The effect of positive and negative message framing on short term continuous positive airway pressure compliance in patients with obstructive sleep apnea
Introduction
Obstructive sleep apnea (OSA) syndrome is a highly prevalent and under-diagnosed disorder (1-3) characterized by recurrent episodes of upper airway obstruction, which leads to sleep fragmentation, increased sympathetic activity, systemic inflammation and oxidative stress (4). OSA leads to daytime sleepiness, impaired functional capacity and quality of life, and moreover to an increased risk of cardiovascular and metabolic disease (5-7).
The best available treatment for OSA is currently continuous positive airway pressure (CPAP), which is aimed to ensure the upper airway patency during sleep (8). However, CPAP frequently remains a long-term treatment requiring good compliance to avoid long term consequences (9). Many patients have difficulties in maintaining long-term CPAP compliance and hence additional strategies need to be employed to improve this.
Patients’ education and training can be key intervention to increase long-term adherence to CPAP therapy (10), as they provide relevant information about the condition, the consequences of OSA and the benefits of CPAP therapy thus aiding patients in making an informed choice about their treatment (11).
Health related information can be presented in terms of either risk or benefit (12), with framed messages presenting this information to the patient in either a positive or a negative manner. To date the role of motivational message framing on adherence to CPAP treatment has been tested previously only in a uncontrolled study (13). Hence, we set out this prospective randomized study to challenge the hypothesis that compliance to CPAP therapy, defined as average CPAP daily usage and percentage of nights with CPAP use for more than 4 hours, in patients with OSA can be improved by delivering positively and negatively framed message as compared to standard care.
Methods
Patients
Consecutive patients referred to the Sleep Disorders Centre at Guy’s & St. Thomas’ Hospitals, London, United Kingdom for suspected OSA were prospectively screened using nocturnal pulse oximetry (Pulsox 300i, Konica Minolta Sensing Inc., Tokyo, Japan) for two consecutive nights at home. Patient who were found to have both a 4% oxygen desaturation index (4% ODI) ≥5 hour−1 and typical symptoms of sleep apnoea [Epworth Sleepiness Scale (ESS) >10 points] (14) or a 4% ODI greater than 15 hour−1 were invited for CPAP treatment and issued with an autoset CPAP device (APAP, S8/S9, ResMed Ltd, Sydney, Australia) for home use.
Exclusion criteria were mental or physical disability precluding compliance with the protocol for the duration of the study, and non-feasible trial follow-up. The local institutional review board approved the study (registration number: 2013-3801). The study data and collection were performed between July 2013 and April 2014.
Protocol
Patients were randomly assigned to one of the three groups: the first received positively framed messages in addition to CPAP, the second received negatively framed messages in addition to CPAP, and a control group entailed patients who received best standard care with CPAP, but no framed messages. The three groups were matched for age, sex and BMI.
In the positively and negatively framed groups, framed messages were read out to the patients during their CPAP collection appointment. The same investigator was in charge to read the messages without adding any evaluative comments and without interruption. As part of the clinical team the sleep technicians were in charge of explaining the CPAP machines. Laminated labels with the printed framed messages (positive or negative) were attached to the tube of the CPAP machines (see online supplement). The same messages were repeated once during weekly phone calls that were performed only for this purpose: the researcher was calling the patients and reading the messages after introducing himself. Any other questions by the patients during these phone calls were directed to the clinical team.
Patients assigned to the control group were followed according to the best standard care. This entailed an APAP collection session during which expert sleep technicians explained the importance of treating OSA and introduced APAP. All patients were instructed on the use of their devices and one-to-one sessions were offered for patients experiencing difficulties. After 2 weeks, all patients were reviewed for troubleshooting and compliance assessment. Fixed pressure CPAP was issued at this stage and all patients were reminded of the importance of treating OSA and the benefits of CPAP treatment.
2-week follow up
After two weeks of CPAP therapy patients were invited to return to the sleep centre to have their compliance data downloaded from the device and to exchange the APAP for a fixed pressure CPAP machine (ResMed Ltd., Sydney, Australia). During this appointment, an ESS score and data from the APAP secure digital (SD) card [residual apnoea-hypopnoea index (AHI); total and daily usage time; air leak and pressure over the last 14 days] were recorded. Fixed CPAP pressure was established according to the downloaded data (typically 95th percentile of average nocturnal pressure), and a fixed pressure CPAP machine was issued.
