Systemic tunnel dissection of mediastinal lymph nodes without clamping via uniportal video-assisted thoracoscopic surgery
Introduction
The standard treatment for patients with early-stage non-small-cell lung cancer (NSCLC) is lobectomy or pneumonectomy with systematic nodal dissection (SND). Efficient systemic mediastinal lymph nodes dissection is crucial to the success of surgery and prognosis of patients (1,2) (Figure 1).
Here we describe a tunnel approach to dissect mediastinal lymph nodes without clamping, including subcarinal lymph node (station 7), right paratracheal lymph node (station 2R, 4R) from and A-P window, para-aortic lymph node (station 5, 6).
Operative techniques
A-P window and para-aortic lymph nodes
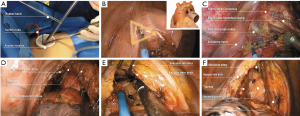
Here we assumed a triangle tunnel around the superior hilar anatomic structure, ascending aorta as one side, descending aorta as the second one and the left pulmonary trunk as the third side (Figure 2A,B). Firstly, dissected the middle mediastinal pleural cling to the superior edge of left pulmonary trunk. Then kept dissociating the pleural along with the first two sides mentioned above and finally converged on the aortic arch. During dissociation, utilized suction to fix the ascending aorta and a tension was developed between suction and hook, which could help to expose. Carefully dissociate the nodes within the triangle region and try to dissect the nodes as a whole bulk. It is important to noted that electrocoagulation need to be powered with less than 30w for reducing related thermal injuries of recurrent laryngeal nerve.
Subcarinal lymph nodes
Firstly, leaned the bed to surgeon until the subcarinal region is vertical to view and the assistant transferred his position behind the surgeon. Next, used suction to pull the remain deflated lung forward, which would tense the posterior mediastinal pleural and help to complete subsequent non-clamping operation. Then the mediastinal pleural over the posterior hilum was incised by electrocoagulation hook to provide exposure to the anatomic structure. Here we defined a manual roof-like tunnel, which include esophagus as one edge and right primary bronchus as another. Based on the supposed edge, further dissection along with the edge was performed. Timely adjust the position of suction and continuous pulling to completely expose the structure with the process of dissociation is very important. And we should keep the hook away from the accessory nerve to avoid thermal injury. During the dissection, exert suction to separate only, without any other instruments to clamp the lymph nodes, which could greatly avoid destroying lymph nodes’ structure. After completely dissociating the two edges of lymph nodes’ region, used suction to bluntly lift the lymph nodes and kept dissociating until we saw the contralateral primary bronchus. One important thing to note is that several nodes in the same station should be dissociated as one bulk together with surrounding adipose and fibrous tissue to the greatest extent (Figure 2C,D).
Right paratracheal lymph nodes
At first, used suction to pull the remain collapsed lung down, which would tense the superior mediastinal. And then pushed the azygos vein upward. Then incised the pleural under the azygos vein and lift the vein by retractor, which established a tunnel underneath the azygos vein. The tunnel allowed us to observe a bulk of tissue including lymph nodes lying on the trachea. Timely adjust the suction and camera to ensure sufficient operative space, which is crucial to the feasibility of non-clamping technique. Utilized electrocoagulation hook only to broaden the interval between adipose tissue surrounding the node along the trachea and superior vena cava underneath the azygos vein (Figure 2E,F).
Comments
Mediastinal lymph nodes should be removed along with surrounding adipose and fibrous tissue and ensure the complete structure of lymph nodes. It inculcates the notion of non-tumor technique. Keep completeness of lymph nodes during dissection is undoubtedly reduce the risk of contact metastasis and local recurrence. The conception of non-clamping, which means use suction electrocautery only during dissection, is exactly meet the non-tumor requirement (4).
Uniportal thoracoscopic surgery of which limitation of operating space is greatly increasing the difficulty of dissection thoroughness. Because of long history of smoking°¢advanced age and suspected lymph node metastasis, the calcification of lymph nodes and tight adhesion are common in lung cancer patients, which greatly increase the difficulty of surgery and the risk of bleeding. By using some physical anatomic structure as landmark to define the regional tunnel for specific station, which emphasizes careful dissection, would help to lower the number of omit lymph nodes and reduce the risk of bleeding. During dissection, timely adjust the position of suction and hook would develop a moderate tension and help to expose, which is crucial to non-clamping technique.
To a certain degree, flexibly use of specific instruments optimized the tunnel dissection procedure. The electrotome designed by Xue-Ning Yang has an obtuse angled hook (145° from the longitude axis) at its apical end. It would greatly increase the flexibility of subtle dissociation from the shallow to deep layer. We utilized the straight suction with four side holes to blunt separate. Moreover, it can keep vision clean via lateral suction.
In summary, based on anatomic landmark of lymph nodes region, establish tunnel dissection without clamping process, could reach the demand of oncology and help to establish the clinical procedure standard of SND.
Acknowledgements
Funding: This work was supported by grants from the National Nature Science Foundation of China (Grant No. 81372285); Guangdong Provincial Key Laboratory of Lung Cancer Translational Medicine (Grant No. 2012A061400006).
Footnote
Conflicts of Interest: Dr. WZ Zhong was awarded “The Master of Thoracic Surgery” and was granted the Award of Best Demonstration in the 2016 Masters of Thoracic Surgery—Uniportal VATS Lobectomy & VATS Segmentectomy Video Contest.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Billè A, Ahmad U, Woo KM, et al. Detection of Recurrence Patterns After Wedge Resection for Early Stage Lung Cancer: Rationale for Radiologic Follow-Up. Ann Thorac Surg 2016;102:1067-73.
- Naruke T, Goya T, Tsuchiya R, et al. The importance of surgery to non-small cell carcinoma of lung with mediastinal lymph node metastasis. Ann Thorac Surg 1988;46:603-10.
- Zhang JT, Dong S, Yang XN, et al. This video describes an alternative technique, systemic tunnel dissection of mediastinal lymph nodes without clamping via uniportal VATS, including station 7, 2R,4R, 5 and 6. Asvide 2017;4:413. Available online: http://www.asvide.com/articles/1726
- Liu C, Pu Q, Guo C, et al. Non-grasping en bloc mediastinal lymph node dissection for video-assisted thoracoscopic lung cancer surgery. BMC Surg 2015;15:38.


