Mediastinal lymph node dissection in surgical treatment for early stage non-small-cell lung cancer: lobe-specific or systematic?
The standard surgical treatment for early stage non-small-cell lung cancer (NSCLC) is lobectomy or pneumonectomy with systematic lymph node dissection (SND) (1,2). In 2006, the European Society of Thoracic Surgeons (ESTS) released guidelines for intraoperative lymph node staging in NSCLC, in which intraoperative procedures for lymph nodes were classified into five groups; selected lymph node biopsy, (systematic) sampling, lobe-specific lymph node dissection (L-SND), SND, and extended lymph node dissection; and it was recommended to provide SND in all cases of complete resection of NSCLC (3).
SND was first reported by Cahan in 1960 (4). This technique is designed to provide precise information on nodal status, which is necessary for optimal postoperative treatment, and to achieve better local cancer control that subsequently improves postoperative survival. However, the influence of SND on local control and survival remains uncertain, even though its value for accurate histologic staging of nodal status is well accepted. In addition, some reports have shown that SND tends to require longer operative times and to increase perioperative complications, compared to other procedures (5-7). Thus, many surgeons tend to avoid SND and perform “less invasive” intraoperative treatment for lymph nodes (8).
Based on this background, L-SND has attracted attention as a procedure in which some nodal stations are left untouched and unresected depending on the lobar location of the primary tumor. In L-SND, almost all ipsilateral hilar and mediastinal lymph node stations are dissected, but only specific mediastinal lymph node stations are left out depending on the lobar location of the primary tumor [stations 7, 8, and 9 for right upper lobe (RUL) or left upper lobe (LUL) tumors; stations 2R and 4R for right lower lobe (RLL) tumors; stations 4L, 5, and 6 for left lower lobe (LLL) tumors; and no specific stations for right middle lobe (RML) tumors are left out].
L-SND is designed based on characteristic mediastinal nodal metastasis patterns that occur for different primary tumor locations. In 1998, Okada et al. showed the characteristic skip N2 metastasis pattern (9), and in 1999, Asamura et al. reported characteristic patterns based on the primary tumor location (10). According to their report, tumors in the RUL and LUL tend to metastasize to the superior mediastinal lymph node station, whereas single-station metastasis to the subcarinal node is very rare; while tumors in the RLL or LLL show metastases to the subcarinal node and to the superior mediastinal or aortic node (10). However, Asamura et al. concluded that subcarinal node metastasis was the touchstone of mediastinal spread of RLL and LLL tumors because single-node or single-station metastases were more common in the subcarinal station and the prognosis of RLL or LLL tumors with both subcarinal and superior mediastinal lymph node metastases was extremely poor, even if SND was performed. Further, a specific lymphatic spread pattern was not identified for RML tumors (10).
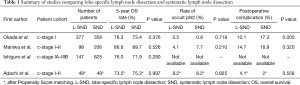
Comparing L-SND with SND from nodal staging and therapeutic perspectives, L-SND has been shown to have similar efficacy to SND for accurate nodal staging and postoperative survival, although other less invasive procedures, such as selected lymph node biopsy and systematic sampling, are inferior to SND (11,12). Okada et al. found equivalence of recurrence patterns, postoperative disease-free survival (DFS) and overall survival (OS) using L-SND (n=377) and SND (n=358) in 735 patients with clinicosurgical stage I NSCLC. The rate of occult pN2 disease also showed no significant difference (0.5% with L-SND vs. 0.8% with SND) (6). Maniwa et al. performed L-SND for 129 patients with NSCLC and found no significant difference in DFS and OS compared with patients who underwent SND. The rate of occult pN2 was also about equal in the two groups (13). Ishiguro et al. showed equivalency of L-SND for postoperative survival compared to SND using propensity score (PS) quartile-stratified Cox proportional hazard models in 147 patients who underwent L-SND (7). We recently reported non-inferiority of L-SND compared to SND for accuracy of staging and postoperative prognosis, using a PS matching method. Our results showed 5-year OS rates of 73.5% after L-SND and 75.3% after SND group, with no significant difference between the procedures, and a rate of occult pN2 of 8.2% for each procedure (14). Hishida et al. assessed the outcomes of 5,392 patients after complete resection (lobectomy with SND or L-SND) for clinical stage I-II NSCLC using an inverse probability of treatment weighting-adjusted Cox model and found the impressive result that L-SND had a favorable impact on postoperative survival, compared with SND (hazard ratio =0.68, 95% confidence interval: 0.60–0.77) (15).