Phone calls
Following fixed pressure CPAP issue, patients were phoned weekly and read the framed health messages (up to a total of 6 phone calls per patient, see Supplementary). The phone calls typically lasted 2–3 minutes and were non-interactive. Patients listened to the messages and were asked not to discuss clinical issues with the person phoning to avoid an advantage over the standard care group. However, all clinical questions or complaints were directed to the clinical team (sleep specialists or qualified technicians) who phoned the patient back to address any clinical concerns. After three unsuccessful attempts to phone a patient, no further attempts were made until the next week’s call was due. The control group did not receive weekly phone calls, other than from the clinical team, as part of their standard care.
6-week follow up
After a total of 6 weeks of CPAP use (2 weeks APAP, and 4 weeks fixed pressure CPAP) patients returned the SD cards via mail or attended for a further appointment. Patients who attended in person were re-assessed by one of the clinical technicians and the ESS score was recorded. Data on the residual AHI, total and daily usage time, air leak and pressure was downloaded from SD cards presented during clinic appointments or from those mailed to the sleep disorders centre.
Sample size calculation
Trupp et al. (13) defined CPAP adherence as a usage of >4 hours per night over a 30-day period of home therapy. The mean percentage of usage was 52% for their total study cohort (median 53%) and the difference between positive and negative framing group was 21 percentage points (42.15% vs. 63.14%, P=0.033). With the expected standard variation of 20%, a power of >0.8, and two-sided testing with an alpha of 0.05, the sample size analysis comparing framing to standard care determined that we would need to include at least 31 patients in each group to avoid a type II error. Following minimization, we recruited more patients (positive framing group n=36, negative framing group n=37, control group n=39) into our study to generate matched groups.
Statistical analysis
Data are reported as mean [standard deviation (SD)], if not otherwise indicated. Normally distributed variables were compared using parametric tests, while non-normally distributed data were compared with non-parametric tests. More specifically, Chi-square tests and one-way analyses of variance (ANOVAs) were used to compare characteristics of participants across the different groups using Dunn’s correction. Within-group data (pre- and post-CPAP initiation) were compared using the Wilcoxon paired test, while within group variables were compared using the Student t-test for paired data. Spearman’s rank correlation coefficient was calculated for non-normally distributed variables. Linear regression was performed to define identify predictors of CPAP compliance including classical predictors such as age, sex and BMI, and sleep-disordered breathing related potential predictors factors such as baseline ESS and 4% ODI (more sleepy patients and patients with severe OSA tend to have greater compliance with CPAP as they observe a greater amelioration of their experience a greater improvement in their symptoms) (9), alongside APAP pressure (we suspected that a higher pressures can become more uncomfortable in patients treated with CPAP) and short-term APAP compliance (average daily usage and total hours used). All variables that showed non-normal distribution were log-transformed prior to being entered in the linear regression model. For all tests, a value of P<0.05 was considered significant. Statistical analysis of the data was performed using GraphPad Prism (Version 5.02, GraphPad Software Inc., San Diego, CA, USA) and SPSS (IBM SPSS Statistics for Windows, Version 20.0, Armonk, NY, USA).
Results
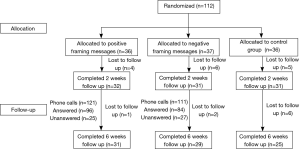
A total of 112 patients were allocated to three matched groups, 36 patients in the positively framed messages group, 37 in the negatively framed messages group, and 39 in the control group (Figure 1).
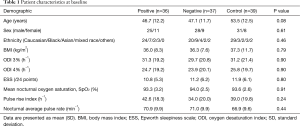
The majority of patients were middle-aged, male and obese with moderate-severe OSA (Table 1). No significant differences were observed across the three groups in demographic, anthropometric, or clinical variables, or in OSA severity indices.
Full table
2-week follow-up results
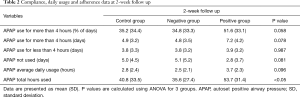
After 2 weeks of APAP treatment, OSA was controlled with a mean pressure of 13.2 (3.0) cmH2O. The residual AHI on APAP was low [median, 2.3 (1–5.82) hour−1], and the air leak on the interface was acceptable [1.5 (4.8) L·sec−1], with no differences observed among the groups.
All patients had a beneficial symptomatic response [ESS baseline 11.0 (6.0) vs. ESS at 2 weeks 9.2 (5.9) points, P<0.0001] with no significant differences among groups.
