Uniportal video-assisted thoracic surgery lobectomy in a patient with carcinoid tumor located at the orifice of the right lower lobe
Introduction
Bronchopulmonary carcinoid tumors are rare neoplasms that consist of less than 2% of lung malignancies (1). They are relatively low-grade neuroendocrine tumors treated by pulmonary resection and lymph node dissection or sampling (2). In rare occasions in patients with limited lung functions, bronchoscopic removal of the tumor can be performed for palliation of symptoms such as persistent cough, and recurrent pneumonia. Because it originates from the bronchial cells, endobronchial location of the tumor is quite common that makes the video-assisted thoracic surgery (VATS) approach a tricky operation. Main problem in VATS resection is that the tumor in the bronchus might either be stapled during the division of lobar bronchus, which leads the tumor staying in the stump and/or fragmented tumor migrating to the bronchial tree. In order to avoid this, thoracotomy could be preferred over thoracoscopic resection in most cases. In the case VATS is performed in selected patients, stapling of the bronchus well above the endobronchial tumor obviates larger resections such as bilobectomy or even pneumonectomy in regard to the location of the tumor.
An open surgery could be avoided, and uniportal VATS be performed in this relatively low-grade malignancy when the endobronchial tumor is removed first through interventional bronchoscopy. Nevertheless, sticking to oncological principals by performing intraoperative frozen pathological analysis remains essential to achieve a complete resection. We herein present a sequential operation of interventional bronchoscopy followed by uniportal VATS right lower lobectomy in a patient with carcinoid tumor located at the orifice of right lower lobe bronchus.
Case presentation
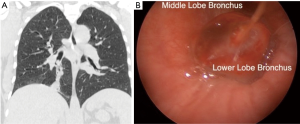
A 47-year old male patient who was diagnosed to have a typical carcinoid tumor located at the orifice of right lower lobe (Figure 1A,B) with bronchoscopic biopsy performed for recurrent pneumonia and persistent cough was referred to our department for surgical treatment. We planned 2-step approach at the same session: (I) interventional bronchoscopy and removal of endobronchial tumor; (II) right lower lobectomy and lymph node dissection with uniportal VATS approach.
Operative techniques (see Figure 2)
Interventional bronchoscopy
Rigid bronchoscopy was performed under general anesthesia. Larynx, trachea the carina and the left bronchial tree were normal. When entered the right bronchial system the tumor was visualized at the orifice of the lower lobe. Tumor that obstructed the lower lobe completely was seen to protrude to the intermediary bronchus allowing only a partial passage into the middle lobe. However, when it was pushed downward with the tip of the bronchoscopic biopsy forceps it was recognized that the origin of the tumor located down in the lower lobe bronchus. Argon plasma cauterization was applied first and followed by removal of endobronchial tumor by bronchoscopic forceps. Intervention was completed when the tumor was removed and the bronchial orifice seen fully open.
Uniportal VATS right lower lobectomy and lymph node dissection
Double lumen endotracheal intubation was performed under general anesthesia. Patient was turned to the left lateral decubitus position and a 3 cm incision was made approximately 3 cm above the imaginary course of the right diaphragm (7th intercostal space) in mid-axillary line. We used no wound retractor/protector. A metallic trocar was placed and its shaft pulled over the camera (30 degrees, 10 mm) inserted. No demarcated neoplastic lesion in the lung was detected in inspection. For the dissection of inferior pulmonary vein, operating table was brought to Trendelenburg position to move the lung upward. Tip of the suction irrigation device and an endoscopic tissue sealer (ENSEAL® G2 Curved, Ethicon) were used for vascular dissection. The vein was stapled with a curved tip stapler (Endo GIA™ 45 mm Curved Tip Articulating Vascular Reload, Medtronic) without hanging it with a silk suture beforehand. Incomplete fissure between the middle and lower lobe was divided by a stapler (Endo GIA™ Universal Roticulator 45–3.5 Loading Unit, Medtronic). Operating table was rotated to backward position to move the lung away for pulmonary artery dissection. Two vascular staplers (Endo GIA™ 45 mm Curved Tip Articulating Vascular Reload, Medtronic) were used to divide individually the common basilar and superior segmental arterial branches of the lower lobe. The lower lobe bronchus was then stapled (Endo GIA™ 60mm Articulating Medium/Thick Reload with Tri-Staple Technology, Medtronic) in proximal part as possible. The lobe was freed completely by stapling of the incomplete fissure between the upper and lower lobes. Then, the lobe was taken into an endo-bag (15 mL) and taken out from the incision, which was enlarged to 5cm to ease the removal of the lobe.
