A hamartoma presenting as an intramural upper oesophageal tumour
Introduction
The embryological development of oesophagus and trachea is from the primitive foregut, and is divided by the development of respiratory diverticulum. Hamartomas were introduced in 1904 by Albrecht (1) as tumour-like malformations with mixing normal tissue components in the organ in which they occur. Hamartomas of the lung and airways are relatively common tumours, but only a few reports describe a hamartoma of the oesophagus in adults (2-8). Also, hamartomas of the nasotracheal tract have been presented, and most of them in paediatric population (9,10). These tumours are mainly composed of cartilage, fat, fibrous tissue, and bone. The chief complaint of these patients is progressive dysphagia and possible weight loss.
We present a case where the preoperative assessment with imaging and endoscopy could not exactly predict the final most probable histological alternative. Therefore, the patient was prepared and consented for a major oesophageal resection and reconstruction, but was perioperatively diagnosed with an intramural upper oesophageal neoplasm, which could be resected pericapsularly without opening of the oesophageal lumen. The rare histology of this lesion will be discussed.
Case presentation
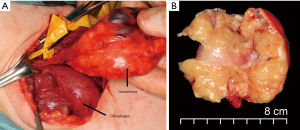
A previously healthy 19-year-old female was referred from a regional hospital in October 2009 with progressive dysphagia and a retrosternal tumour. She did not have significant weight loss. In computed tomography the lesion measured 4.9 cm × 3.5 cm × 9.0 cm (Figure 1). In the imaging, the tumour appeared heterogenic, located above carina, and was submucosal in oesophagus. In order to obtain a biopsy, both bronchoscopy and esophagoscopy were done under general anaesthesia. External compression of the oesophagus was noted between 12 to 25 cm from the incisor line and the mucosa was macroscopically normal. Several fine needle aspirations from the tumour were taken, which were all negative for malignant cells. In an oesophageal ultrasound examination cystic structures were identified, and the tumour appeared benign in nature. Operative treatment was scheduled, but due to patient-related factors, the operation was postponed to September 2010. Operative treatment consisted of a neck incision to approach the oesophagus, which was then encircled and muscular wall was opened vertically keeping the mucosa intact. The tumour was identified between muscle and mucosal layer and a pericapsular enucleation was performed (Figure 2). The patient was discharged on the second postoperative day without any primary complications. On a follow-up visit one month later the patient complained hoarseness and a consultation was appointed at the Department of Otolaryngology-Head and Neck Surgery. Left vocal cord paralysis was noted and scheduled for follow-up. During the first 1-year follow-up, her hoarseness subsided without any intervention and the patient has remained also otherwise symptomless.
Pathologic findings
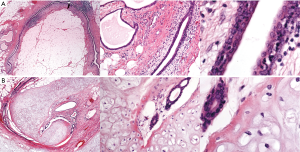
In light microscopy the surgical specimen composed of mature fat tissue, fibrous tissue, cartilage and benign glandular structures (Figure 3).
Discussion
We report on a rare finding of a mediastinal mass that was diagnosed as a large intramural hamartomatous tumour of the proximal oesophagus. The final diagnosis was only evident macroscopically perioperatively and histopathologically after surgical resection of the entire tumour mass. This report adds to the differential diagnosis of slowly growing upper mediastinal tumours. More importantly it demonstrates the importance of preoperative assessment and the value of preparing the patient even for major resections and reconstructions even though the final surgical outcome based on a rare histological alternative may lead to a totally different outcome.
Benign tumours of the oesophagus are rare accounting up to 0.5% or less of all oesophageal tumours at autopsy (11,12). Other types of tumours rise from distal to middle oesophagus, and only fibrovascular polyps tend to dominate in upper oesophagus (12). The most common tumour type is leiomyoma, while other benign tumours are rare, such as neurofibromas (schwannoma), granular cell tumours, hemangiomas, lipomas, and other types of polyps like hamartoma (13). Previous reports have described intraluminal polypomatous descriptions of oesophageal hamartoma or lower intramural oesophageal hamartoma (2,3,5,14) or lower intramural oesophageal hamartoma (4). Hamartoma in cervical oesophagus of adults is extremely rare and only five case reports on this entity have been published this far (2,3,5,8,15).
Benign oesophageal tumours also constitute a rare cause of dysphagia. An incidence of only 15 cases per 11,000 patients has been reported (12). Also, submucosal tumours are often asymptomatic and discovered only after their diameter exceeds 5 cm. The first step at diagnosis is to rule out the possibility of malignancy. The diagnostic tool of choice in the modern era is endoscopic ultrasound (EUS) although barium oesophagogram, contrast-enhanced CT image and conventional gastroscopy are as well key elements in the diagnostic work-up. In our case EUS was not usable because of very proximal location of the tumour in the oesophagus but CT scan revealed cystic nature of the tumour and the tumour appeared benign in nature. In contrast to our finding Zhang et al. have reported usefulness of EUS in the differential diagnosis of cervical oesophageal hamartomas (8).