L-SND has been suggested to be less invasive than SND. Okada et al. found significantly lower postoperative morbidity after L-SND (10.1%) compared to SND (17.3%), with the most common morbidity being arrhythmia, including atrial fibrillation (AF) (6). Maniwa et al. also showed that postoperative arrhythmia tended to be more common after SND than after L-SND (13). Intra- and postoperative AF are associated with mediastinal lymph node dissection and often require anticoagulant agents, cause prolongation of hospital stay and brain infarction, and may be fatal (16,17). The mechanism of onset involves surgical maneuvers during mediastinal nodal dissection and postoperative local inflammation around the vagal nerve, especially the cardiac plexus, and pulmonary veins. L-SND may prevent AF by avoiding resection of mediastinal lymph node stations near the cardiac plexus or pulmonary veins, and this hypothesis may be proven by the results of Okada et al. Complications of recurrent nerve paralysis after resection of nodal station 2R or 5 and chylothorax after resection of nodal station 7 may also be prevented by avoiding these stations using L-SND. Maniwa et al. found significantly shorter median operative times using L-SND (211 min) compared to SND (250 min) (P=0.0005) (13). Ishiguro et al. also showed that patients who underwent L-SND had a shorter operative time (169.3 vs. 201.9 min, P<0.001), in addition to less intraoperative blood loss (65 vs. 220 g, P<0.001) and a shorter hospital stay (13 vs. 15 days, P<0.001) compared to patients who underwent SND (7). These results (summarized in Table 1) all indicate that L-SND is less invasive than SND, and lead us to suggest that L-SND may be a better standard procedure than SND in surgery for early stage NSCLC.
Full table
In contrast to this suggestion, the L-SND procedure has been criticized in several studies. In particular, Bille et al. conducted a retrospective study in 1,667 patients with a diagnosis of clinical stage I NSCLC who underwent complete lung resection with SND. Occult N2 disease was detected in 9% of these patients (146/1,667), and risk factors for occult N2 disease were histology (adenocarcinoma) and vascular invasion. Skip metastases (defined as N2 lymph node involvement without N1 involvement) was observed in 34% of patients with pN2 disease (47/139), and 16% of patients with occult N2 disease had mediastinal lymph node metastases beyond the extent of L-SND (6 with RUL tumors and 2 with LUL tumors had metastasis to station 7; 6 with RLL tumors had metastasis to station 2R or 4R; and 8 with LLL tumors had metastasis to station 5 or 6); consequently, it was concluded that SND should be performed even in surgery for clinical stage I NSCLC (18). The rate of occult N2 was similar and the rate of skip metastasis was higher compared to previous reports (19). These results may reflect the insufficiency of selected lymph node biopsy, systematic nodal sampling, and hilar nodal dissection only for diagnosis of true N2 disease, and we agree with the conclusion in Bille et al. that mediastinal lymph node dissection should be performed even in patients with clinical stage I NSCLC.
However, the question remains of whether SND is really necessary for all patients with clinical stage I NSCLC. On this issue, we have a different view to that of Bille et al. From a therapeutic perspective, 22 patients with occult N2 disease had mediastinal lymph node metastases beyond the extent of L-SND in Bille et al., but half of these patients had multiple station N2 metastases. Such patients would be diagnosed with N2 disease and classified as stage IIIA after L-SND, and consequently would have received appropriate postoperative treatment. Only 11 patients had metastasis to a sole lymph node station that might have been missed by L-SND (2 with RUL tumors and 1 with a LUL tumor with metastasis only in station 7; 3 with RLL tumors with metastasis only in station 2R or 4R; and 5 with LLL tumors with metastasis only in station 5 or 6). These patients would have received a benefit from SND in terms of accurate staging, but these cases amounted to only 0.66% of all patients (11/1,667). Furthermore, 22 patients with occult N2 disease beyond the extent of L-SND could not have received a true R0 operation if they had undergone L-SND, but we have no evidence that SND improved the postoperative survival of these patients.
