Minimally invasive, multi-disciplinary approach for surgical management of a mediastinal congenital bronchogenic cyst in a 6-month-old infant
Introduction
Congenital mediastinal masses are not rare anomalies. In fact, early detection of mediastinal tumors via prenatal fetal ultrasonography is feasible. Early detection can avoid acute complications and allows for selection of the most appropriate time for intervention (1). However, few cases of mediastinal masses discovered through prenatal diagnosis have been reported previously.
We present a case of prenatal diagnosis of a mediastinal cyst through ultrasound, confirmed during infancy, using computed tomography (CT) and magnetic resonance imaging (MRI).
Case presentation
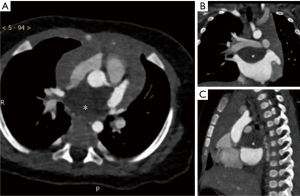
In March 2017, a 6-month-old male infant was admitted to the hospital for a 3-day history of respiratory distress. The physical examination and laboratory test results on admission were unremarkable, without any audible cardiac murmur. He was already well-known to us. At the gestational age of 24 weeks, prenatal fetal ultrasonography was performed as part of the Guangdong provincial-wide screening program for congenital heart disease (CHD). Ultrasonography revealed a mediastinal mass of unclear etiology. He was delivered at full term naturally. He was asymptomatic since birth; therefore, no immediate intervention was recommended. In December 2016, at 3 months old, transesophageal echocardiography was performed, which suggested cor triatriatum, a rare CHD. However, cardiac CT revealed a mid-mediastinal mass (30 mm × 21 mm × 20 mm) and no findings confirming cor triatriatum (Figure 1). Cardiac MRI was performed in February 2017, and the mass, which was noted to have enlarged (33 mm × 23 mm × 21 mm), was diagnosed as a benign mediastinal cyst.
Based on the findings on prenatal ultrasonography and postnatal imaging studies (CT, MRI), a benign mediastinal cyst was suspected. The cyst was below the tracheal carina, and the patient developed symptoms of cough and fever, which may be caused by oncothlipsis. Owing to the enlargement of the mass and the respiratory distress it has caused, the patient’s family felt very anxious and helpless. Under these circumstances, surgical management is the standard regimen (2). Unfortunately, there is no easy way to perform the surgery in a 6-month-old infant because of the high risk of anesthesia and the complicated perioperative management. However, if the mass is not removed, it can possibly affect respiratory function and make the patient susceptible to infection in the future. Previous studies, such as those by Shah et al. (2) and Jain et al. (3), have shown that, video-assisted thoracoscopic surgery (VATS) in an infant is a safe and effective procedure associated with low morbidity and a shorter hospital stay, only with high-quality anesthesia and perioperative management. In cases where a malignancy, such as a malignant thymoma, is suspected, VATS should nevertheless be performed, either for biopsy or for complete resection (4), because of the following advantages: (I) VATS produces minimal trauma; (II) large data show that VATS is a mature technology, associated with wide visualization and a good cancerous technique and (III) open surgery is associated with greater trauma, limited vision, and serious complications.
A multi-disciplinary conference consisting of the departments of congenital cardiac surgery, general thoracic surgery, radiology, and pathology reached the consensus that surgical resection is the treatment of choice for a primary mediastinal tumor without evidence of distant metastasis to relieve potential compression.
The decision of the team was to manage this mass with a right-sided VATS rather than a median sternotomy because the mass was located more posteriorly at the level of the left atrium. Cardiopulmonary bypass was available in case part of the left atrial wall needed to be resected en bloc for completion. VATS with minimal access was preferred over conventional thoracotomy, because it is associated with less postoperative pain, less likelihood of blood transfusion, and shorter postoperative hospital stay (5).
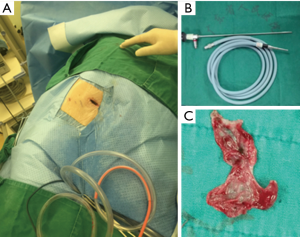
During the operation, the patient was intubated with a single-lumen endotracheal tube and ventilated with low tidal volume general anesthesia (Figure 2). The patient was placed in the standard left lateral decubitus position. One access incision (3 cm) was made along the anterior axillary line in the 4th intercostal space (ICS), with an additional camera port (1 cm) located along the posterior axillary line 1 ICS lower than the access incision and without rib spreading. A plastic wound protector was used to prevent implantation metastasis, and an additional suction tube was fixed to maintain a clear surgical field. The procedure was facilitated by using a 5-mm high-definition 30° thoracoscope, which improved visibility through the uniportal access (Figure 3).