Patients allocated to the positive framed messages group used APAP more frequently; their number of days of APAP usage for longer than 4 hours was significantly higher when compared with both the negative framing group and the control group. Similarly, the total number of days of APAP usage was higher in the positive group, as well as the total number of hours of APAP usage (Table 2).
Full table
After the initial 2 weeks of APAP treatment, 15 patients stopped treatment, 4 from the positive framed group, 6 from the negative framed group and 5 from the control group (P=0.74).
6-week follow-up results
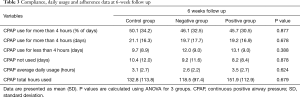
After 6 weeks of CPAP treatment, compliance data showed no differences between groups. CPAP average daily usage was similar in the three groups, 3.1 (2.7) hours in the control group, 2.6 (2.2) hours in the negative group and 3.5 (2.7) hours in the positive group (P=0.624), total hours of usage were 151.9 (112.9) hours, 118.5 (97.4) hours and 132.8 (113.8) hours, respectively (P=0.679). Further compliance data are summarised in Table 3.
Full table
There was no difference between 2 and 6 months compliance for each of the three groups. A total of 24 patients were lost to follow up at 6 weeks, either because they had returned their machine or because they could not be contacted, 5 in the positive framed group, 8 in the negative framed group, and 11 in the control group (P<0.05 for comparison between positively framed and control group; please refer to the online supplement for more information on the success rate of the follow up phone calls).
Correlations and regression analysis
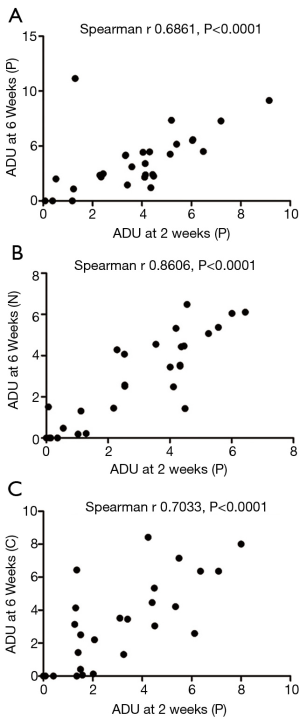
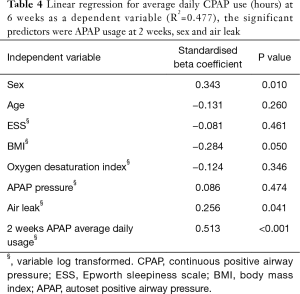
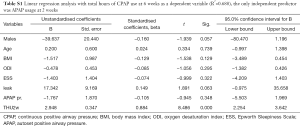
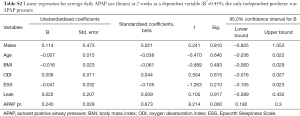
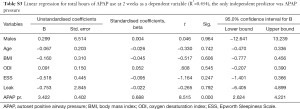
There was a significant correlation between the CPAP compliance at 2 weeks and at 6 weeks in all three groups (Figure 2). A linear regression analysis revealed that the independent predictors of CPAP compliance (Tables 4,S1,S2,S3) were the average daily APAP use at 2 weeks (P<0.001), and the total hours of APAP use at 2 weeks (P=0.006) for average daily CPAP use (hours) and total hours of CPAP use at 6 weeks, respectively (R2=0.467 and R2=0.309).
Full table
Full table
Full table
Full table
Sex resulted as a predictor for both compliance parameters at 6 weeks; BMI was an additional independent predictor for average daily CPAP use at 6 weeks. No independent predictors were identified when 2 weeks compliance data were included in the model as dependent variables. Ethnicity did not result as a significant predictor of 6 weeks’ average daily usage (standardized beta coefficient, 0.114, P=0.404) or total hours used (standardized beta coefficient, −0.224, P=0.110).
Discussion
To the best of our knowledge this is the first randomised and controlled study examining the impact of positively and negatively framed messages regarding CPAP usage on CPAP adherence and likelihood of continuation of therapy in OSA patients. We found that both these components of patients’ compliance to treatment can be enhanced at the short-term by positively framed messages. In particular, framing messages around CPAP therapy helped to avoid loss to follow up as compared to the standard care group; moreover, the use of positively framed messages was associated with a reduction in the dropout rate of CPAP users by more than 50% at 6 weeks. Compliance data at 2 weeks are closely related to results at 6 weeks, indicating that the importance of fully engaging OSA patients during the initial period of CPAP therapy.
