Misdiagnosis of anomalous pulmonary venous connections in a patient with lung cancer and a review of the literature
IntroductionOther Section
Anomalous pulmonary venous connections (APVCs) are a group of rare conditions in which one or more of the pulmonary veins are connected to the right atrium or systemic vein. The venous abnormality can be either partial (PAPVCs) or total (TAPVCs). Typically, it causes a left-to-right shunt, with signs and symptoms depending on the extent of the shunt. In patients with hidden asymptomatic PAPVC requiring a major lung resection, the surgical procedure could increase the volume of shunt flow and cause right-sided heart failure (1). Therefore, it is critical to detect and correct this anomaly to prevent heart failure from occurring during the surgery. We present a case of a misdiagnosed PAPVC in a patient who underwent a right pulmonary resection for lung cancer with a previous history of tuberculosis and left lobe resection.
Case presentationOther Section
A 54-year-old woman was admitted to our Institution for a lesion in the right lung. Her medical history included smoking history (10 packs/year), chronic hepatitis type B, gastritis and systemic sclerosis. In 2011, she underwent left upper lobe wedge resection for an indeterminate pulmonary lesion with definitive diagnosis of pulmonary tuberculosis; neither intraoperative nor postoperative complications occurred.
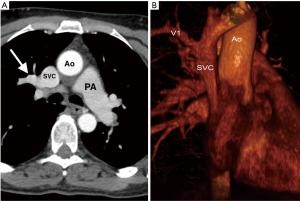
Chest CT scan revealed 1 cm lesion in the right upper lobe (Figure 1). Physical examination showed no specific abnormalities and no lymphadenopathy were found. The levels of cancer embryonic antigen (CEA) and prostate specific antigen (PSA) were normal. Positron emission tomography-computed tomography (CT) using 18F-fluorodeoxyglucose (PET-FDG) showed a nodule with maximum standard uptake value of 7.6. Bronchoscopy was negative and arterial blood gas analysis revealed a PaO2 of 88.5 mmHg and PaCO2 of 39.5 mmHg on room air. Pulmonary function tests were normal. Transthoracic echocardiography was not performed. The patient was scheduled to undergo a wedge surgical resection with intraoperative frozen section analysis followed by upper right lobectomy in case of a diagnosis of non-small cell lung cancer on the frozen specimen. During thoracoscopic examination of the pleural cavity an anomalous pulmonary vein coming out from the right upper lobe and draining into the superior vena cava was found (Figure 2). Intraoperative diagnosis done was non-small cell lung cancer (NSCLC). Therefore, conversion to open thoracotomy was required to allow safe management of the anomalous vein, and right upper lobectomy was performed as definitive treatment for both the lung cancer and the PAPVC.
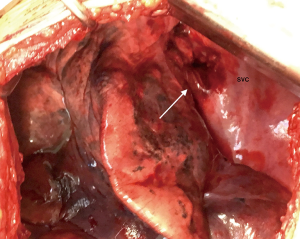
The anomalous right superior pulmonary vein was divided using a vascular stapler. Intraoperatively oxygenation was preserved and no hemodynamic problems occurred during the surgery.
Macroscopically, the resected specimen showed a well circumscribed and confined nodule within the parenchyma measuring 0.8 cm × 0.6 cm × 0.7 cm, no hemorrhage or necrosis were found in the lesion. Histopathological examination of the resected specimen revealed moderately differentiated acinar adenocarcinoma. Furthermore, all mediastinal lymph nodes were free of tumor cells. The pathologic stage of the lung cancer was IA (T1aN0M0). The duration of surgery was 206 minutes and the amount of bleeding was 120 mL. Postoperative course was uneventful. Echocardiography showed normal cardiovascular activity without atrial septal defect. The patient remains in good health 6 months after surgery.
DiscussionOther Section
Partial anomalous pulmonary venous connections (PAPVCs) are a group of rare conditions in which one or more of the pulmonary veins, but not all, are connected to the right atrium or to a systemic vein (1). PAPVCs can be found in only 0.1–0.2% of the adult population using CT scans (2), this prevalence raises to 0.4–0.7% at the time of autopsy (1). The spectrum covers a wide variety of morphological substrates, often associated with other congenital heart diseases (3). Typically, it causes a left-to-right shunt with shunt magnitude depending on the number and position of pulmonary veins draining systemically and on the associated lesions. When symptomatic, it manifests with fatigue, dyspnea, syncope, atrial arrhythmias, right heart failure, and rarely patients develop pulmonary hypertension (4). Dilatation of the right heart chambers, due to volume load, is a characteristic particularly when the Qp/Qs exceeds 2:1 (5). PAPVCs with a small amount of shunt are usually asymptomatic and tend not be found during lifetime. In the present case, the patient had no symptoms and PAPVC was diagnosed intraoperatively, although in retrospect, the enhanced anomalous vein was visible on the preoperative CT but diagnosis was not made at that time. CT and particularly computerized tomography angiography (CTA) allows detection and assessment of the diverse and complex anatomy of APVCs, providing a noninvasive assessment of the three-dimensional anatomy with excellent spatial resolution (6). PAPVCs can be undetected at the initial radiological diagnosis because of the low incidence, often non-symptomatic till later stages, and the lack of knowledge of physicians.
