Lung allocation
Introduction
Currently, approximately 3,500 transplants are performed worldwide annually (1). Eligible patients are put on the waiting list at their local transplant centre. Unfortunately, a shortage of donor organs leads to considerable numbers of patients dying on the waiting list for lung transplantation (LTx) before suitable organs become available. Lung transplantation is nowadays an accepted therapy for end-stage thoracic disease, but major problems remain to be addressed. Transplantation is has a costly and risky therapy. Demand for donor lungs exceeds the supply by far. The discrepancy between supply of organs and demand for them as life-saving therapies has resulted in scrutiny of organ distribution policies, and raises ethical questions. In designing an allocation algorithm, a number of ethical principles should be considered including the four basic ethical principles:
- Patient autonomy: a patient has the right to choose/refuse treatment;
- Beneficence: practitioner should act in the best interest of the patient;
- Non-maleficence: an obligation to not intentionally inflict harm to the patient;
- Justice: concerns the distribution of scarce health resources (“Who gets what?”).
Efficient donor organ allocation remains crucial in optimizing donor use, to reduce waitlist mortality and to improve transplant outcomes.
In some countries, there is national wait list and some countries are organized in supranational allocation systems (e.g., Eurotransplant). Available donor lungs will be assigned according to predetermined criteria. Usually lungs are matched by size (total lung capacity) and blood type in first order. In case of several suitable candidates for a given organ offer, organs are distributed according further pre-specified rules. The entire process of organ distribution is called “organ allocation”.
Allocation criteria after blood type and size matching may be based on clinical judgment (so called center decision), urgency (e.g., by audit process, individual decision, or objectively by a score system), or on waiting time, or a combination of several of these criteria. Currently, rules guiding allocation in most countries are based on urgency and transplant benefit, with survival benefit being the accepted primary goal. The ideal time for the transplant is not easy to determine and depends on the individual course of the underlying illness. Many pulmonary diseases experience a relatively slowly progressive course while other will develop a sudden acceleration with rapid deterioration of the patient’s condition. Within a system of waiting time based allocation only up to 30% of patients will die before an organ becomes available (2). Installation of an urgency status will decrease mortality of critically ill candidates unless the proportion of patients on urgency status will be too high (3).
Most people agree that top priority should be given to patients with the least amount of time to live (‘Rule of Rescue’) and outcome is rated second by the majority. Existing registry data are often used to assist individual assessment of urgency and transplant benefit in conjunction with clinical judgment. Historically, lung allocation, in the US and in the Eurotransplant region, was mainly based on waiting time. In some European countries there is a national urgency list (France, Switzerland) and some European countries allocate donor lungs according center decision (UK). More than 60% of the worldwide lung transplant activity is allocated by the lung allocation score (LAS). Waiting time-based lung allocation and center-based allocation has been reported to be associated with high wait list mortality (2,4).
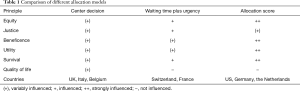
The pros and cons of the three most commonly used allocation models (center decision, waiting time plus urgency and an allocation score) are displayed in Table 1.
Full table
The LAS
The LAS is a numerical value used to assign relative priority in distributing donated lungs. The LAS evaluates several parameters of patient health to direct organ donation toward patients obtaining greatest benefit from lung transplantation (5).
More than a decade ago, the US Department of Health and Human Services issued the “Final Rule”, intended to ensure that organs were allocated “based on medical criteria, not accidents of geography”. In 1998, the Department of Health and Human Services of the US suggested that waiting time-based allocation should be replaced by medical urgency in the absence of unsuccessful transplants. Urgency was classified as more important than the prospect of success. A working group was set up to develop a corresponding system for lung allocation. Essential ethical aspects in the development were equality of all patients (blood group, ethnicity), justice (each patient is judged strictly according to objective criteria), benefit (principle: the benefit must outweigh the potential damage), and usefulness (benefit of a scarce resource).