Clinical significance
Maintaining long-term compliance with CPAP therapy remains a challenging task (15). Several healthcare systems have begun to implement automated electronic tracking systems following the American Thoracic Society recommendations (16), to better track long-term compliance. Previous investigators have found that education and support of patients on CPAP by the use of educational videos, phone calls, and home visits, can improve CPAP compliance (17). In line with those findings our data also support the view that framed messages during CPAP initiation can reduce the number of drop outs that from a service, although a lasting effect on compliance and usage time between different framing messages and standard care at 6 weeks of treatment could not be detected. Nonetheless, our results are consistent with earlier findings that revealed that short-term compliance with CPAP can predict long-term usage (18). Non-compliance should therefore be detected early on, and addressed adequately. Patients who struggle within the first two weeks require additional support to overcome problems with CPAP use.
Whilst Trupp et al. (13) found that negatively framed messages were associated with better CPAP compliance, our data revealed that positively framed messages increased short-term compliance. This difference might be explained by the observation that ‘gains and losses’ due to treatment are not equally perceived by patients: some patients experience a stronger emotional response from a ‘loss’ than they would from a similar ‘gain’ in their health status and vice versa. Potential differences in the cohorts studied, including race (19), socio-economic status (20), social factors (21) as well as the involvement of the spouse in the treatment (22), might have further contributed to these different findings. In our study ‘ethnicity’ was no predictor of CPAP usage but this could be due to the relatively low number of patients in the three subgroups. Cultural differences between populations could also conceivably affect CPAP compliance, although there are no published data specifically addressing this issue.
Of note, our study recruited consecutive patients with OSA in a tertiary referral centre starting on CPAP treatment, at variance with many studies were patients were highly selected for co-morbidities, intellectual capacity, geographic access and health consciousness (23). Moreover, we randomised patients to have a matched control group representing patients followed according to our standardised clinical protocol. In contrast, prior studies (13) had no control group and included only patients with a history of cardiovascular disease. Thus, it may be postulated that this subgroup of patients would be more receptive to negatively framed messages, considering the cardiovascular implications of untreated OSA.
A recently published controlled trial randomised patients beginning with CPAP therapy to receive either standard care, or an educational program that included a 25-minute educational video, an information booklet, a 20-minute patient-centred face-to-face motivational interview and a 10-minute phone call on day 2 of CPAP use (24). Although CPAP adherence decreased at 3 months, compliance remained significantly higher in the intervention arm (P<0.001). These results support the contention that engaging the patient during the initial period around CPAP setup is key for the success of treatment. In order to achieve improved CPAP adherence, dedicated time for education of the patients using repeated and multi-modal interventions can improve long-term use. Our data complement these findings, pointing out the importance of the initial two-weeks period following CPAP initiation.
Changing behaviour to support long-term medical therapy is difficult and suitable interventions are likely to require a complex approach. The use of framing messages (positively or negatively) can lead to variable outcomes in different scenarios, which might depend on comorbidities. Potentially, this intervention can significantly impact on healthcare delivery, quality of life and care-delivery related costs (12). Multiple confounders can influence the patients’ decision to continue with therapy other than the framing effect. A recent Cochrane review analysed 35 studies (involving 16,342 participants) in which two different types of framing were used to impact on patient behaviour related to various health conditions (non-OSA). Effects of attribute (positive vs. negative) and of goal (gain vs. loss) framing of the same health information were studied and the authors concluded that there is little if any consistent effect on health consumers’ behaviour (25) However, the studies included were heterogeneous and it was suggested that there is a clear framing effect in selected conditions. Considering the complexity of the different determinants and the lack of high-quality evidence (Table 5), further research is required supporting the use of behavioral interventions in patients with OSA on CPAP.