As mentioned above, Asamura et al. showed a poor prognosis of RLL or LLL tumors with both subcarinal and superior mediastinal lymph node metastases, even if SND was performed (10). Aokage et al. also found that a primary RUL or LUL tumor with metastasis to station 7 was associated with poor 5-year survival of 9.1% (20), and Hishida et al. showed a poorer prognosis for patients with pN2 disease outside the L-SND area, even after SND (15). In 78 patients with cN2/pN2 stage IIIA NSCLS, Matsunaga et al. showed greatly inferior postoperative 5-year DFS in patients with a RUL or LUL tumor with lower mediastinal (station 7, 8, 9) nodal metastases or a RLL or LLL tumor with upper mediastinal (station 2R, 4R, 5, 6) nodal metastases, compared to patients with a RUL or LUL tumor with only upper mediastinal nodal metastases or a RLL or LLL tumor with only lower mediastinal nodal metastases (0% vs. 29.6%, P<0.001) (21). Given these results, it is unclear whether SND improves survival in patients with occult N2 disease beyond the extent of L-SND.
In terms of invasiveness, Bille et al. found that 28% of patients had postoperative complications, which is a higher rate than in previous reports, and that the most common complication was AF (7.5%). As mentioned above, postoperative AF is associated with mediastinal lymph node dissection (16,17) and L-SND may prevent postoperative AF by leaving specific mediastinal lymph node stations near the cardiac plexus or pulmonary veins untouched and unresected, as found by Okada et al. Thus, considering the results of Bille et al. from therapeutic and postoperative perspectives, we consider that L-SND seems to be the more favorable procedure in surgical treatment of early stage NSCLC, compared to SND.
It is impossible to cure all patients with occult N2 disease completely, even if SND is used in surgery, and it is also impossible to eliminate postoperative complications completely, even if L-SND is performed during surgery. Therefore, the question of which of L-SND and SND is preferable for patients with early stage NSCLC may depend on which of minimization of the risk of overlooking occult N2 patients with an increased risk of postoperative complications among all patients compared to reduction of the risk of total postoperative complications with sacrifice of a few patients is more beneficial for all patients with early stage NSCLC. This is a difficult and somewhat ethical issue, and there is insufficient evidence to resolve this problem because all reported studies to date, including Bille et al., have been conducted retrospectively. To help to resolve this issue, a well-designed prospective randomized controlled trial (RCT) comparing L-SND to SND in patients with clinical stage I-II NSCLC is currently ongoing in Japan (JCOG1413, L-SPEC trial). We anticipate that our opinions stated above will be supported by the results of this RCT.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Naruke T, Goya T, Tsuchiya R, et al. The importance of surgery to non-small cell carcinoma of lung with mediastinal lymph node metastasis. Ann Thorac Surg 1988;46:603-10. [Crossref] [PubMed]
- Martini N, Flehinger BJ, Zaman MB, et al. Results of resection in non-oat cell carcinoma of the lung with mediastinal lymph node metastases. Ann Surg. 1983;198:386-97. [Crossref] [PubMed]
- Lardinois D, De Leyn P, Van Schil P, et al. ESTS guidelines for intraoperative lymph node staging in non-small cell lung cancer. Eur J Cardiothorac Surg 2006;30:787-92. [Crossref] [PubMed]
- Cahan WG. Radical lobectomy. J Thorac Cardiovasc Surg 1960;39:555-72. [PubMed]
- Lardinois D, Suter H, Hakki H, et al. Morbidity, survival, and site of recurrence after mediastinal lymph-node dissection versus systematic sampling after complete resection for non-small cell lung cancer. Ann Thorac Surg 2005;80:268-74. [Crossref] [PubMed]
