Sudden hypotension occurring after 4 days of left-sided central catheter placement
Introduction
Insertion of central venous catheters (CVCs) is an important therapeutic procedure for critically ill patients. CVC provide a reliable venous access for medications, intravenous fluids, and hemodialysis as well as measurement of hemodynamic variables. Despite their common use and important role in the management of critically ill patients, complications following CVC insertion are reported to occur up to 15% of patients, consisted of mechanical, infectious, and thromboembolic complications (1).
Mechanical complications including arterial puncture, hematoma, pneumothorax, and hemothorax usually occur immediately after CVC insertion (1-3). However, physicians should be aware of the late mechanical complications such as vascular perforation and cardiac tamponade is also possible several hours or days later after successful CVC placement in special circumstances (3). Clinical symptoms and signs are usually nonspecific despite their life-threatening outcome, and the diagnosis and proper management can be delayed without high suspicion. Herein we report a case of delayed vascular perforation occurring after 4 days of left-sided hemodialysis catheter insertion.
Case presentation
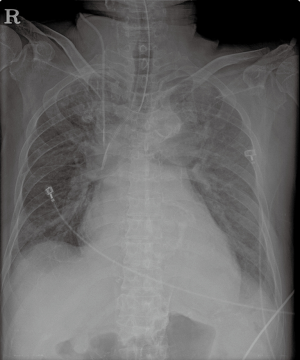
A 74-year-old male was admitted to our emergency intensive care unit for septic shock caused by Clostridium difficile colitis. He had been treated with immunosuppressive agents since renal transplantation in 1999. Septic shock progressed rapidly refractory to fluid resuscitation and antibiotic treatment and caused acute kidney injury and respiratory failure. A four-lumen CVC was already inserted into right internal jugular vein for administration of high dose vasopressors. Despite shock management with insertion of endotracheal tube for mechanical ventilation, he showed refractory metabolic acidosis with no urine output. Physicians decided to perform continuous renal replacement therapy (CRRT). The hemodialysis catheter was inserted into left subclavian vein using ultrasound guidance. Chest X-ray showed that the catheter tip was positioned within superior vena cava without any immediate complication (Figure 1).
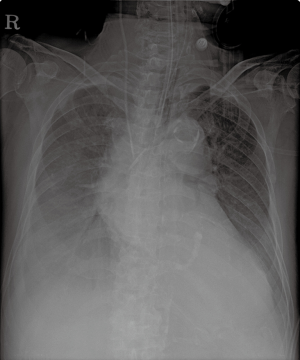
During hospital days, he seemed almost recovered from septic shock with tapering vasopressor smoothly. However, sudden hypotension with alarms of CRRT machine occurred on the fourth hospital day. After 1 L of fluid bolus infusion, hypotension soon recovered and CRRT showed good flow via dialysis catheter. Recurrent hypotension with alarms of CRRT machine developed after 3 hours of that event and was refractory to fluid infusion. Immediate chest X-ray showed a new right-sided pleural effusion (Figure 2) and thoracentesis revealed that the pleural fluid was bloody.
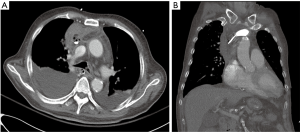
Chest computed tomography was emergently performed (Figure 3). The tip of catheter perforated the innominate vein and located with air bubbles in the mediastinum. Bedside echocardiography also showed the small amount of pericardial effusion without any echocardiographic features of cardiac tamponade.
Emergent operation for vascular repair was recommended, but his families refused surgical treatment. Emergent radiologic intervention was performed using covered self-expanding stents. Three covered stents were deployed into the innominate vein. However, bleeding persisted despite intervention and the patient’s status worsened progressively refractory to the administration of 0.9% saline bolus and transfusion of red blood cells. He finally expired on that day.
Discussion
A well-functioning hemodialysis catheter is essential for successful CRRT (2,4). Hemodialysis catheters can be inserted at three different access sites such as the internal jugular vein, the subclavian vein and the femoral vein. While right internal jugular vein was the first choice for catheter placement, subclavian veins are used as a last resort due to the risk of central venous stenosis (4,5). For all hemodialysis catheter insertions, the use of bedside ultrasound guidance is recommended for increased success rate and decreased complication rates (2,4,6).
The common complications associated with CVC are categorized as the immediate complications that occur during catheterization and the delayed complications after use of catheter. The common immediate complications include failure to place the catheter, arterial puncture, hematoma, air embolism, pneumothorax and hemothorax (2,7). Chest X-ray should be checked to ensure appropriate placement of catheter tip and no immediate complication (2,4,6). The delayed complications include infection, venous thrombosis, catheter migration and embolization (2,7). Among the delayed complications, delayed vascular perforation by CVC is a rare but life-threatening complication (2,8-10). Left-sided approach, large diameter catheters and old age were known as the risk factors for delayed vascular perforation (4,8). The left-sided catheter may move with changes in patient’s position, which result the tip to be perpendicular to the vascular wall and cause vascular erosion (2,8).
The diagnosis of delayed vascular perforation should be based on a high index of suspicion and particular attention to every patient with left-sided CVC who presents sudden onsets of unexplained hypotension, chest pain and respiratory difficulty, especially within 7 days after catheter placement (2,3,8). Immediate chest computed tomography should be performed to assess the precise location and extent of vascular injury and the management varies from conservative care to emergent operation, which depends on the severity of vascular injury as well as patient’s general status (2-4,8).
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
References
- McGee DC, Gould MK. Preventing complications of central venous catheterization. N Engl J Med 2003;348:1123-33. [Crossref] [PubMed]
- Marino PL. Marino's the ICU book. 4th ed. Philadelphia: Lippincott Williams & Wilkins, 2013.
- Teichgraber UK, Gebauer B, Benter T, et al. Central venous access catheters: radiological management of complications. Cardiovasc Intervent Radiol 2003;26:321-33. [PubMed]
- Vijayan A. Vascular access for continuous renal replacement therapy. Semin Dial 2009;22:133-6. [Crossref] [PubMed]
- Hernandez D, Diaz F, Rufino M, et al. Subclavian vascular access stenosis in dialysis patients: natural history and risk factors. J Am Soc Nephrol 1998;9:1507-10. [PubMed]
- National Kidney Foundation. III. NKF-K/DOQI clinical practice guidelines for vascular access: update 2000. Am J Kidney Dis 2001;37:S137-81. [Crossref] [PubMed]
- Eisen LA, Narasimhan M, Berger JS, et al. Mechanical complications of central venous catheters. J Intensive Care Med 2006;21:40-6. [Crossref] [PubMed]
- Walshe C, Phelan D, Bourke J, et al. Vascular erosion by central venous catheters used for total parenteral nutrition. Intensive Care Med 2007;33:534-7. [Crossref] [PubMed]
- Agrawal S, Payal YS, Sharma JP. A retrospective clinical audit of 696 central venous catheterizations at a tertiary care teaching hospital in India. J Emerg Trauma Shock 2012;5:304-8. [Crossref] [PubMed]
- Balasubramanian S, Gupta S, Nicholls M, et al. Rare complication of a dialysis catheter insertion. Clin Kidney J 2014;7:194-6. [Crossref] [PubMed]


