Surgical resection of a well-differentiated inflammatory liposarcoma of the middle mediastinum: a case report
Introduction
Liposarcoma is a mesenchymal neoplasm that accounts for approximately 20% of all adult soft tissue sarcoma (1). Liposarcomas often arise in the lower extremities or the retroperitoneum; cases arising from the mediastinum are only found in 0.5–1.9% of all liposarcomas. Furthermore, liposarcomas are reported to account for less than 2% of mediastinal tumors (2). We herein present a rare case involving the complete resection of a well-differentiated inflammatory liposarcoma that arose from the middle mediastinum.
Case presentation
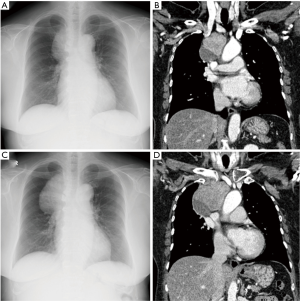
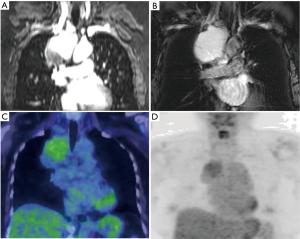
A 68-year-old woman was admitted to our hospital after an abnormal shadow in the right-upper lung field was pointed out in a medical examination. She had undergone surgery for right breast cancer at 65 years of age, and was followed up without recurrence. Chest X-ray and chest CT at the first visit (Figure 1A and 1B) and at 4 months later (Figure 1C and 1D) are shown in Figure 1. A mass shadow of 100 mm in diameter was observed to protrude from the mediastinum to the right-upper lung field on a chest X-ray (Figure 1A). A blood analysis revealed that there was no elevation of markers such as carcinoembryonic antigen (CEA), carbohydrate antigen15-3 (CA15-3), squamous cell carcinoma antigen (SCC), cytokeratin-19 fragments (CYFRA), pro-gastrin-releasing peptide (ProGRP), neutron-specific enolase (NSE), and angiotensin converting enzyme (ACE). Chest computed tomography (CT) revealed a massive shadow that was in contact with the right side of the trachea and the dorsal side of the superior vena cava in the right-middle mediastinum; A 55-mm area of the head side of the shadow showed high absorption, while a 45-mm area on the caudal side showed low absorption (Figure 1B). On chest magnetic resonance imaging (MRI), T1-weighted imaging showed an area of high signal intensity on the head side component and low signal intensity on the caudal side component (Figure 2A). Both components showed the same high intensity signal on T2-weighted imaging (Figure 2B). Although positron emission tomography (PET) revealed no significant difference between the two components, the FDG accumulation of the upper part tended to be stronger (SUVmax =3.67) in comparison to the lower part (SUVmax =2.55) (Figure 2C,2D). Fine-needle aspiration cytology was performed by endobronchial ultrasonography (EBUS); however, the diagnosis could not be determined. Since the infection tests were also negative, the possibility of an infectious lesion was denied. We therefore planned the surgical resection of the tumor for diagnostic and therapeutic purposes. The operation was postponed for 4 months based on the patient’s wishes. During this time, the high absorption component on the head side grew to 80 mm, while the low absorption part on the caudal side showed little change in size (Figure 1C,1D). The doubling time of the high absorption component was calculated as 76 days.
As the tumor invasion to superior vena cava was suspected from the preoperative image findings, we judged that a median sternum approach was needed in preparation for the angioplasty of superior vena cava. We performed tumor exeresis and thymectomy by a median sternotomy. During the surgery, the tumor was found to have adhered to the superior vena cava, trachea, brachiocephalic artery, and aortic arch, but there was no macroscopic infiltration. Tumor removal was performed after exposing and peeling of vessels without combined resection. There was no macroscopic residual tumor. The operation time was 8 hours and 19 minutes, with 890 mL of blood loss.
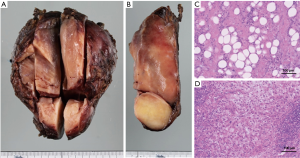
The resected tumor was 92 mm in size, and was composed of two solid components, which had different color tones (Figure 3A,3B). A pathological examination revealed that the component that showed low-absorption on CT (on the caudal side) consisted of various large and small adipocytes, accompanied by fibrous septa with some atypical cells. It was diagnosed as the lipoma-like subtype of well-differentiated liposarcoma (Figure 3C). The component that showed high-absorption on CT (on the head side) showed the proliferation of oval to spindle-shaped or polygonal cells with hyperchromatic nuclei that were arranged in a vaguely fascicular or haphazard pattern with fibro-collagenous, accompanied by myxoid stroma, dense lymphocytic inflammatory cell infiltration and lymphoid aggregates. Diagnosis of inflammatory subtype of well-differentiated liposarcoma was achieved (Figure 3D). Immunohistochemical staining was positive for CDK4, MDM2, and p16.
