Bronchopulmonary foregut malformation presenting as extralobar pulmonary sequestration associated with a bronchogenic cyst: an unusual clinical and radiological feature in an adolescent patient
Introduction
Bronchopulmonary foregut malformations (BPFMs) include congenital anomalies associated with the development of the foregut, pulmonary, airway, and vascular components (1). Among them, extralobar pulmonary sequestration is known as dysplastic or nonfunctioning lung tissue with its own pleura and without communication with the normal bronchial tree. It is usually located in the left lower hemithorax and receives its blood supply from one or more systemic arteries (2). Bronchogenic cysts originate from an abnormal budding of the tracheobronchial tree and are typically solitary cysts lined with either squamous or ciliated columnar epithelium, which is similar to bronchi (3).
We recently encountered a case of BPFM presenting as extralobar pulmonary sequestration associated with a bronchogenic cyst. The patient had an anterior mediastinal cystic mass and suffered from fever and pleural effusion, a presentation that mimics an infected bronchogenic cyst with perforation. Furthermore, computed tomography (CT) demonstrated the lesion was located in the upper hemithorax and was supplied from the pulmonary artery. We present a case of a complex BPFM consisting of extralobar sequestration associated with a bronchogenic cyst presenting as an unusual clinical and radiological feature.
Case presentation
A 15-year-old boy was admitted to the emergency room for left pleuritic chest pain and fever (38.0 °C) of 1-day duration. The chest radiograph showed a large lobulated mass in the left hilar area that shared a sharp border with the adjacent lung parenchyma. A chest CT scan showed a cystic mass in the left mediastinal area that formed an acute angle with the adjacent parenchyma of the left upper lobe, suggesting an extrapulmonary origin. The mass contained a non-enhanced homogenous low-attenuated fluid component (Figure 1A). There was a scanty amount of pleural fluid in the left hemithorax, suggesting perforation of the cystic mass (Figure 1A). A small artery originating from the left pulmonary artery and entering the medial side of the cystic mass was visualized (Figure 1B). We therefore suggested the presence of a complicated cystic mass, such as a bronchogenic cyst or dermoid cyst, with infection.
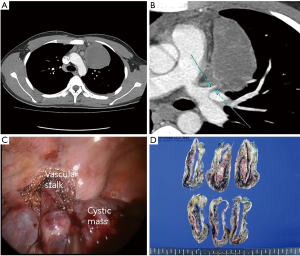
The patient underwent thoracoscopic surgical intervention for lesion resection. During surgery, we found a supernumerary lobe of the left lung, with a vascular hilum, between the upper and lower lobes. This lobe consisted of cystic and solid components with hilar vasculature without perforation. The cystic component, which contained thick mucus-like material, included the hilum, and the solid component, which turned out to be composed of lung tissue, was an inclusion of the cystic mass (Figure 1C). A small feeding vessel originating from the hilum was identified and divided with an endoscopic stapler. Gross pathological examination showed a unilocular cystic mass within the inflamed sequestrated lung (Figure 1D) with a wall showing fibrotic change. Microscopically, a bronchial epithelial lining was seen in the large cyst, and inflamed sequestrated lung tissue covered the cyst. A relatively large muscular artery was present at the hilum of the sequestrated lung. No infectious organisms were present in the culture of pleural fluid. The patient’s postoperative course was uneventful and his symptoms disappeared.
Discussion
BPFMs have been described by numerous classifications and terminologies incorporating a common origin and association. These include congenital anomalies associated with the development of the foregut (bronchogenic cyst, esophageal/neurenteric cyst, tracheoesophageal fistula/diverticula/stenosis), pulmonary [pulmonary agenesis/hypoplasia, congenital lobar emphysema, congenital pulmonary airway malformation (CPAM)], airway (tracheal/bronchial atresia, tracheal bronchus), and vascular (pulmonary sling, alveolar capillary dysplasia) components (1,4,5).