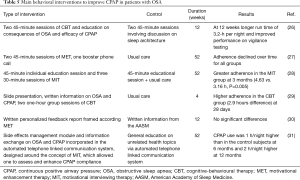
Full table
Limitations
In the current study, patients were not assessed using full polysomnography when first diagnosed. In the UK, it is standard to perform either respiratory polygraphyies or, frequently, nocturnal pulse oximetries to diagnose OSA, which is following evidence-based guidance according to the National Institute of Health and Clinical Excellence (NICE) (32). Our approach did not deliver messages using videos or further information booklets; more intense educational programs may be more successful in establishing a lasting effect on CPAP compliance. We also acknowledge that a non-message-based call for the control group would have been helpful to make the group more comparable with the positively and negatively framing groups. However, the study was designed to compare the intervention with standard medical care (‘usual care’). The design of our study was restricted, and the focus was medical rather than psychological in orientation. Due to the complexity of the parameters used for the intervention it is important to recognise the multiple factors associated with the development of framed messages (33-35). For instance, individuals respond differently to equivalent messages depending on whether they are framed to emphasize benefits (gain-framed) or costs (loss-framed). However, patients’ decision is influenced by several different factors involving the health behavior in question (36) (if behavior has a relatively certain outcome, individuals are more persuaded by gain-framed messages), motivational readiness (37) (patients in a stage of pre-contemplation have little intention to become active and are therefore less likely to respond to a message), credibility of the source of messages (38) (framing effects were not observed when the message source had low credibility) and mood induction (39) (fearful individuals tend to make more pessimistic decisions due to high perception of risk, low certainty, and lack of personal control).
The results of this study might have been further influenced by the fact that the same information that was presented during the appointments could have been perceived by different patients in different ways, leading to a receiver-dependent bias. The sample of patients studied was relatively small, and loss to follow up further reduced the total number of patients included in the final analysis. However, the number of patients who dropped out after the first two weeks was higher in the negative and in the control group, which suggests that motivating patients with positive framed messages may avoid an early drop out from the CPAP service. It was not possible to establish for sure whether patients were lost to treatment once they were lost to follow up. We had been unable to contact some patients after the 6 weeks period, meaning that adherence data about the difference between groups should therefore be interpreted with caution. However, in studies on patients with OSA treated with CPAP patients lost to follow up are commonly considered to be non-compliant (40). Lastly, CPAP compliance was on average lower than the recommended 4 hours/night. This could, in part, contribute to a reduced effect of the intervention between the three groups, but it reflects the level of compliance commonly observed in patients who are treated with CPAP.
Conclusions
Positively framed messages are a simple and inexpensive method to improve early CPAP compliance in patients with OSA and to reduce the drop-out rate at follow up by more than 50% compared to standard clinical care. However, the beneficial impact of framed messages after an initial 2-week period of CPAP use is limited and resources should be used to focus on the initial period around CPAP setup to encourage, educate, and engage with patients.
Further studies are required to identify receptive patient groups to framed messages and to describe detailed items analyses on which aspects of the positively or negatively framed messages are most effective. Future research needs to focus on the impact of framing on different comorbidities of patients with OSA such as hypertension or diabetes. Framed messages could be used as part of a multi-modal approach to construct a patient-based and individualised educational program during early CPAP use.
Supplementary
In the positive and negative framing group, the following statements were read out loud during the APAP collection. The patients were called weekly and the following messages were read out again, according to each framed group.
The positively framed messages were:
- Using CPAP at least 4 hours per night will reduce your daytime sleepiness and give you more energy.
- If you use your CPAP at least 4 hours per night, you can experience benefits that may save your life.
- Using CPAP at least 4 hours per night will increase your chances of lowering your blood pressure.
- Using your CPAP at least 4 hours per night decreases the risk of cardiovascular events.
- Using CPAP at least 4 hours per night will decrease your chances of experiencing sudden death.
The negatively framed messages were:
- If you do not use your CPAP at least 4 hours per night, you miss the chance to be less sleepy and have more energy.
- If you do not use your CPAP at least 4 hours per night, you cannot treat your sleep apnoea and not treating sleep apnoea can cost your life.
- If you do not use your CPAP at least 4 hours per night, you may decrease your chance of lowering your blood pressure.
- If you do not use your CPAP at least 4 hours per night, you may increase your chance of cardiovascular events.
- You may not decrease the risk of sudden death if you do not use your CPAP at least 4 hours per night.
A total of 121 and 111 phone calls were performed over the 6 weeks for the positive and negative framed group respectively. In the former group 25 phone calls were unanswered by the patients whilst in the latter group 27 phone calls were unanswered. There were no significant differences between the groups (P=0.50).