To develop a statistical model, 3,104 American Lung Transplant-data recorded in the US Register OPTN were analysed from candidates of the years 1997 and 1998. Eighty percent of all listings were made according to four diagnostic groups [lung emphysema/chronic obstructive lung disease (COPD) including alpha1-antitrypsin deficiency (n=1,461), cystic fibrosis (n=708), idiopathic pulmonary fibrosis (n=608) and idiopathic pulmonary arterial hypertension (n=327)].
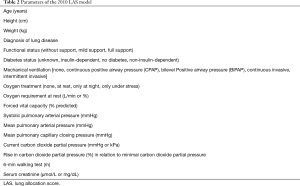
Because of the relatively small number of patients with idiopathic pulmonary arterial hypertension, this group was enriched by patients from the years 1995 and 1996 so that in the end, 636 of these patients were available for evaluation. Approximately 30 parameters of lung transplant candidates were recorded in the US at that time on the wait list. These included age, height, weight, body mass index (BMI), pulmonary arterial pressure (PAP), cardiac index (CI), pulmonary capillary wedge pressure (PCWP), forced vital capacity (FVC), forced expiratory volume in 1 second (FEV1), functional status, etc.
In the four diagnosis groups mentioned above, multivariate Cox analysis was carried out, which resulted in disease-specific factors which had a significant influence on the wait list mortality.
The remaining 20% of the patients who were initially not covered by these groups were assigned to the four main groups on the basis of clinically similar symptoms and courses. This assignment was statistically verified by comparing the survival of the respective patients with the calculated survival of the group.
In addition, the results were adjusted by combining the parameters of all four groups into a total model. These factors were confirmed in their prognostic statement by separate analysis of the four disease categories. With the overall analysis of all patients, both the probable survival within a year on the wait list, as well as the 1-year survival after lung transplantation could be calculated using biometric and clinical data. Similarly, prognostic factors for 1-year survival after transplantation had been calculated in a multivariate regressive Cox analysis. The restriction to 1 year was made, since after this time the influence of factors, which determines the immediate success of transplantation, hardly could have any effect on the result.
The models for survival after lung transplantation and wait list survival probability were combined to form a model in which the actual benefit of the transplant was calculated as the difference between transplant survival and wait list survival. Double weighing of wait list survival corresponded to the original intention to take the urgency more into consideration than the success prospect. The LAS takes into account the estimated survival benefit offered by LTx by 1 year after surgery and medical urgency. Parameters included in the model are displayed in Table 2. LAS can be appointed a value between 0 and 100 and according to this model rates the estimated survival advantage by LTx to 1 year. The aim of the system is to direct organs to recipients who are predicted to have the greatest potential transplantation survival benefit.
Full table
The LAS system was introduced in the US in May 2005 and has also been adopted in Germany in December 2011 for LTx candidates age 12 and older and in the Netherlands in April 2014. In the years following implementation in the US and Germany, numerous mainly favourable reports regarding effects on waiting list outflow, transplant activity and outcomes have been published. In the US and Germany constant reduction of mortality on the wait list was observed translated to approximately 8 lives saved on the waiting lists per 100 lung transplants performed (3,6).
Since its introduction as a tool for donor lung allocation in the US in 2005, the number of LTx for US CF patients has increased by 25%. Of note, 70% of wait-listed CF patients were transplanted after a waiting period of 1 year decreasing the 1-year waiting-list mortality from 15% to 10% (7).
Pulmonary hypertension accounts for approximately 5% of all lung transplant activity, with improvements in medical therapy leading to global declines in waiting list registrations and transplant activity. Existing US data on LAS performance for PH patients have revealed somewhat conflicting findings (8,9). Initial reports failed to demonstrate improved waiting list mortality among candidates with pulmonary hypertension, however, more recent analysis involving larger cohorts have contested this. The German data, whilst also limited by small sample size supports this latter report, showing clear reductions in waiting list mortality (3). Composition of transplant recipients changed, with fewer patients with obstructive lung diseases (e.g., COPD) and more recipients with restrictive lung diseases (e.g., idiopathic pulmonary fibrosis). Transplantation under invasive mechanical respiratory support increased in Germany from 9% to 13% (3).
