Mediastinal lymph node dissection: the debate is not resolved
In non-small cell lung cancer (NSCLC), metastasis to lymph nodes is one of the most important determinants of prognosis (1,2). Accurate lymph node staging is crucial for selecting therapeutic strategies. Anatomic lung resection with a sampling or systematic mediastinal lymph node dissection (MLND) is the standard treatment of early stage NSCLC (3). Some studies conclude that the lymphatic spread of NSCLC cannot be considered as lobe specific. Therefore, systematic ipsilateral lymphadenectomy is the only option that accurately determines LNs status (4). Other investigators have focused on mediastinal node removal based on nodal spread pathways and have proposed a lobe-specific mediastinal lymph node assessment based on tumor location (5-7). Darling and colleagues (8) pointed out that only 4% of patients were upstaged to pN2 by lymph node dissection in their ACOSOG Z0030 trial which had performed rigorous systematic node sampling prior to randomization.
However the extent of optimal lymph node dissection still remains controversial among thoracic surgeons. In terms of local recurrence and distant metastasis, it is still unclear whether MLND might decrease the incidence of local recurrence and distant metastasis after complete resection for NSCLC. The ACOSOG Z0030 trial did not definitively conclude that MLND affected the probability of local recurrence as well as distant metastasis. Sugi and colleagues (9) demonstrated that there is no statistically significant difference in terms of local recurrence and distant metastasis while comparing MLND and mediastinal lymph node sampling (MLNS) in patients with NSCLC, clinical stage I (<2 cm). It is also important to address the risk of complications in MLND compared to MLNS, where investigators argue against MLND due to risks that prolong hospitalization and increase mortality (10). In other studies that compared the outcomes of patients from MLND and MLNS, researchers did not find any significant statistical difference in complications comparing MLND and MLNS (11). However, MLND is related to increased operative risks such as: increased operative time, blood loss, recurrent laryngeal nerve injury, chylothorax, risk of bronchopleural fistula, large vessel injury, and tracheoesophageal fistula as reported in prior publications (12).
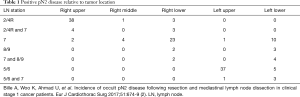
This retrospective study was conducted to evaluate the role of MLND in clinical stage I NSCLC. Bille and colleagues (2), according to their study, found 9% occult pN2 disease after reviewing 1,667 patients with clinical stage I NSCLC after anatomic lung resection with removal of two or more mediastinal lymph node stations. In addition, 16% of patients had unexpected pN2 disease. Of 44 right upper lobe (RUL) cancers with positive mediastinal nodes, 38 positive N2 nodes were identified at station 2/4R (which is the lobe specific pathway) and 2 were found to have metastasized to both stations 2/4R and 7. Only 2 were skip metastasis to level 7.
Out of 474 RUL tumors, only 2 skip metastases were identified with a mediastinal dissection. These would not have been diagnosed if a lobe specific sampling was performed. As a result, patients would not have received adjuvant oncological treatment. Is this worth MLND in the other 472 lesions?
Right lower lobe (RLL) tumors consisted of 452 cases where 28 had occult lymph node metastasis to level 7. Only 3 had metastasized to level 2/4R and 2 to level 8/9 which would have been sampled for a RLL resection. Four hundred left upper lobe (LUL) resections were performed and only 1 skip metastasis to level 7 was identified. Two hundred and eighty-two left lower lobe (LLL) resections with mediastinal dissection were performed and only 5 metastasis to level 5/6 were identified which otherwise would have been missed with lobe-specific sampling. (Table 1).
Full table
In this study, the authors observed an association between nodal status and survival. The 5-year overall survival was 61%, pN2 patients had a 5-year survival of 36% compared to 66% of patients with N0 disease. Other authors have reported similar survival rates for pN2 patients (4,6). However these data do not provide any evidence that MLND is superior to lobe-specific dissection, because only a few skip metastases were found in this study by MLND. This wouldn’t have caused any impact on survival outcome in this large population study (Table 1). It also indicated that 74 (8.3%) and 72 (9.2%) pN2 were discovered when 2 and 3 mediastinal lymph node stations were removed respectively. Thus no significant difference in number of diagnosed pN2 was observed when higher numbers of lymph nodes were removed. In the clinical setting, lobe-specific MLNS is sufficient. We do not believe that the data supports MLND as superior to MLNS in terms of survival and local recurrence. MLND is associated with risk of intraoperative complications and longer hospital stay.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Lardinois D, De Leyn P, Van Schil P, et al. ESTS guidelines for intraoperative lymph node staging in non-small cell lung cancer. Eur J Cardiothorac Surg 2006;30:787-92. [Crossref] [PubMed]
- Bille A, Woo KM, Ahmad U, et al. Incidence of occult pN2 disease following resection and mediastinal lymph node dissection in clinical stage I lung cancer patients. Eur J Cardiothorac Surg 2017;51:674-9. [Crossref] [PubMed]
- Defranchi SA, Cassivi SD, Nichols FC, et al. N2 disease in T1 non-small cell lung cancer. Ann Thorac Surg 2009;88:924-8. [Crossref] [PubMed]
- Riquet M, Rivera C, Pricopi C, et al. Is the lymphatic drainage of lung cancer lobe-specific? A surgical appraisal. Eur J Cardiothorac Surg 2015;47:543-9. [Crossref] [PubMed]
- Shapiro M, Kadakia S, Lim J, et al. Lobe-specific mediastinal nodal dissection is sufficient during lobectomy by video-assisted thoracic surgery or thoracotomy for early-stage lung cancer. Chest 2013;144:1615-21. [Crossref] [PubMed]
- Asamura H, Nakayama H, Kondo H, et al. Lobe-specific extent of systematic lymph node dissection for non-small cell lung carcinomas according to a retrospective study of metastasis and prognosis. J Thorac Cardiovasc Surg 1999;117:1102-11. [Crossref] [PubMed]
- Rusch VW, Crowley J, Giroux DJ, et al. The IASLC Lung Cancer Staging Project: proposals for the revision of the N descriptors in the forthcoming seventh edition of the TNM classification for lung cancer. J Thorac Oncol 2007;2:603-12.
- Darling GE, Allen MS, Decker PA, et al. Randomized trial of mediastinal lymph node sampling versus complete lymphadenectomy during pulmonary resection in the patient with N0 or N1 (less than hilar) non-small cell carcinoma: results of the American College of Surgery Oncology Group Z0030 Trial. J Thorac Cardiovasc Surg 2011;141:662-70. [Crossref] [PubMed]
- Sugi K, Nawata K, Fujita N, et al. Systematic lymph node dissection for clinically diagnosed peripheral non-small-cell lung cancer less than 2 cm in diameter. World J Surg 1998;22:290-4; discussion 294-5. [Crossref] [PubMed]
- Passlick B, Kubuschock B, Sienel W, et al. Mediastinal lymphadenectomy in non-small cell lung cancer: effectiveness in patients with or without nodal micrometastases - results of a preliminary study. Eur J Cardiothorac Surg 2002;21:520-6. [Crossref] [PubMed]
- Huang X, Wang J, Chen Q, et al. Mediastinal lymph node dissection versus mediastinal lymph node sampling for early stage non-small cell lung cancer: a systematic review and meta-analysis. PLoS One 2014;9:e109979. [Crossref] [PubMed]
- Flores RM, Ihekweazu U, Dycoco J, et al. Video-assisted thoracoscopic surgery (VATS) lobectomy: catastrophic intraoperative complications. J Thorac Cardiovasc Surg 2011;142:1412-7. [Crossref] [PubMed]


