Clinical analysis of acute myocardial infarction caused by coronary embolism
Introduction
Acute myocardial infarction (AMI) is very common in clinic, and is often caused by incomplete coronary occlusion or complete occlusion induced by acute plaque rupture (1). Coronary angiography plays an important role in the etiology diagnosis and treatment of AMI (2). In previous studies, 1–12% of patients with AMI who underwent coronary angiography did not develop an irregular lumen, or coronary artery stenosis of <50% (3,4). In this type of AMI, causes of infarct-related artery occlusion vary from person to person, such as increased platelet or coagulation activity (hypercoagulability) (5-7), coronary artery spasm (8), coronary artery embolism (9,10), as well as coronary myocardial bridge, coronary artery ectasia and coronary artery dissection (11). AMI caused by coronary artery embolism is rare in clinical practice. This study conducts an analysis of the clinical characteristics of these patients.
Methods
From 2005 to 2015, five patients with AMI caused by coronary artery embolism were admitted to our hospital, and underwent primary percutaneous coronary intervention (PPCI). Among them, two patients were male and three patients were female; and the average age of these patients was 62 years old (range, 40–78 years old). All five patients were definitely diagnosed with AMI in the Emergency Department according to clinical symptoms, electrocardiogram (ECG) and myocardial enzymology indexes; and underwent PPCI treatment. In this study, clinical features and imaging characteristics of coronary artery angiography were retrospectively analyzed.
Results
Primary diseases
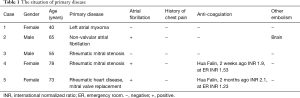
Among the five patients with coronary artery embolism, one patient had left atrial myxoma, one patient had non-valvular atrial fibrillation and three patients had rheumatic heart disease; and among these three patients with rheumatic heart disease, two patients had mitral valve stenosis, and one patient had post-mitral valve replacement. Furthermore, among the three patients with rheumatic heart disease, two patients were combined with atrial fibrillation. Among the three patients with atrial fibrillation, two patients received anticoagulant drug warfarin, while the other patient did not take any anticoagulant drug. Among the two patients that received warfarin, one patient had an international normalized ratio (INR) of 2.1 in a clinical test 2 months prior, and did not undergo any test during the last 2 months, while the other one patient had an INR of 1.9 two weeks prior, and took antibiotics for upper respiratory tract infection a week ago. In the test taken in the Emergency Department, the INR was 1.23 (primary disease conditions are listed in Table 1).
Full table
AMI manifestations
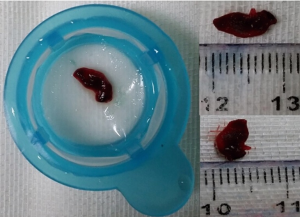
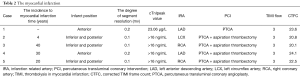
In all five patients, initial symptoms were chest pain, which was sustained without remission. ECG performances all matched ST segment elevation myocardial infarction, in which two patients had anterior wall myocardial infarction and three patients had inferior and posterior wall myocardial infarction. Myocardial enzymological indexes were consistent with AMI characteristic changes. Coronary angiography results of all five patients revealed the following: except for the occluded blood vessels, the remaining blood vessels were normal, and there were no signs of atherosclerosis (Figure 1). After percutaneous transluminal coronary angioplasty (PTCA) and thrombus suction, infarct-related blood vessels were free of residual stenosis; thus, stent implantations were not required. Five patients were all improved and discharged (myocardial infarction conditions are listed in Table 2).

Full table
Echocardiogram
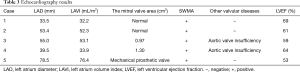
Four of five patients developed left atrium enhancement, and abnormal wall motions of the left atrium was found. Among them, one patient had post-mitral valve replacement, two patients had mitral stenosis, two patients had aortic valve insufficiency, and one patient had reduced left ventricular ejection fraction (LVEF) (echocardiogram performances are listed in Table 3).
Full table
Embolism in other parts of the body
One patient developed cerebral infarction in addition to AMI.