Bronchogenic cysts generally demonstrate an enhanced capsular wall and a homogenous consistency on enhanced CT because they have a bronchial epithelial lining and are filled with mucus (6). In the case of complicated bronchogenic cysts, a thick, contrast-enhanced wall with or without internal high attenuation may be demonstrated (7). According to the patient’s demographics and symptoms, dermoid cyst, necrotic tumor, esophageal duplication cyst, and other congenital cystic lesions can be considered as the differential diagnosis for relatively enhanced, thick walled cystic lesions on CT (8). Furthermore, as collateral neovascularization from an infected lesion can be encountered as a consequence of chronic inflammation (3), we suggested infected bronchogenic cyst as the first impression, despite the presence of a supplying vascular structure.
Among BPFMs, extralobar pulmonary sequestration is composed of non-functioning lung tissue and has its own pleura supplied by a systemic artery (1) (Figure 2A). However, BPFMs can be supplied from the pulmonary artery or pulmonary and systemic arteries in extremely rare cases (2). A few reports have demonstrated that pulmonary sequestrations have been described in conjunction with other lung anomalies such as bronchogenic cysts, bronchial atresia, and CPAM, among others (1,8). According to the reports, extralobar pulmonary sequestrations are usually located within the left lower hemithorax region, with systemic artery supply from the descending aorta or intercostal artery and a coexisting bronchogenic cyst noted adjacent to the sequestrated lung tissue (Figure 2B).

However, in our case of complex BPFM, the radiological and clinical findings were unusual. On CT images, a bronchogenic cyst was encircled by sequestrated lung tissue with independent pleura and was located in the left upper hemithorax, not the lower area. In addition, it was supplied from the pulmonary artery, not the systemic artery (Figure 2C). Pleural effusion was also noted. According to a review of BPFM by Heithoff et al. (4), in older children and adults, presentations with recurrent infections such as pneumonia and pleurisy have been reported, although almost all of the patients are totally asymptomatic. Conversely, in this case, the patient presented with acute-onset pain and fever. Thus, we anticipated a thick capsular wall as the sequelae of infection in the cyst or an abscess in a malformed mass, together with symptoms such as fever and pain as a result of perforation of the cystic lesion.
We have described an unusual case of a complex BPFM consisting of extralobar sequestration associated with a bronchogenic cyst, which mimicked an infected mediastinal bronchogenic cyst with perforation.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Newman B. Congenital bronchopulmonary foregut malformations: concepts and controversies. Pediatr Radiol 2006;36:773-91. [Crossref] [PubMed]
- Karantanas AH. Imaging of pulmonary sequestration. AJR Am J Roentgenol 1990;155:1343. [Crossref] [PubMed]
- Akman C, Kantarci F, Cetinkaya S. Imaging in mediastinitis: a systematic review based on aetiology. Clin Radiol 2004;59:573-85. [Crossref] [PubMed]
- Heithoff KB, Sane SM, Williams HJ, et al. Bronchopulmonary foregut malformations. A unifying etiological concept. AJR Am J Roentgenol 1976;126:46-55. [Crossref] [PubMed]
- Kumar B, Agrawal LD, Sharma SB. Congenital bronchopulmonary malformations: a single-center experience and a review of literature. Ann Thorac Med 2008;3:135-9. [Crossref] [PubMed]
- Ramenofsky ML, Leape LL, McCauley RG. Bronchogenic cyst. J Pediatr Surg 1979;14:219-24. [Crossref] [PubMed]
- McAdams HP, Kirejczyk WM, Rosado-de-Christenson ML, et al. Bronchogenic cyst: imaging features with clinical and histopathologic correlation. Radiology 2000;217:441-6. [Crossref] [PubMed]
- Bratu I, Flageole H, Chen MF, et al. The multiple facets of pulmonary sequestration. J Pediatr Surg 2001;36:784-90. [Crossref] [PubMed]