There are a few reports on successful endoscopic treatments of oesophageal hamartomas (5,16,17). According to Ginai et al. a prerequisite for successful endoscopic ligation of the hamartoma is that it is pediculated (15). This was not the case in our patient. We decided to proceed with surgery similarly to Zhang et al. (8) because the tumour was inside the muscular wall of the cervical oesophagus and there was no safe endoscopic approach available. Also, the cervical location of the tumour was very favourable to surgery. Our patient had an uneventful recovery and did not have any recurrence during a 6-year follow-up.
In our case light microscopy revealed the surgical specimen (Figure 3) composing of mature fat tissue, fibrous tissue, cartilage and benign glandular structures which is a rare form of chondromatous hamartoma as noted by Amstalden and others (18).
Conclusions
We conclude, that diagnosis of these lesions is challenging even with modern diagnostic aids, such as computed tomography, ultrasound esophagoscopy and endoscopic fine-needle aspiration. In contrast, the operative approach and technique are relatively straightforward and will be followed by symptom-relief but may involve large resections with consequent reconstructions. The long-term prognosis of oesophageal hamartomas seems good after surgical treatment (19) and without significant concern for residual tumour growth. Although hamartoma is a very rare entity it is worth remembering in the differential diagnosis of submucosal cervical tumour in the oesophagus.
Acknowledgements
The authors thank Yvonne Sundström for skilful secretarial assistance.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Albrecht E. Ueber hamartome. Verhandlungen der Deutschen Gesellschaft für Pathologie 1904;7:153-7.
- Shah B, Unger L, Heimlich HJ. Hamartomatous polyp of the oesophagus. Arch Surg 1975;110:326-8. [Crossref] [PubMed]
- Saitoh Y, Inomata Y, Tadaki N, et al. Pedunculated intraluminal osteochrondromatous hamartoma of the oesophagus. J Otolaryngol 1990;19:339-42. [PubMed]
- Venn GE, DaCosta P, Goldstraw P. Giant oesophageal hamartoma. Thorax 1985;40:684-5. [Crossref] [PubMed]
- Halfhide BC, Ginai AZ, Spoelstra HA, et al. Case report: a hamartoma presenting as a giant oesophageal polyp. Br J Radiol 1995;68:85-8. [Crossref] [PubMed]
- Everett C, Volberg F, Ulshen M, et al. Intramural esophageal hamartoma: a report of two cases and review of the literature. Gastrointest Radiol 1980;5:317-9. [Crossref] [PubMed]
- Hou SP, Zhang QQ, Wang LN, et al. Chondroma-like hamartoma of esophagus: report of a case. Zhonghua Bing Li Xue Za Zhi 2012;41:274-5. [PubMed]
- Zhang C, Xu J, Wang Z, et al. Chondromatous hamartoma of cervical esophagus: a case report and literature review. J Thorac Dis 2017;9:E236-E244. [Crossref] [PubMed]
- Park SK. Mesenchymal hamartoma in nasopharynx: a case report. Auris Nasus Larynx 2008;35:437-9. [Crossref] [PubMed]
- Mäkitie AA. Hamartoma of the larynx: an unusual cause of dyspnea. Ann Otol Rhinol Laryngol 2003;112:841-3. [Crossref] [PubMed]
- Attah EB, Hajdu SI. Benign and malignant tumors of the esophagus at autopsy. J Thorac Cardiovasc Surg 1968;55:396-404. [PubMed]
- Choong CK, Meyers BF. Benign esophageal tumors: introduction, incidence, classification, and clinical features. Semin Thorac Cardiovasc Surg 2003;15:3-8. [Crossref] [PubMed]
- Heitmiller FR, Brock VM. Benign Tumours and Cysts of the Oesophagus. In: Yeo CJ, Mcfadden DW, Pemberton JH, et al. editors. Shackelford’s Surgery of the Alimentary Tract. 7th ed. Philadelphia: Elsevier, 2013:180-94.
- Caceres M, Steeb G, Wilks SM, et al. Large pedunculated polyps originating in the oesophagus and hypopharynx. Ann Thorac Surg 2006;81:393-6. [Crossref] [PubMed]
- Ginai AZ, Halfhide BC, Dees J, et al. Giant esophageal polyp: a clinical and radiological entity with variable histology. Eur Radiol 1998;8:264-9. [Crossref] [PubMed]
- Xu GQ, Hu FL, Chen LH, et al. The value of endoscopic ultrasonography on diagnosis and treatment of esophageal hamartoma. J Zhejiang Univ Sci B 2008;9:662-6. [Crossref] [PubMed]
- Coury J, Steinfeld J, Zwillenberg D, et al. Oesophageal hamartoma as an unusual cause of neonatal apnea and bradycardia. Ear Nose Throat J 2010;89:E7-E11. [PubMed]
- Amstalden EM, Carvalho RB, Pacheco EM, et al. Chondromatous hamartoma of the chest wall: description of 3 new cases and literature review. Int J Surg Pathol 2006;14:119-26. [Crossref] [PubMed]
- Smith CW, Murray GF, Wilcox BR. Intramural oesophageal hamartoma. An unusual cause of progressive stricture in a child. J Thorac Cardiovasc Surg 1976;72:315-8. [PubMed]



