Fibrous lung tumor: a peculiar case
Introduction
Solitary fibrous tumor (SFT) is a rare neoplasm which most frequently occurs in the pleura, especially visceral pleura, but it is known that intrapulmonary SFT is extremely rare. After several decades of controversies, now it is generally agreed that it originates from mesenchymal cells of submesothelial tissue of the pleura (1). Most of these tumors project into the pleural cavity in a pedunculated manner from the visceral pleura (1,2). Inward tumor growth into the lung parenchyma from the visceral pleura is infrequent and a pure intrapulmonary SFT without morphologic and histologic attachment to the visceral pleura has been described very rarely.
We report here an extremely rare case of a large size of intrapulmonary SFT.
Case report
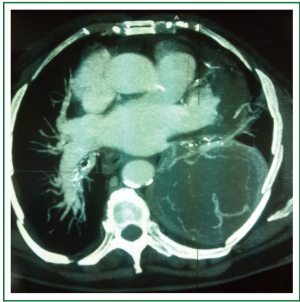
An 81-year-old woman was admitted to hospital for investigations after complaining of left chest pain. She and her family had no specific history and she was no smoker. Patient presented with a chest pain. The chest roentgenogram revealed a nodular shadow within the left lung. A subsequent chest computed tomography (CT) showed a 10 cm × 9 cm, well-circumscribed, intrapulmonary nodular lesion with a large basal pleural connection in the postero-basal and lateral-basal wall of left lung (Figure 1).
There was no mediastinohilar lymphadenopathy or secondary lesions. Other findings were normal.
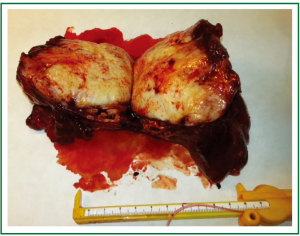
Therefore after diagnostic confirmation of a pulmonary nodule, surgery was performed in the left lung, which was removed by a lobectomy. Through a left inferior lobectomy and ilo-mediastinal lymph node sampling, the entire mass was resected. Histopathological examination revealed a SFT with myxoid aspects, necrotic and hemorrhagic areas (mitosis number ×10; HPF =2; proliferative index evaluated by Ki67 =155).
Immunohistochemically, tumor cells showed an entirely positive reaction to the CD34, Vimentine positive, Bcl positive, CD99 slightly positive, while calretinin, S100, Actine and CKpool were negative. With these morphological and immunohistochemical findings, the final diagnosis was solitary lung fibrous tumor.
The resected tumor was well circumscribed and its dimension was 10 cm × 9 cm (Figure 2). This was surely a peculiar great size for this tumor according with literature.
The postoperative course was uneventful and patient was followed up in outpatient clinic after hospital discharge occurred three days after surgery.
Discussion
SFTs are rare, slow-growing mesenchymal neoplasms thought to originate from submesothelial connective issue (3). They most commonly arise from the parietal and visceral pleura, grow in a nodular and expanding pattern into the pleural cavity, and are often pedunculated.
SFTs are common during the fifth and sixth decades, with no sex predominance. No etiologic agent has been identified; in particular there is no link with smoking or asbestos exposure. Clinically, these tumors are often found incidentally on chest X-rays. CT demonstrates well delineated, noninvasive, non calcified, and highly enhanced masses (2). They are classified as benign or malignant. Normally this tumors have a size not exceeding 3-4 cm in their biggest diameter. Because they lack distinctive histologic features, an immunohistochemical examination is very important for their diagnosis. Immunohistochemically, all the SFTs appear to demonstrate vimentin and CD34 reactivities, and invariable negativity for keratin. In our case CD34 reactivity was found to be positive.
The clinical behavior of the tumor is unpredictable. Intraparenchymal presentation of SFT has been associated with a higher incidence of aggressive or malignant behavior (4). The incidence of aggressive behavior is variously reported as between 13% and 23% of cases in most large series of pleural tumors. The highest risk of recurrence was seen in tumors of pathologically malignant and morphologically sessile types. Chemotherapy and radiotherapy are generally considered ineffective for these tumors; However, Saynak et al. reported a patient with recurrence of SFT, which had a significant response to external thoracic radiotherapy (5). To date there has been no report concerning postsurgical recurrence in published intrapulmonary SFTs, inclusive of the present case. Considering the big size of this tumor, a long-term follow-up of these patients is necessary (1).
In conclusion, a SFT with such big size is extremely rare. Complete surgical resection is the best treatment in SFTs, but further follow-up studies are needed to understand if the bigger size is correlated to a malignant further behavior.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Magdeleinat P, Alifano M, Petino A, et al. Solitary fibrous tumors of the pleura: clinical characteristics, surgical treatment and outcome. Eur J Cardiothorac Surg 2002;21:1087-93. [PubMed]
- de Perrot M, Fischer S, Bründler MA, et al. Solitary fibrous tumors of the pleura. Ann Thorac Surg 2002;74:285-93. [PubMed]
- Cardillo G, Facciolo F, Cavazzana AO, et al. Localized (solitary) fibrous tumors of the pleura: an analysis of 55 patients. Ann Thorac Surg 2000;70:1808-12. [PubMed]
- Aufiero TX, McGary SA, Campbell DB, et al. Intrapulmonary benign fibrous tumor of the pleura. J Thorac Cardiovasc Surg 1995;110:549-51. [PubMed]
- Saynak M, Bayir-Angin G, Kocak Z, et al. Recurrent solitary fibrous tumor of the pleura: significant response to radiotherapy. Med Oncol 2010;27:45-8. [PubMed]