Discussion
Coronary artery embolism is not a common cause of myocardial infarction (12). It has been confirmed by autopsy that the incidence of myocardial infarction caused by coronary artery embolism was 10–13% (13). Furthermore, the consequences of embolism are related to the size of the emboli and diameter of the embolized vessels (13,14). Coronary artery embolism events can easily occur in patients after cardiac valve replacement, chronic atrial fibrillation, dilated cardiomyopathy, infective endocarditis, intracardiac shunts, cardiac myxoma, mural thrombus and hypercoagulative state (15-18). Most emboli would fall to the left coronary artery system, due to the shape and flow characteristics of the aortic valve (19). For patients suspected to have emboli inside the coronary artery, esophageal ultrasound should be used to evaluate whether residual intracardiac emboli exist (20). To date, there is still no consensus in the treatment of coronary artery embolism. For early AMI with ST segment elevation, there are currently two available treatments, intravenous thrombolysis and percutaneous intervention. Some literatures have reported that intravenous thrombolysis could be chosen for the treatment of this kind of coronary artery embolism (21-24). Some studies suggest that a double dose of thrombolysis therapy is superior to a single dose (17), but this view remains controversial. If the emboli falling off are infectious vegetation, thrombolysis therapy is inappropriate (13). Hernández et al. reported treatments for three cases of AMI caused by coronary artery embolism; and all cases were successfully treated with PTCA and stent implantation (25). Treatment methods using suction to deal with emboli inside the coronary artery have been reported (5,17,26,27). There are also studies that reported that some surgeons applied a distal protection device to prevent the distal end of the blood vessel from being embolized, which can improve distal blood flow (26,27).
Among the five patients, one patient had left atrial myxoma, one patient had non-valvular atrial fibrillation and three patients had rheumatic heart disease; and among these three patients with rheumatic heart disease, one patient had post-mitral valve replacement and two patients were combined with atrial fibrillation. Patients with non-valvular atrial fibrillation did not receive anticoagulant drugs, while two patients with rheumatic heart disease combined with atrial fibrillation received warfarin anticoagulant therapy. However, one patient did not undergo detection for blood coagulation function in the last two months, and obtained an incompetent INR score during the detection in the Emergency Department; while another patient had an INR of 1.9 two weeks ago, received antibiotics for upper respiratory tract infection one week prior, and INR fell below the norm. All five patients were diagnosed with ST segment elevation myocardial infarction by clinical symptoms, ECG and myocardial enzymologic changes; and received PPCI. For the patient with left atrial myxoma, after balloon dilatation, the emboli fell to the ending of left anterior descending artery (LAD) branch due to the small diameter of the distal vessel; thus, no suction was conducted. The rest of the four patients underwent both PTCA and thrombus suction. After recovery of TIMI-3 blood flow, all infarct-related vessels were free of residual stenosis. All five patients were considered to develop coronary artery embolism.
Among the two patients with rheumatic heart disease, one patient had post-mitral valve replacement with atrial fibrillation, orally received warfarin, but INR was not monitored in accordance with the provisions; and the other rheumatic heart disease patient with mitral stenosis and atrial fibrillation orally took warfarin, and coagulation indicators were monitored. However, for this patient, the last INR test failed to meet the required standard, and antibiotics were administered, which may have affected the anticoagulation effect of warfarin. The cause for the occurrence of coronary embolism in these two patients was considered to be the inferior anticoagulation effect. In addition, another non-valvular atrial fibrillation patient did not take any anticoagulation drug, and this was confirmed to be the culprit of multiple organ embolisms. The rheumatic heart disease patient, though without atrial fibrillation, developed left atrial enlargement; and the enlargement of the left atrium was considered as a risk factor for thrombosis. For asymptomatic left atrial myxoma, it is difficult to prevent the occurrence of embolism events. Five patients with coronary artery embolism were treated with PPCI treatment; and in two patients, the emboli was drawn out by an aspiration catheter. In case of a huge embolus, this was pulled out via a guiding tube (Figure 2).
Through the analysis of the above five AMI patients caused by coronary artery embolism, for patients with myocardial infarction caused by coronary artery embolism, emergency percutaneous coronary intervention therapies (including thrombus aspiration, percutaneous coronary artery angioplasty and stent implantation) are very critical. For simple embolization of coronary patients without atherosclerosis, the emboli should be removed as far as possible through various instruments and means; but it should not try to open the vessel by stent implantation, since this would increase the dose of antiplatelet agents that patients require, increase post-operative bleeding risk, and increase the risk of coronary events. For patients with high risk of embolism, effective anticoagulant therapy and close monitoring of the anticoagulation effect are important means of preventing the recurrence of embolisms.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the Ethics Committee of Beijing Chao-Yang Hospital, Capital Medical University (approval ID: 2015-subject-80).