- Okada M, Sakamoto T, Yuki T, et al. Selective mediastinal lymphadenectomy for clinico-surgical stage I non-small cell lung cancer. Ann Thorac Surg 2006;81:1028-32. [Crossref] [PubMed]
- Ishiguro F, Matsuo K, Fukui T, et al. Effect of selective lymph node dissection based on patterns of lobe-specific lymph node metastases on patient outcome in patients with resectable non-small cell lung cancer: a large-scale retrospective cohort study applying a propensity score. J Thorac Cardiovasc Surg 2010;139:1001-6. [Crossref] [PubMed]
- Little AG, Rusch VW, Bonner JA, et al. Patterns of surgical care of lung cancer patients. Ann Thorac Surg 2005;80:2051-6. [Crossref] [PubMed]
- Okada M, Tsubota N, Yoshimura M, et al. Proposal for reasonable mediastinal lymphadenectomy in bronchogenic carcinomas: role of subcarinal nodes in selective dissection. J Thorac Cardiovasc Surg 1998;116:949-53. [Crossref] [PubMed]
- Asamura H, Nakayama H, Kondo H, et al. Lobe-specific extent of systematic lymph node dissection for non-small cell lung carcinomas according to a retrospective study of metastasis and prognosis. J Thorac Cardiovasc Surg 1999;117:1102-11. [Crossref] [PubMed]
- Wright G, Manser RL, Byrnes G, et al. Surgery for non-small cell lung cancer: systematic review and meta-analysis of randomized controlled trials. Thorax 2006;61:597-603. [Crossref] [PubMed]
- Darling GE, Allen MS, Decker PA, et al. Randomized trial of mediastinal lymph node sampling versus complete lymphadenectomy during pulmonary resection in the patient with N0 or N1 (less than hilar) non-small cell carcinoma: results of the American College of Surgery Oncology Group Z0030 Trial. J Thorac Cardiovasc Surg 2011;141:662-70. [Crossref] [PubMed]
- Maniwa T, Okumura T, Isaka M, et al. Recurrence of mediastinal node cancer after lobe-specific systematic nodal dissection for non-small-cell lung cancer. Eur J Cardiothorac Surg 2013;44:e59-64. [Crossref] [PubMed]
- Adachi H, Sakamaki K, Nishii T, et al. Lobe-specific lymph node dissection as a standard procedure in surgery for non-small-cell lung cancer: A propensity score matching study. J Thorac Oncol 2017;12:85-93. [Crossref] [PubMed]
- Hishida T, Miyaoka E, Yokoi K, et al. Lobe-Specific Nodal Dissection for Clinical Stage I and II NSCLC: Japanese Multi-Institutional Retrospective Study Using Propensity Score Analysis. J Thorac Oncol 2016;11:1529-37. [Crossref] [PubMed]
- Wu DH, Xu MY, Mao T, et al. Risk factors for intraoperative atrial fibrillation: a retrospective analysis of 10,563 lung operations in a single center. Ann Thorac Surg 2012;94:193-7. [Crossref] [PubMed]
- Muranishi Y, Sonobe M, Menju T, et al. Atrial fibrillation after lung cancer surgery:incidence, severity, and risk factors. Surg Today 2017;47:252-8. [Crossref] [PubMed]
- Bille A, Woo KM, Ahmad U, et al. Incidence of occult pN2 disease following resection and mediastinal lymph node dissection in clinical stage I lung cancer patients. Eur J Cardiothorac Surg 2017;51:674-9. [Crossref] [PubMed]
- Gorai A, Sakao Y, Kuroda H, et al. The clinicopathological features associated with skip N2 metastases in patients with clinical stage IA non-small-cell lung cancer. Eur J Cardiothorac Surg 2015;47:653-8. [Crossref] [PubMed]
- Aokage K, Yoshida J, Ishii G, et al. Subcarinal lymph node in upper lobe non-small cell lung cancer patients: is selective lymph node dissection valid? Lung Cancer 2010;70:163-7. [Crossref] [PubMed]
- Matsunaga T, Suzuki K, Takamochi K, et al. Time to refine N2 staging? cN2α and cN2β based on local regional involvement provide a more accurate prognosis in surgically treated IIIA non-small-cell lung cancer than N2 alone or the number of node stations involved. Eur J Cardiothorac Surg 2014;46:86-91. [Crossref] [PubMed]


