeon’s experience or phase of learning curve (10).
Some reports focused on successful completed VATS lobectomy and eliminated conversion cases when investigated the advantage of VATS lobectomy. But the reasons of these eliminated conversions might include injury of vessels and/or bronchus, adherent lymph node, severe thoracic adhesion and injury of other organs, etc, which induced more complex procedure that even could not be completed through VATS. Opposite of the benefits from VATS, conversion cases could have longer operative time and more blood loss since the attempt of VATS comparing with open thoracotomy approach. Also the difficulty of VATS lobectomy could be underestimated since the elimination of conversion cases. Although some studies (15) demonstrated VATS lobectomy had better results of operative time and incidence of complications comparing with open thoracotomy, the advantage of VATS could also be overestimated since the elimination of conversion cases. In our study, the operative time of VATS lobectomy did not have statistical difference comparing with open thoracotomy approach even the conversion cases were included in VATS group, but the complete VATS group was significant shorter than the open group. For blood loss, VATS group (including conversion cases) had similar statistical result comparing with open group, also the complete VATS group was significant less than open group. This result exactly demonstrates that the advantage of VATS could be overestimated if the conversion cases eliminated from VATS group.
In 2010, Gopeldas and colleagues (16), using the Healthcare Cost and Utilization Project Nationwide Inpatient Sample database, concluded that VATS lobectomy was associated with a greater number of intraoperative complications than open lobectomy, while the mortality and hospital stay period did not have significant deference. Even though the definition of intraoperative complications in this study was ambiguous, the level of thoracic expertise as reflected by the rate of VATS lobectomy was lower (6%) than what is available in the STS database (20%), the database may not capture the desired end points accurately in as much as its primary purpose was to address health care costs.
Our study preliminary demonstrated the incidence of severe intraoperative complication during VATS lobectomy was low and similar to open lobectomy. The severe intraoperative complications during VATS lobectomy are manageable and surgeon needs to take proper caution in performing VATS lobectomies. The safety of VATS lobectomy was proved again with this retrospective study, but further well-designed trials (e.g., prospective randomized controlled trials) are needed.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Solaini L, Prusciano F, Bagioni P, et al. Video-assisted thoracic surgery (VATS) of the lung: analysis of intraoperative and postoperative complications over 15 years and review of the literature. Surgical endoscopy 2008;22:298-310. [PubMed]
- Boffa DJ, Allen MS, Grab JD, et al. Data from The Society of Thoracic Surgeons General Thoracic Surgery database: the surgical management of primary lung tumors. J Thorac Cardiovasc Surg 2008;135:247-54. [PubMed]
- Hartwig MG, D’Amico TA. Thoracoscopic lobectomy: the gold standard forearly-stage lung cancer? Ann Thorac Surg 2010;89:S2098-101. [PubMed]
- Flores RM, Park BJ, Dycoco J, et al. Lobectomy by video-assisted thoracic surgery (VATS) versus thoracotomy for lung cancer. J Thorac Cardiovasc Surg 2009;138:11-8. [PubMed]
- Ilonen IK, Räsänen JV, Knuuttila A, et al. Anatomic thoracoscopic lung resection for non-small cell lung cancer in stage I is associated with less morbidity and shorter hospitalization than thoracotomy. Acta Oncol 2011;50:1126-32. [PubMed]
- Villamizar NR, Darrabie MD, Burfeind WR, et al. Thoracoscopic lobectomy is associated with lower morbidity compared with thoracotomy. J Thorac Cardiovasc Surg 2009;138:419-25. [PubMed]
- Yan TD, Black D, Bannon PG, et al. Systematic review and meta-analysis of randomized and nonrandomized trials on safety and efficacy of video-assistedthoracic surgery lobectomy for early-stage non-small-cell lung cancer. J Clin Oncol 2009;27:2553-62. [PubMed]
- Cao C, Manganas C, Ang SC, et al. A meta-analysis of unmatched and matched patients comparing video-assisted thoracoscopic lobectomy and conventional open lobectomy. Ann Cardiothorac Surg 2012;1:16-23.
- Dunning J, Walker WS. Pulmonary artery bleeding caused during VATS lobectomy. Ann Cardiothorac Surg 2012;1:109-10.
- Petersen RH, Hansen HJ. Learning curve associated with VATS lobectomy. Ann Cardiothorac Surg 2012;1:47-50.
- Flores RM, Ihekweazu UN, Rizk N, et al. Patterns of recurrence andincidence of second primary tumors after lobectomy by means of video-assistedthoracoscopic surgery (VATS) versus thoracotomy for lung cancer. J Thorac Cardiovasc Surg 2011;141:59-64. [PubMed]
- Paul S, Altorki NK, Sheng S, et al. Thoracoscopic lobectomy is associated with lower morbidity than open lobectomy: a propensity-matched analysis from the STS database. J Thorac Cardiovasc Surg 2010;139:366-78. [PubMed]
- Flores RM, Ihekweazu U, Dycoco J, et al. Video-assisted thoracoscopicsurgery (VATS) lobectomy: catastrophic intraoperative complications. J Thorac Cardiovasc Surg 2011;142:1412-7. [PubMed]
- Kim K, Kim HK, Park JS, et al. Video-assisted thoracic surgery lobectomy: single institutional experience with 704 cases. Ann Thorac Surg 2010;89:S2118-22. [PubMed]
- Scott WJ, Allen MS, Darling G, et al. Video-assisted thoracic surgeryversus open lobectomy for lung cancer: a secondary analysis of data from theAmerican College of Surgeons Oncology Group Z0030 randomized clinical trial. J Thorac Cardiovasc Surg 2010;139:976-81; discussion 981-3. [PubMed]
- Gopaldas RR, Bakaeen FG, Dao TK, et al. Video-assistedthoracoscopic versus open thoracotomy lobectomy in a cohort of 13,619 patients. Ann Thorac Surg 2010;89:1563-70. [PubMed]