References
- Libby P. Current concepts of the pathogenesis of the acute coronary syndromes. Circulation 2001;104:365-72. [Crossref] [PubMed]
- Gensini GG. Coronary arteriography: role in myocardial revascularization. Postgrad Med 1978;63:121-8. [Crossref] [PubMed]
- Alpert JS. Myocardial infarction with angiographically normal coronary arteries. Arch Intern Med 1994;154:265-9. [Crossref] [PubMed]
- Larsen AI, Galbraith PD, Ghali WA, et al. Characteristics and outcomes of patients with acute myocardial infarction and angiographically normal coronary arteries. Am J Cardiol 2005;95:261-3. [Crossref] [PubMed]
- Fuster V, Chesebro JH, Frye RL, et al. Platelet survival and the development of coronary artery disease in the young adult: effects of cigarette smoking, strong family history and medical therapy. Circulation 1981;63:546-51. [Crossref] [PubMed]
- Ross R, Kay R, Ambrose J, et al. Coronary thrombosis in the absence of angiographically-evident obstructive coronary disease. Chest 1983;84:768-70. [Crossref] [PubMed]
- Steele P, Rainwater J, Vogel R. Abnormal platelet survival time in men with myocardial infarction and normal coronary arteriogram. Am J Cardiol 1978;41:60-2. [Crossref] [PubMed]
- Gersh BJ, Bassendine MF, Forman R, et al. Coronary artery spasm and myocardial infarction in the absence of angiographically demonstrable obstructive coronary disease. Mayo Clin Proc 1981;56:700-8. [PubMed]
- Glazier JJ, McGinnity JG, Spears JR. Coronary embolism complicating aortic valve endocarditis: treatment with placement of an intracoronary stent. Clin Cardiol 1997;20:885-8. [Crossref] [PubMed]
- Granger EK, Rankin J, Larbalestier RI, et al. Obstruction of the right coronary artery ostium by an aortic valve papillary fibroelastoma. Heart Lung Circ 2005;14:266-8. [Crossref] [PubMed]
- Rigatelli G. Normal angiogram in patients with acute coronary syndrome: searching for unusual substrates of myocardial ischemia. Int J Cardiol 2005;99:25-7. [Crossref] [PubMed]
- Cheng TO. Coronary embolism. Int J Cardiol 2009;136:1-3. [Crossref] [PubMed]
- Aslam MS, Sanghi V, Hersh S, et al. Coronary artery saddle embolus and myocardial infarction in a patient with prosthetic mitral valve. Catheter Cardiovasc Interv 2002;57:367-70. [Crossref] [PubMed]
- Waller BF, Dixon DS, Kim RW. Embolus to the left main coronary artery. Am J Cardiol 1982;50:658-60. [Crossref] [PubMed]
- Kiernan TJ, Flynn AM, Kearney P. Coronary embolism causing myocardial infarction in a patient with mechanical aortic valve prosthesis. Int J Cardiol 2006;112:e14-6. [Crossref] [PubMed]
- Lavoie JP, Leduc L, Mercier LA. Embolic myocardial infarction in a pregnant woman with a mechanical heart valve on low molecular weight heparin. Can J Cardiol 2004;20:917-9. [PubMed]
- Hung WC, Wu CJ, Chen WJ, et al. Transradial intracoronary catheter-aspiration embolectomy for acute coronary embolism after mitral valve replacement. Tex Heart Inst J 2003;30:316-8. [PubMed]
- Kraus PA, Lipman J. Coronary embolism causing myocardial infarction. Intensive Care Med 1990;16:215-6. [Crossref] [PubMed]
- Prizel KR, Hutchins GM, Bulkley BH. Coronary artery embolism and myocardial infarction. Ann Intern Med 1978;88:155-61. [Crossref] [PubMed]
- Meier B. Catheter-based closure of the patent foramen ovale. Circulation 2009;120:1837-41. [Crossref] [PubMed]
- Dogan M, Acikel S, Aksoy MM, et al. Coronary saddle embolism causing myocardial infarction in a patient with mechanical mitral valve prosthesis: treatment with thrombolytic therapy. Int J Cardiol 2009;135:e47-8. [Crossref] [PubMed]
- Steinwender C, Hofmann R, Hartenthaler B, et al. Resolution of a coronary embolus by intravenous application of bivalirudin. Int J Cardiol 2009;132:e115-6. [Crossref] [PubMed]
- Atmaca Y, Ozdol C, Erol C. Coronary embolism in a patient with mitral valve prosthesis: successful management with tirofiban and half-dose tissue-type plasminogen activator. Chin Med J (Engl) 2007;120:2321-2. [PubMed]
- Quinn EG, Fergusson DJ. Coronary embolism following aortic and mitral valve replacement: successful management with abciximab and urokinase. Cathet Cardiovasc Diagn 1998;43:457-9. [Crossref] [PubMed]
- Hernández F, Pombo M, Dalmau R, et al. Acute coronary embolism: angiographic diagnosis and treatment with primary angioplasty. Catheter Cardiovasc Interv 2002;55:491-4. [Crossref] [PubMed]
- Belli G, Pezzano A, De Biase AM, et al. Adjunctive thrombus aspiration and mechanical protection from distal embolization in primary percutaneous intervention for acute myocardial infarction. Catheter Cardiovasc Interv 2000;50:362-70. [Crossref] [PubMed]
- Beran G, Lang I, Schreiber W, et al. Intracoronary thrombectomy with the X-sizer catheter system improves epicardial flow and accelerates ST-segment resolution in patients with acute coronary syndrome: a prospective, randomized, controlled study. Circulation 2002;105:2355-60. [Crossref] [PubMed]