Frozen pathological analysis of the bronchial surgical margin revealed no malignancy in bronchial margin. Mediastinal lymph node sampling including the stations upper and lower paratracheal, subcarinal and inferior ligament was performed. After coagulation, thoracic cavity was irrigated by saline solution, and a 28F chest tube was placed from the incision.
Rigid bronchoscopy was performed when the patient was still on operating table and punch biopsy was taken from the bronchus just above the bronchial stump for frozen pathological analysis, which showed no malignancy. He was taken to intensive care unit for one-night stay. His chest tube was removed on postoperative day 3 and discharged from the hospital one postoperative day 4 after an uneventful postoperative period.
Discussion
Typical carcinoid tumor is the low-grade subgroup of neuroendocrine tumors of the lung (1,2). Curative treatment of the disease is lung resection that provides high rate of survival (1). Although excision of the endobronchial tumor palliates the symptoms such as recurrent pneumonia and persistent cough, it remains an option only in patients who cannot tolerate lung resection.
Because it arises from the neuroendocrine cells of the bronchial epithelium, an endobronchial tumor in the bronchial orifice is seen in most cases. In order to avoid leaving some part of the tumor in the bronchial stump, removal of the endobronchial tumor first remains essential before stapling or dividing and suturing the bronchus. To be able to achieve this, thoracotomy is generally preferred over VATS in patients with endobronchial tumor for its technical feasibility to manage the bronchus. Because stapling the bronchus above the tumor is necessary, VATS approach could only be associated with larger resection of the lung when the tumor locates in the proximal part of the bronchus. As in our patient we presented here (where the tumor protrudes from the right lower lobe bronchus to intermediary bronchus), only a lower bilobectomy could achieve a complete resection in the case VATS is performed. Nevertheless, it is known that the above point of the tumor seen on bronchoscopy is not always the point where the tumor originates; the base of the carcinoid tumor may locate well below in the bronchus. Keeping this feature of the tumor in mind, removal of the endobronchial tumor by interventional bronchoscopy can be considered before the option of VATS approach is abandoned fully in this low-grade malignancy. Yet, oncological principals are always the first to consider in deciding “an invasive or less invasive approach”. Therefore, close collaboration with pathology laboratory that performs frozen analyses throughout surgery remains essential to achieve a complete resection by histologically proven evidences.
In standard uniportal VATS lung resections 5th intercostal space in anterior axillary line is selected (4,5). However, we place the incision in lower part on the 7th intercostal space in midaxillary line; just above the diaphragm, for almost all cases for uniportal VATS lobectomy, segmentectomy or pneumonectomy. This entry site could be enlarged as thoracotomy incision or used for chest tube insertion whenever a conversion to thoracotomy is needed. Additionally, a lower entry site that permits working in caudocranial plane allows also (I) the division of pulmonary vein first, which is important in surgical oncological principals, (II) using the instruments in longer distance with larger angles, and (III) inserting the chest tube as low as possible for better postoperative drainage at the end of the operation. Because of this position of the access incision, the primary surgeon locates at the “anterior and foot site”, where the assistant locates at the head site of the patient.
Our experience showed that using plastic wound retractor/protector was associated with the limitation of instruments moving in larger angels. For this reason, we prefer the naked incision in uniportal VATS approach.
