Exercise Doppler echocardiography for the diagnosis of pulmonary hypertension: renewed interest and evolving roles
Exercise-induced pulmonary hypertension (PHT) was defined historically as an increase of >30 mmHg in the mean pulmonary artery pressure (MPAP) during exercise in patients who otherwise had a normal MPAP at rest (1). This concept was adopted for almost two decades before it was dropped from the diagnostic criteria of PHT in 2008 following the 4th World Symposium on PHT due to the ambiguity in the cut-off values for abnormality (2). In recent years, however, the tide might have turned. New and improved definitions for exercise PHT have been proposed and validated in a variety of patient cohorts, generating interest and bringing exercise PHT back into the limelight (3,4). As the latest iteration of the World Symposium on PHT in Nice approaches, this paper by van Riel et al. is both timely and relevant.
By way of introduction, exercise PHT is of potentially wide clinical use and carries important prognostic value. As a provocative test, it is capable of unmasking the underlying abnormal exercise pulmonary physiology in patients who have relatively normal resting pulmonary pressures (5). It has been shown to enable early detection of subclinical mild pulmonary arterial hypertension, which is a clinically relevant phase in the natural history of disease, lending opportunity for screening and perhaps early intervention before irreversible adverse pulmonary vascular remodelling sets in (5). Among patients with valvular heart diseases, the development of exercise PHT portents higher mortality, heart failure admission rates and post-operative cardiovascular events (6-10). As such, the importance of obtaining an accurate diagnosis of exercise-induced PHT cannot be over-emphasized. Right heart catheterisation remains the gold standard of pulmonary arterial pressures measurement and the cornerstone for the diagnosis of PHT despite its invasive nature.
In the study by van Riel et al., the authors compared the use of Doppler echocardiography to right-heart catheterisation at detecting PHT in a cohort of patients presenting with exertional intolerance but no prior history of PHT (11). The tricuspid regurgitation (TR) signals on Doppler echocardiogram were used for pulmonary artery pressure (PAP) calculations, which include systolic pulmonary artery pressure (SPAP) estimation from peak TR velocity and MPAP estimation from the TR velocity-time integral envelop. The TR signals were further graded from A to C, in the order of descending signal quality. Grade A TR signal was defined by extension of signal for at least half of ventricular systole and with a well-defined border, while grade B referred to signals with only one criterion fulfilled and grade C referred to signals with neither criterion fulfilled. In terms of feasibility, grade A signals were detected in 68% of patients at rest and 34% during peak exercise. Although the percentage of grade A TR signals dropped by almost 1/3 from rest to exercise, the correlation of MPAP and SPAP between Doppler echocardiography and right heart catheterisation for grade A signals was not overtly affected. In fact, the correlation between these two modalities was slightly higher on exercise compared to its corresponding value at rest (r=0.72, bias −2.9±8.0 mmHg at rest and r=0.75, bias −1.9±15.6 mmHg on exercise). Patients with grades B and C TR signals had poor correlation with right heart catheterisation. In patients with grade A TR signals, the MPAP to workload ratio (MPAP/workload) at 1.4 mmHg/10 watts was able to predict an abnormal pulmonary hemodynamic response during exercise [defined as >3.0 mmHg/L/min increase in the MPAP/cardiac output (CO) slope] with a sensitivity of 91% and specificity of 82% [area under the receiver operator’s curve 0.9, 95% confidence interval (CI), 0.77–1.0, P=0.001].
The correlations between exercise Doppler-derived PAP and that obtained from right heart catheterization in this paper were comparable to those reported in the literature (12,13) (Table 1). In the study by Kovacs et al., there was no significant difference in SPAP between exercise Doppler echocardiography and right heart catheterisation at increasing stages of semi-supine bicycle exercise (13). In a more recent study by Claessen et al., both MPAP and SPAP from echocardiography had good correlations with exercise cardiac magnetic resonance imaging combined with simultaneous invasive pressure registration (12). The echocardiographic-derived MPAP/CO was obtained in 87% of the study subjects. It was able to identify patients with abnormal pulmonary vascular reserve, as defined by invasively-derived MPAP/CO of >3 mmHg/L/min.
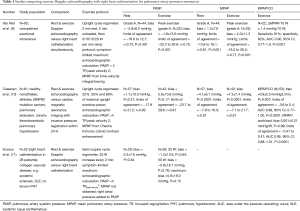
Full table
van Riel et al. have also shown that MPAP/workload could be a viable surrogate for MPAP/CO assessment. There are, in fact, several theoretical advantages to this approach. For starter, workload and CO have been shown to demonstrate a linear relationship (14). Also, using workload in place of CO means no additional calculations for CO are required. This could circumvent the problem of inaccurate CO measurement, especially from echocardiography whereby geometrical assumption of left ventricular outflow tract (LVOT) shape is made and the position of LVOT pulse Doppler is difficult to assess during exercise. However, the clinical utility of MPAP/workload warrants further studies as there is considerable amount of individual variability in CO for the same workload (15). Also, in patient with LV dysfunction, CO may reach a plateau state at high exercise intensity, during which further increase in workload is not translated into an increase in CO (16).