Acknowledgements
We are grateful for the support by the team at the Sleep Disorders Centre at Guy’s & St. Thomas’ NHS Foundation Trust, London. The authors want to thank Anna Maria Frigo for assistance with statistics and for her comments that greatly improved the manuscript. The research was supported by the National Institute for Health Research (NIHR) Biomedical Research Centre based at Guy’s and St. Thomas’ NHS Foundation Trust and King’s College London.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by local institutional review board (No. 2013-3801) and written informed consent was obtained from all patients.
References
- Young T, Palta M, Dempsey J, et al. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med 1993;328:1230-5. [Crossref] [PubMed]
- Steier J, Martin A, Harris J, et al. Predicted relative prevalence estimates for obstructive sleep apnoea and the associated healthcare provision across the UK. Thorax 2014;69:390-2. [Crossref] [PubMed]
- Peppard PE, Young T, Barnet JH, et al. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol 2013;177:1006-14. [Crossref] [PubMed]
- Deegan PC, McNicholas WT. Pathophysiology of obstructive sleep apnoea. Eur Respir J 1995;8:1161-78. [Crossref] [PubMed]
- Olaithe M, Bucks RS. Executive dysfunction in OSA before and after treatment: a meta-analysis. Sleep 2013;36:1297-305. [Crossref] [PubMed]
- Somers VK, White DP, Amin R, et al. Sleep apnea and cardiovascular disease: an American Heart Association/American College of Cardiology Foundation Scientific Statement from the American Heart Association Council for High Blood Pressure Research Professional Education Committee, Council on Clinical Cardiology, Stroke Council, and Council on Cardiovascular Nursing. J Am Coll Cardiol 2008;52:686-717. [Crossref] [PubMed]
- Campos-Rodriguez F, Martinez-Garcia MA, Reyes-Nuñez N, et al. Role of sleep apnea and continuous positive airway pressure therapy in the incidence of stroke or coronary heart disease in women. Am J Respir Crit Care Med 2014;189:1544-50. [Crossref] [PubMed]
- Sanders MH, Montserrat JM, Farré R, et al. Positive pressure therapy: a perspective on evidence-based outcomes and methods of application. Proc Am Thorac Soc 2008;5:161-72. [Crossref] [PubMed]
- Sawyer AM, Gooneratne NS, Marcus CL, et al. A systematic review of CPAP adherence across age groups: clinical and empiric insights for developing CPAP adherence interventions. Sleep Med Rev 2011;15:343-56. [Crossref] [PubMed]
- Smith I, Nadig V, Lasserson TJ. Educational, supportive and behavioural interventions to improve usage of continuous positive airway pressure machines for adults with obstructive sleep apnoea. Cochrane Database Syst Rev 2009;2:CD007736. [PubMed]
- Engleman HM, Wild MR. Improving CPAP use by patients with the sleep apnoea/hypopnoea syndrome (SAHS). Sleep Med Rev 2003;7:81-99. [Crossref] [PubMed]
- Tversky A, Kahneman D. The framing of decisions and the psychology of choice. Science. 1981;211:453-8. [Crossref] [PubMed]
- Trupp RJ, Corwin EJ, Ahijevych KL, et al. The impact of educational message framing on adherence to continuous positive airway pressure therapy. Behav Sleep Med 2011;9:38-52. [Crossref] [PubMed]
- Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 1991;14:540-5. [Crossref] [PubMed]
- Chai-Coetzer CL, Luo YM, Antic NA, et al. Predictors of long-term adherence to continuous positive airway pressure therapy in patients with obstructive sleep apnea and cardiovascular disease in the SAVE study. Sleep 2013;36:1929-37. [Crossref] [PubMed]
- Schwab RJ, Badr SM, Epstein LJ, et al. An official American Thoracic Society statement: continuous positive airway pressure adherence tracking systems. The optimal monitoring strategies and outcome measures in adults. Am J Respir Crit Care Med 2013;188:613-20. [Crossref] [PubMed]
- Hoy CJ, Vennelle M, Kingshott RN, et al. Can intensive support improve continuous positive airway pressure use in patients with the sleep apnea/hypopnea syndrome? Am J Respir Crit Care Med 1999;159:1096-100. [Crossref] [PubMed]