The postoperative course was good, and the patient was discharged on the 19th day after surgery. She is currently under regular observation at the outpatient department of our hospital; there has been no recurrence in the 8 months after surgery.
Discussion
Histologically, liposarcomas are classified into five types: well-differentiated type, mucus type, dedifferentiated type, pleomorphic type, and round cell type. The 5-year survival rates for these pathological types are reported to be 87.1%, 79.4%, 49.0%, 50.0%, and 42.3%, respectively (3). In addition, the well-differentiated type is further classified into three subtypes: lipoma-like type, sclerosis type, and inflammatory type. Although well-differentiated liposarcomas, which account for approximately 40% of all liposarcomas, are the most common type (3), well-differentiated inflammatory liposarcoma, which is accompanied by the infiltration of inflammatory cells such as lymphocytes and plasma cells, is a very rare subtype; its frequency among all liposarcomas is approximately 2% (4).
The imaging findings of liposarcoma are quite different; however, they tend to show a clear border and lobular images on MRI. The contrast effect varies depending on the tumor’s degree of differentiation; poorly differentiated tissue type tumors with higher malignancy tend to show greater contrast (5). Likewise, it is reported that liposarcomas with lower degrees of differentiation tend to show more non-uniform and higher CT values (6).
The first choice of treatment for liposarcoma is surgical resection. Complete resection is considered to be preferable because of the high rate of local recurrence. Cases of well-differentiated liposarcoma rarely show distant metastasis, and are expected to have a relatively good prognosis in comparison to other types such as the dedifferentiated type or pleomorphic type (7). Liposarcomas are basically considered to be resistant to chemotherapy and there is no established chemotherapy regimen; however, combined therapy with ifosfamide + doxorubicin was reported to be associated with a response rate of 30–40% (8).
We reported a rare case of liposarcoma of mediastinal origin that was pathologically diagnosed as the well-differentiated inflammatory type. After preoperative chest CT showed a high absorption component and a low absorption component, chest MRI was useful for differentiating the tumor from cystic disease. In addition, the CT high absorption component showed rapid growth, and the differential diagnosis from dedifferentiated liposarcoma before surgery was difficult. The enlargement of the tumor may have been attributable to an increase in inflammatory components due to the presence of tumor-derived G-CSF and IL-6—which has been reported in dedifferentiated liposarcoma (9)—or it may have occurred as a result of the invasion of inflammatory cells due to chronic inflammation.
In conclusion, we experienced a rare case involving the complete resection of a middle mediastinal tumor with two components that showed different growth rates, which were diagnosed as the lipoma-like subtype and inflammatory subtype of well-differentiated liposarcoma. Because of the diversity of imaging characteristics displayed by liposarcomas, it is sometimes difficult to make an accurate preoperative diagnosis of liposarcoma; however, the combination use of diagnostic tools such as CT, MRI, and PET can be useful for planning the treatment strategy.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Murphey MD. World Health Organization classification of bone and soft tissue tumors: modifications and implications for radiologists. Semin Musculoskelet Radiol 2007;11:201-14. [Crossref] [PubMed]
- Wychulis AR, Payne WS, Clagett OT, et al. Surgical treatment of mediastinal tumors: a 40 year experience. J Thorac Cardiovasc Surg 1971;62:379-92. [PubMed]
- Oh YJ, Yi SY, Kim KH, et al. Prognostic Model to Predict Survival Outcome for Curatively Resected Liposarcoma: A Multi-Institutional Experience. J Cancer 2016;7:1174-80. [Crossref] [PubMed]
- Kraus MD, Guillou L, Fletcher CD. Well-differentiated inflammatory liposarcoma: an uncommon and easily overlooked variant of a common sarcoma. Am J Surg Pathol 1997;21:518-27. [Crossref] [PubMed]
- Arkun R, Memis A, Akalin T, et al. Liposarcoma of soft tissue: MRI findings with pathologic correlation. Skeletal Radiol 1997;26:167-72. [Crossref] [PubMed]
- Taira N, Kinoshita S, Miyake T, et al. Primary liposarcoma of the anterior mediastinum--case report and review of literature. Jpn J Thorac Cardiovasc Surg 1998;46:450-4. [Crossref] [PubMed]
- Evans HL. Liposarcoma: a study of 55 cases with a reassessment of its classification. Am J Surg Pathol 1979;3:507-23. [Crossref] [PubMed]
- Jones RL, Fisher C, Al-Muderis O, et al. Differential sensitivity of liposarcoma subtypes to chemotherapy. Eur J Cancer 2005;41:2853-60. [Crossref] [PubMed]
- Hisaoka M, Tsuji S, Hashimoto H, et al. Dedifferentiated liposarcoma with an inflammatory malignant fibrous histiocytoma-like component presenting a leukemoid reaction. Pathol Int 1997;47:642-6. [Crossref] [PubMed]


