Single-stage surgery experience in a case of coarctation of the aorta with an arch aneurysm combined with severe coronary artery disease
Introduction
Coarctation of the aorta (COA) is a congenital heart disease that usually treated in infancy (1). Because of its long-term tolerance, COA in adults is associated with a high level of collateral circulation and vascular variation. Here, we report a rare case of COA with an arch aneurysm combined with severe coronary artery disease; in this case, single-stage surgical correction produced satisfactory outcomes.
Case presentation
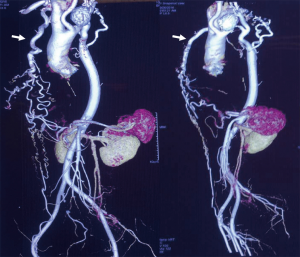
This case involved a 61-year-old female patient with chest tightness, wheezing, and coughing with white, foamy sputum who was categorized as NYHA class IV. She had a prior history of hypertension. Echocardiography showed normal LVEF with mild aortic and mitral valve regurgitation. Computed tomography angiography (CTA) and 3D CT scan reconstruction revealed COA with an arch aneurysm. The aneurysm was between the left subclavian and carotid arteries and had severe peripheral calcification. A small collateral vessel derived from left subclavian artery connected with the arch aneurysm. A thickened right mammary artery was accompanied with collateral circulation (Figure 1). Carotid CTA indicated local occlusion of the left carotid artery. Coronary angiography revealed >90% stenosis in the left anterior descending (LAD) artery, left circumflex artery (LCX), posterolateral artery (PLA), and posterior descending artery (PDA) openings.
Operative technique
We performed ascending-to-descending aortic bypass, COA and aneurysm ligation, and coronary artery bypass grafting (CABG). The surgical approach involved a median sternotomy. Cardiopulmonary bypass was established using the right femoral artery, the aorta, and the superior and inferior vena cavae. A longitudinal posterior pericardial incision over the descending aorta allowed for exposure of the anastomotic stoma. An occluding vascular clamp was used to control the descending aorta, and end-to-side anastomosis of a 20 mm Dacron graft to the descending aorta by a continuous 5-0 polypropylene suture. The graft was located posterior to the inferior vena cava but inferior to the superior vena cava and curved around the right atrium. During graft suturing deep hypothermic circulatory arrest (20 °C) is used and antegrade cerebral perfusion was administered for brain protection. A side wall clamp was used for the ascending aorta anastomosis. The COA and aneurysm were ligated and sutured with 4-0 polypropylene. CABG was performed with the saphenous vein (Figure 2A). The operation time was 640 min, the CPB time was 287 min, and the cross-clamp time was 212 min.
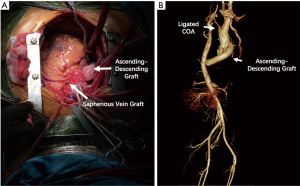
The patient was extubated 6 h after the operation, and discharged on day 12. 3D CT scan reconstruction revealed a stable hemodynamic situation (Figure 2B). A 6-month follow-up indicated great quality of life with NYHA class II status.
Discussion
Intervention or open surgery
Most COA patients are treated in infancy and/or childhood or die during childhood without treatment. The majority of COA patients who survive to adulthood suffer from rich compensatory collateral circulation accompanied by vascular malformations. Surgical difficulties are likely for elderly patients with COA and other cardiovascular diseases due to such malformations. Currently, the preferred treatment for adult COA is thoracic endovascular aortic repair (TEVAR) (2,3). However, in this case, a median sternotomy was necessary due to CABG; therefore, the superiority of minimally invasive intervention was rendered moot. Moreover, because of the relative positions of COA and the aneurysm, an arch covered-stent graft would likely have occluded the left subclavian artery. The patient had dysplastic right vertebral and left internal carotid arteries, and her brain was dependent on blood supply from the thickened left vertebral artery. Occlusion of the left subclavian artery would have resulted in a high risk of insufficiency of blood supply to the brain, which might have required a neck-axillary bypass. Therefore, we did not consider minimally invasive treatment in this case.