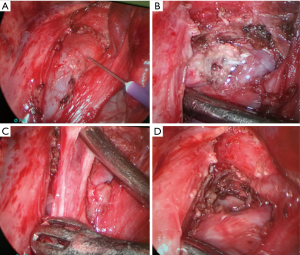
The operation began by exploring the space between the left atrium and the left pulmonary artery anterior to the left main bronchus, below the tracheal carina, after the mediastinal pericardium was incised parallel and anterior to the left phrenic nerve. The margin of the cyst was not readily visible. An electrocoagulation hook was used to dissect the anatomical structures. Other instruments used for dissection included a curved suction device and non-traumatic hemostatic forceps. The location of the cyst was finally localized by needle puncture, and viscous fluid was aspirated. Subsequently, the wall of the entire cyst was sharply dissected using electrocautery. A chest drain was left in the pleura through the camera port.
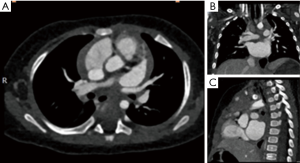
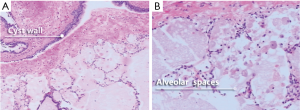
The patient’s postoperative course was uneventful (Figure 4), and the infant was discharged in stable condition 5 days postoperatively. The final pathological findings of the specimen were consistent with a bronchogenic cyst (Figure 5).
Discussion
The incidence of bronchogenic cysts is estimated to be 1 in 100,000 persons (6,7). Most of these cysts are congenital, and asymptomatic at the early stage. Hence, they are found most often in young adults and are rare in infancy.
CHD accounts for almost one-third of all congenital anomalies (8). Furthermore, the incidence of CHD in Asia is reported to be as high as 9.3 per 1,000 live births (8). Therefore, it is important to have an effective provincial-wide fetal ultrasonography screening program to identify fetuses with major CHDs so that they can be transferred to main tertiary care institutions for delivery and immediate access to sophisticated care, if needed. Since 2010, our institution has contributed to about 10–13% of the total number of cases in the database of European CHDs, and a significant percentage of our fetuses were prenatally diagnosed by our fetal ultrasonography program.
In this case, the cyst was discovered by the provincial-wide fetal ultrasonography screening program from our cardiovascular institute. Thereafter, a multi-disciplinary conference reached the consensus that surgical resection is the treatment of choice. Few cases of minimally invasive surgery in infancy have been described in literature. Patrick et al. (9) believe that thoracoscopy is a safe and effective method to resect mediastinal lesions in infants and children. In this case, a mediastinal lesion resection via VATS was performed, and the cyst was successfully resected.
In summary, we harnessed the provincial-wide fetal ultrasonography screening program to detect a mediastinal tumor. We formulated a management plan and applied prompt interventions. We speculate that many congenital mediastinal masses can be safely managed by VATS with less postoperative discomfort, less likelihood of blood transfusion, and shorter postoperative hospital stay.
Although this report is of a single case and follow-up duration is not long enough, we nevertheless make the first move to improve the pattern to a feasible, reliable, and efficient one, which could be used to treat similar patients.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained for publication of this case report and any accompanying images.
References
- Rios LT, Araujo Júnior E, Nardozza LM, et al. Prenatal diagnosis and postnatal findings of bronchogenic cyst. Case Rep Pulmonol 2013;2013:483864.
- Shah R, Reddy AS, Dhende NP. Video assisted thoracic surgery in children. J Minim Access Surg 2007;3:161-7. [Crossref] [PubMed]
- Jain P, Sanghvi B, Shah H, et al. Thoracoscopic excision of mediastinal cysts in children. J Minim Access Surg 2007;3:123-6. [Crossref] [PubMed]
- Cheng YJ, Wu HH, Chou SH, et al. Video-assisted thoracoscopic management of mediastinal tumors. JSLS 2001;5:241-4. [PubMed]
- Aydin Y, Araz O, Ozgokce M, et al. Video-Assisted Thoracoscopic Surgery of Mediastinal Cysts: Report of 13 Cases. Indian J Surg 2015;77:236-9. [Crossref] [PubMed]
- Duwe BV, Sterman DH, Musani AI. Tumors of the mediastinum. Chest 2005;128:2893-909. [Crossref] [PubMed]
- Takeda S, Miyoshi S, Minami M, et al. Clinical spectrum of mediastinal cysts. Chest 2003;124:125-32. [Crossref] [PubMed]
- van der Linde D, Konings EE, Slager MA, et al. Birth prevalence of congenital heart disease worldwide: a systematic review and meta-analysis. J Am Coll Cardiol 2011;58:2241-7. [Crossref] [PubMed]
- Partrick DA, Rothenberg SS. Thoracoscopic resection of mediastinal masses in infants and children: an evaluation of technique and results. J Pediatr Surg 2001;36:1165-7. [Crossref] [PubMed]