Although echocardiography has a specific role in the diagnosis and classification of APVCs, it lacks the sensitivity and specificity of CTA in detecting and defining the anatomic pathways of PAPVCs (7). In patients with hidden PAPVC requiring a major lung resection, the surgical procedure could increase the volume of shunt flow and cause right-sided heart failure (1). Therefore, it is very critical to detect and correct this anomaly to prevent heart failure from occurring during or after surgery. Approximately, 50% of patients with PAPVCs are diagnosed intraoperatively (8).
If PAPVC is located in the same lobe of the tumor, lobectomy and ligation of the anomalous vein is the definitive treatment for both the PAPVC and tumor. Nevertheless, if PAPVC and the tumor are located in different lobes, correction of the PAPVC based on the extent of pulmonary resection and the Qp/Qs ratio. The correction of PAPVC will prevent increase in the shunt fraction through the PAPVC with the decrease of the overall normal vasculature after lobectomy (1,4,9,10). In this case, lung cancer was located in the right upper lobe unilaterally with the PAPVC. We performed a lobectomy to treat both lung cancer and PAPVC. No haemodynamic problems occurred during and after the surgery. A conversion to open thoracotomy was required to allow safe management of the anomalous vein. Interestingly, our patient had a history of left pulmonary resection and was ventilated through one lung without any intraoperative complications.
This report stresses the critical role of the early and non-invasive detection of asymptomatic PAPVC through pre-operative CT scans. We believe that more cautious approach should be followed when evaluating patients for lung resection to prevent complications during or after surgery.
AcknowledgementsOther Section
None.
FootnoteOther Section
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
ReferencesOther Section
- Black MD, Shamji FM, Goldstein W, et al. Pulmonary resection and contralateral anomalous venous drainage: a lethal combination. Ann Thorac Surg 1992;53:689-91. [Crossref] [PubMed]
- Ho ML, Bhalla S, Bierhals A, et al. MDCT of partial anomalous pulmonary venous return (PAPVR) in adults. J Thorac Imaging 2009;24:89-95. [Crossref] [PubMed]
- Herlong JR, Jaggers JJ, Ungerleider RM. Congenital Heart Surgery Nomenclature and Database Project: pulmonary venous anomalies. Ann Thorac Surg 2000;69:S56-69. [Crossref] [PubMed]
- Tourmousoglou C, Kalogeropoulou C, Koletsis E, et al. Right upper lobe partial anomalous pulmonary venous connection. Case Rep Vasc Med 2014;2014:249896. [Crossref] [PubMed]
- Fragata J, Magalhães M, Baquero L, et al. Partial anomalous pulmonary venous connections: surgical management. World J Pediatr Congenit Heart Surg 2013;4:44-9. [Crossref] [PubMed]
- Dyer KT, Hlavacek AM, Meinel FG, et al. Imaging in congenital pulmonary vein anomalies: the role of computed tomography. Pediatr Radiol 2014;44:1158-68. [Crossref] [PubMed]
- Zhang Z, Zhang L, Xie F, et al. Echocardiographic diagnosis of anomalous pulmonary venous connections: Experience of 84 cases from 1 medical center. Medicine (Baltimore) 2016;95:e5389. [Crossref] [PubMed]
- Kawagoe I, Hayashida M, Nozumi Y, et al. A Combination of a Partial Anomalous Pulmonary Venous Connection (PAPVC) and a Lung Tumor Requiring Pulmonary Resection. J Cardiothorac Vasc Anesth 2017;31:274-8. [Crossref] [PubMed]
- Sakurai H, Kondo H, Sekiguchi A, et al. Left pneumonectomy for lung cancer after correction of contralateral partial anomalous pulmonary venous return. Ann Thorac Surg 2005;79:1778-80. [Crossref] [PubMed]
- Mikubo M, Ikeda S, Hoshino T, et al. Pulmonary resection of lung cancer in a patient with partial anomalous pulmonary venous connection. Ann Thorac Surg 2013;95:1799-801. [Crossref] [PubMed]