Because the area of entrance into the thorax is limited, the operation becomes more comfortable when fewer instruments are inserted. Capability of the operating table to maneuver in different directions should be used at this point to facilitate in taking out the lung out of vision. Rotation of the operating table in different directions can take the role of pulling out the lung by a grasper inserted through another port in multi-port VATS. Even only a bit move of the lung out of surgical view makes the dissection of bronchovascular structures and the lymph node sampling much easier.
Before development of curved-tip staplers we had to circle and hang the vessels with a silk suture to be able to insert the stapler under the artery or vein. Curved tip stapler shortened the operative time by obviating the need of hanging on the vessel before inserting it.
In conclusion, uniportal VATS lobectomy following removal of the endobronchial tumor by interventional bronchoscopy can be a viable alternative in a patient with centrally located typical carcinoid tumor. Yet, frozen pathological analysis throughout surgery remains an essential part of operation to avoid the recurrence.
Pitfalls
- Advantages of lower entry (port) incision: this allows (i) working in caudocranial plane permitting the division of pulmonary vein first which is one of the rules of surgical oncological principals. [In contrast, the artery is divided first in standard upper-entry uniportal VATS lobectomy to be able to visualize the vein (4)], (ii) maneuvering the instruments in larger angels thanks to longer distance between the entry site and the target area, (iii) draining the pleural cavity more efficiently with the placement of the chest tube at the 7th intercostal space when compared to the chest tube inserted through the 5th intercostal space in anterior axillary line in classical uniportal VATS lobectomy.
- Location of the primary surgeon: because the incision is in the lower chest, surgery is achieved in the caudocranial plane. For this reason, surgeon locates in the anterior and inferior (foot site) but not in the superior (head site) of the patient as in standard uniportal VATS.
- Naked incision: using a wound retractor/protector can be better in looking inside the chest directly from the large hole created by this tool and less injury to the intercostal nerve. However, the soft edge of the skin incision allows the movement of the instruments in larger angels when compared to inflexible edges created by the plastic wound protector.
- Rotating the operating table: limited access area in uniportal VATS lobectomy obliges inserting fewer instruments through the incision for a comfortable operation. Instead of pulling the lung by a grasper inserted through the incision for better visualization, the capability of operating table to rotate in different directions can be used to move the lung from the working area:
- Trendelenburg (head down) position for the dissection of inferior pulmonary vein, and pulmonary ligament lymph node dissection;
- Reverse Trendelenburg (head up) and backward position for paratracheal lymph node dissection;
- Backward position for arterial dissection;
- Forward position for subcarinal lymph node dissection.
- Curved tip stapler: this tool saves time by allowing turning the vessel without hanging it with a silk suture beforehand.
Acknowledgements
Dr. S Halezeroğlu was awarded “The Master of Thoracic Surgery” and was granted the Award of Great Potential in the 2016 Masters of Thoracic Surgery—Uniportal VATS Lobectomy & VATS Segmentectomy Video Contest.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Modlin IM, Lye KD, Kidd M. A 5-decade analysis of 13,715 carcinoid tumors. Cancer 2003;97:934-59. [Crossref] [PubMed]
- Detterbeck FC. Management of carcinoid tumors. Ann Thorac Surg 2010;89:998-1005. [Crossref] [PubMed]
- Halezeroğlu S. Bronchoscopic removal of endobronchial tumor and uniportal VATS right lower lobectomy for carcinoid tumor located at the orifice of right lower lobe. Asvide 2017;4:418. Available online: http://www.asvide.com/articles/1732
- Gonzalez-Rivas D, Fieira E, Delgado M, et al. Uniportal video-assisted thoracoscopic lobectomy. J Thorac Dis 2013;5 Suppl 3:S234-45. [PubMed]
- Sihoe AD. The evolution of minimally invasive thoracic surgery: implications for the practice of uniportal thoracoscopic surgery. J Thorac Dis 2014;6:S604-17. [PubMed]