In February 2015 a new LAS model was introduced in the US after the Thoracic Organ Transplantation Committee proposed a revision to the LAS system. This revision includes modifications to the covariates in the waiting list and post-transplant survival models, coefficients of the covariates, and baseline waiting list and post-transplant survival rates used in the LAS calculation. New parameters like increase in creatinine and bilirubine, central venous pressure (CVP), CI (if less than 2 L/min/m2), 6-min-walk distance (if it is less than 1,200 feet), oxygen needed at rest were included in the 2015 LAS model, while others were abandoned. Results of performance of the new model are not yet published. Germany has decided to continue with the 2010 model in 2017.
The LAS can be computed online (2010 model: http://www.eurotransplant.org/cms/index.php?page=las_calculator and 2015 model: https://optn.transplant.hrsa.gov/resources/allocation-calculators/las-calculator/). In the US, organ distribution is made locally first, while in Germany distribution is nationally in first step.
Broader geographic sharing may increase travel costs and ischemic time, but a more appropriate recipient might be identified closer to the donor in a neighboring donor service area. It could be demonstrated recently that 53% of the lungs in the US were transplanted locally (within 58 donor service areas). For each local allocation, a median of 6 recipients in a larger region (nationwide there are 11 regions) had higher LAS values in this retrospective analysis (10). There are practical limitations to transportation of donor lungs because increasing ischemic time and graft dysfunction is related to increasing donor age. Any lung organ distribution system needs to take into account the large size of this country, and a ‘national´ list is probably impractical for large countries.
The transplantation center is responsible for the correct procurement and regular update of LAS (usually in intervals of 3 months, in critical patients every 2 weeks). It should be noted that LAS is not a suitable tool for identifying candidates. This must be performed via individual patient assessment by the transplant team.
No allocation system can eliminate death on the waiting list. Therefore distribution of donor lungs as a precious resource should be made wisely and fairly.
Acknowledgements
None.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Yusen RD, Edwards LB, Kucheryavaya AY, et al. The Registry of the International Society for Heart and Lung Transplantation: Thirty-second Official Adult Lung and Heart-Lung Transplantation Report--2015; Focus Theme: Early Graft Failure. J Heart Lung Transplant 2015;34:1264-77. [Crossref] [PubMed]
- De Meester J, Smits JM, Persijn GG, et al. Listing for lung transplantation: life expectancy and transplant effect, stratified by type of end-stage lung disease, the Eurotransplant experience. J Heart Lung Transplant 2001;20:518-24. [Crossref] [PubMed]
- Gottlieb J, Smits J, Schramm R, et al. Lung Transplantation in Germany Since the Introduction of the Lung Allocation Score. Dtsch Arztebl Int 2017;114:179-85. [PubMed]
- Mackay LS, Anderson RL, Parry G, et al. Pulmonary fibrosis: rate of disease progression as a trigger for referral for lung transplantation. Thorax 2007;62:1069-73. [Crossref] [PubMed]
- Egan TM, Murray S, Bustami RT, et al. Development of the new lung allocation system in the United States. Am J Transplant 2006;6:1212-27. [Crossref] [PubMed]
- Egan TM, Edwards LB. Effect of the lung allocation score on lung transplantation in the United States. J Heart Lung Transplant 2016;35:433-9. [Crossref] [PubMed]
- Thabut G, Christie JD, Mal H, et al. Survival benefit of lung transplant for cystic fibrosis since lung allocation score implementation. Am J Respir Crit Care Med 2013;187:1335-40. [Crossref] [PubMed]
- Chen H, Shiboski SC, Golden JA, et al. Impact of the lung allocation score on lung transplantation for pulmonary arterial hypertension. Am J Respir Crit Care Med 2009;180:468-74. [Crossref] [PubMed]
- Schaffer JM, Singh SK, Joyce DL, et al. Transplantation for idiopathic pulmonary arterial hypertension: improvement in the lung allocation score era. Circulation 2013;127:2503-13. [Crossref] [PubMed]
- Russo MJ, Meltzer D, Merlo A, et al. Local allocation of lung donors results in transplanting lungs in lower priority transplant recipients. Ann Thorac Surg 2013;95:1231-4; discussion 1234-5. [Crossref] [PubMed]