- Budhiraja R, Parthasarathy S, Drake CL, et al. Early CPAP use identifies subsequent adherence to CPAP therapy. Sleep 2007;30:320-4. [PubMed]
- Billings ME, Auckley D, Benca R, et al. Race and residential socioeconomics as predictors of CPAP adherence. Sleep 2011;34:1653-8. [Crossref] [PubMed]
- Simon-Tuval T, Reuveni H, Greenberg-Dotan S, et al. Low socioeconomic status is a risk factor for CPAP acceptance among adult OSAS patients requiring treatment. Sleep 2009;32:545-52. [Crossref] [PubMed]
- Lewis KE, Seale L, Bartle IE, et al. Early predictors of CPAP use for the treatment of obstructive sleep apnea. Sleep 2004;27:134-8. [Crossref] [PubMed]
- Glazer Baron K, Gunn HE, Czajkowski LA, et al. Spousal involvement in CPAP: does pressure help? J Clin Sleep Med 2012;8:147-53. [PubMed]
- McArdle N, Devereux G, Heidarnejad H, et al. Long-term use of CPAP therapy for sleep apnea/hypopnea syndrome. Am J Respir Crit Care Med 1999;159:1108-14. [Crossref] [PubMed]
- Lai AY, Fong DY, Lam JC, et al. The efficacy of a brief motivational enhancement education program on continuous positive airway pressure adherence in obstructive sleep apnea: A randomized controlled trial. Chest 2014;146:600-10. [Crossref] [PubMed]
- Akl EA, Oxman AD, Herrin J, et al. Framing of health information messages. Cochrane Database Syst Rev 2011.CD006777. [PubMed]
- Aloia MS, Di Dio L, Ilnicky N, et al. Improving compliance with nasal CPAP in older adults with OAHS. Sleep Breath 2001;5:13-21. [Crossref] [PubMed]
- Aloia MS, Arnedt JT, Strand M, et al. Motivational Enhancement to Improve Adherence to Positive Airway Pressure in Patients with Obstructive Sleep Apnea: A Randomized Controlled Trial. Sleep 2013;36:1655-62. [PubMed]
- Olsen S, Smith S, Oei T, et al. Motivational Interviewing (MINT) improves continuous positive airway pressure (CPAP) acceptance and adherence: a randomized controlled trial. J Consult Clin Psychol 2012;80:151-63. [Crossref] [PubMed]
- Richards D, Bartlett DJ, Wong K, et al. Increased adherence to CPAP with a group cognitive behavioral treatment intervention: a randomized trial. Sleep 2007;30:635-40. [Crossref] [PubMed]
- Roecklein KA, Schumacher JA, Gabriele JM, et al. Personalized feedback to improve CPAP adherence in obstructive sleep apnea. Behav Sleep Med 2010;8:105-12. [Crossref] [PubMed]
- Sparrow D, Aloia M, Demolles DA, et al. A telemedicine intervention to improve adherence to continuous positive airway pressure: a randomized controlled trial. Thorax 2010;65:1061-6. [Crossref] [PubMed]
- NICE. Sleep apnoea - continuous positive airway pressure (CPAP) [Internet]. NICE. Cited 31th May 2014. Available online: http://www.nice.org.uk
- Leventhal H. Fear appeals and persuasion: the differentiation of a motivational construct. Am J Public Health 1971;61:1208-24. [Crossref] [PubMed]
- Meyerowitz BE, Chaiken S. The effect of message framing on breast self-examination attitudes, intentions, and behavior. J Pers Soc Psychol 1987;52:500-10. [Crossref] [PubMed]
- Gallagher KM, Updegraff JA. Heath message framing effects on attitudes, intentions and behavior: a meta-analytic review. Ann Behav Med 2012;43:101-16. [Crossref] [PubMed]
- Rothman AJ, Salovey P. Shaping perceptions to motivate healthy behavior: the role of message framing. Psychol Bull 1997;121:3-19. [Crossref] [PubMed]
- Prochaska JO, Di Clemente CC. Stages and processes of self-change of smoking: toward an integrative model of change. J Consult Clin Psychol 1983;51:390-5. [Crossref] [PubMed]
- Jones LW, Sinclair RC, Rhodes RE, et al. Promoting exercise behaviour: an integration of persuasion theories and the theory of planned behaviour. Br J Health Psychol 2004;9:505-21. [Crossref] [PubMed]
- Robberson MR, Rogers RW. Beyond fear appeals: Negative and positive persuasive appeals to health and self-esteem. J Appl Soc Psychol 1988;18:277-87. [Crossref]
- Somers ML, Peterson E, Sharma S, et al. Continuous Positive Airway Pressure Adherence for Obstructive Sleep Apnea. ISRN Otolaryngol 2011;2011:943586. [Crossref] [PubMed]