Single- or multiple-stage surgery
Two-stage surgery would also have been a feasible approach. In such surgery, CABG would have been performed via median sternotomy, and correction of the aneurysm and COA would have been completed via a left postero-lateral thoracotomy incision 6 weeks later (4). However, with the development of deep hypothermic circulatory arrest techniques, single-stage surgery has become the first choice for patients with COA and concomitant cardiovascular diseases (5,6). Due to the difficulties to expose the descending aorta via a median sternotomy, single-stage surgery is more challenging and requires advanced surgical techniques.
Anatomical or non-anatomical correction
Anatomical corrections of COA include end-to-end anastomosis, patch aortoplasty, arch replacement with a frozen elephant trunk and stent implantation, among other procedures (1). Non-anatomical corrections mainly involve an ascending-descending or ascending-abdominal aorta graft. Technically, the abdominal aorta is much easier to expose; however, the abdominal-thoracic incision may lead to unsatisfactory postoperative recovery. In this case, CT findings revealed an aneurysm with solid calcification that was extremely unlikely to rupture. On the other hand, the aneurysm and COA were rather deep in the thoracic region for anatomical correction. Thus, we chose to use non-anatomical correction to reduce the hemodynamic impact of COA. We ligated on both sides of the aneurysm to occlude its main blood supply, creating dead space with thrombosis organization that could no longer affect the patient’s hemodynamics.
Intraoperative attention points
We also needed to devote attention to avoiding all possible dangerous intraoperative situations. First, once anastomosis is complete, re-exposure for anastomotic bleeding would be much more challenging. Thus, high-quality surgical anastomosis is required. Second, surgeons should prevent the distortion, traction, or oppression of important tissues surrounding the graft. Third, COA patients suffer from prolonged periods of high cardiac afterload and hypertrophy. After the completion of an ascending-descending aorta graft, the resulting sharp decrease in afterload may lead to unstable hemodynamics (7). Epinephrine and norepinephrine should be used to maintain blood pressure.
In conclusion, for such patients with deep COA position combined with other cardiovascular disease and complex vascular anatomy, one-stage, non-anatomical correction surgery is a feasible and effective approach.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
References
- Taggart NW, Minahan M, Cabalka AK, et al. Immediate Outcomes of Covered Stent Placement for Treatment or Prevention of Aortic Wall Injury Associated With Coarctation of the Aorta (COAST II). JACC Cardiovasc Interv 2016;9:484-93. [Crossref] [PubMed]
- Kpodonu J, Ramaiah VG, Rodriguez-Lopez JA, et al. Endovascular management of recurrent adult coarctation of the aorta. Ann Thorac Surg 2010;90:1716-20. [Crossref] [PubMed]
- Li Q, Lin K, Gan CP, et al. One-Stage Hybrid Procedure to Treat Aortic Coarctation Complicated by Intracardiac Anomalies in Two Adults. Ann Thorac Surg 2015;100:2364-7. [Crossref] [PubMed]
- Connolly HM, Schaff HV, Izhar U, et al. Posterior pericardial ascending-to-descending aortic bypass: an alternative surgical approach for complex coarctation of the aorta. Circulation 2001;104:I133-7. [Crossref] [PubMed]
- Ulas MM, Ergun K, Lafci G, et al. Single-stage repair of adult aortic coarctation and concomitant coronary artery disease: an unusual surgical approach through median sternotomy. Cardiovasc J Afr 2012;23:e10-2. [Crossref] [PubMed]
- Yilmaz M, Polat B, Saba D. Single-stage repair of adult aortic coarctation and concomitant cardiovascular pathologies: a new alternative surgical approach. J Cardiothorac Surg 2006;1:18. [Crossref] [PubMed]
- Pethig K, Wahlers T, Tager S, et al. Perioperative complications in combined aortic valve replacement and extraanatomic ascending-descending bypass. Ann Thorac Surg 1996;61:1724-6. [Crossref] [PubMed]