In this study by van Riel et al., patients without TR or in whom TR signal was not recorded were excluded from the study. Although the reason for absent TR signal (apart from a competent tricuspid valve) is unknown, it is not unreasonable to postulate that it could be related to poor signal quality. Therefore, the real feasibility of using TR signal for PAP calculation could be lower than that reported, after taking into account the exclusion criterion alluded to earlier. Our group has previously shown that exercise SPAP is feasible and reproducible in high-volume Heart Valve Clinics with dedicated imaging protocols and skilled operators. In patients with secondary mitral regurgitation, we could achieve a feasibility rate of 94% using semi-supine bicycle ergometer for SPAP measurement, without the need for contrast administration (13).
This study also highlights the importance of obtaining high-quality Doppler echocardiographic signals. Indeed, in selected instances, the quality of Doppler echocardiographic signals can be improved by the administration of contrast or the use of dedicated imaging protocol. The use of agitated colloid enhancement has been shown to improve the detection of TR, which was not apparent or absent on non-contrasted study (12). Although there is an inherent risk of pressure overestimation from ‘spike’ noise artefact, it is by and large a useful tool and should be considered when the Doppler signal is of suboptimal quality. Both the exercise and imaging protocols should be standardised and optimised for exercise echocardiography, which calls for multiple imaging parameters within a limited amount of time (6). For the assessment of PHT as a consequence of valvular heart diseases, our group advocate semi-supine bicycle ergometer, with the imaging table tilted according to optimal imaging windows. Symptom-limited graded exercise protocol, starting at 25 watts, followed by an increase of 25 watts every 2 min up to ≥80% of age-predicted target heart rate is recommended. The echocardiogram is performed continuously throughout exercise, allowing for PAP, ventricular sizes and functions assessment. Rather than interpreting elevated PAP in isolation, we recommend an integrated approach, taking into account patient’s age, exercise load, CO and systemic blood pressure for a comprehensive interpretation (6).
Despite its potential clinical utility and non-invasive nature, exercise PHT has yet to receive the recognition and attention it deserves. Historically, exercise PHT was part of the hemodynamic definition of PHT since the 1st World Symposium of PHT back in 1973 in Geneva. It was not until the 4th World Symposium of PHT in 2008 in Dana Point that exercise PHT was removed from the definition of PHT due to the lack of clear distinction of normal physiological from pathological state during exercise (2). There was considerable overlap with that observed in normal healthy population, especially in athletes or those above 50 years of age (2). Another problem with the definition of exercise PHT is that PAP varies according to the level, type and posture of exercise and there is a lack of standardization on these parameters. To overcome these limitations, new definitions of exercise PHT has been proposed. In the work by Herve et al., the authors proposed a composite definition of exercise PHT, which included mean pulmonary pressure, MPAP >30 mmHg and total pulmonary resistance >3 mmHg/L/min (14). The sensitivity and specificity of this improved definition were high, at 0.98 and 1.0 respectively. Instead of using PAP as the sole parameter, the effect of total pulmonary resistance, derived from MPAP/CO, was taken into account. The MPAP/CO ratio describes the steepness of PAP increase per unit increase of CO during exercise. It assesses the pressure-flow relationship, which should be relatively stable if the adaptation of pulmonary circulation is adequate. This approach helps to distinguish PHT from increased MPAP due to increased flow in healthy subject with normal total pulmonary resistance and has been gaining grounds in recent years (15). Apart from the progress made in the optimal definition of exercise PHT, there has also been interest in the methods of pulmonary pressures measurement. It has been suggested that serial PHT measurement during graded exercise might be a better alternative to peak exercise SPAP in conditions such as pulmonary arterial hypertension and scleroderma (16). This approach, however, is technically challenging and its application in other conditions calls for clinician’s judgement and discretion. The Heart Valve Clinic International Database (HAVEC) group advocates peak exercise SPAP for patients with valvular heart disease, considering the need to accommodate multiple imaging parameters within a limited imaging window period (17).
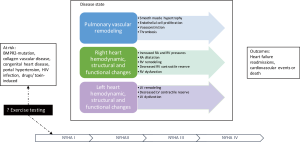
The take home messages are two-fold. First, this study strengthens the role of non-invasive imaging modality such as Doppler echocardiography and highlights the importance of obtaining high quality TR signals for meaningful PAP calculation. Second, the MPAP to workload ratio was able to predict abnormal pulmonary vascular response during exercise with good sensitivity and specificity. This study comes after the 2015 European Society of Cardiology and the European Respiratory Society (ESC/ERS) PHT guidelines, which recommend the use of echocardiography to evaluate the probability of PHT and defer the measurement of PAP to right heart catheterisation (18). In this regard, echocardiography could be a useful first line screening tool for patients with suspected PHT and a gatekeeper for right heart catheterisation by risk stratifying patients into low, intermediate and high echocardiographic probability of PHT. In terms of clinical application, despite the good correlation with right heart catheterisation, Doppler echocardiography should not be regarded as an alternative to right heart catheterisation. Echocardiography nevertheless plays a complementary role in the monitoring of the hemodynamic consequences of PHT such as left and right atrial/ventricular overload or dysfunction (Figure 1). It is also the ideal modality for serial non-invasive monitoring of pulmonary pressures. Depends on the goals of the managing physicians, echocardiography or right heart catheterisation can be considered under different circumstances. If the purpose is to confirm or refute the diagnosis of PHT with certainty and to further characterise the groups of PHT, it is probably prudent to proceed with right heart catheterisation. In patients with valvular diseases, e.g., symptomatic but non-severe mitral regurgitation or mitral stenosis, mild mitral regurgitation before cardiopulmonary bypass surgery, asymptomatic severe mitral regurgitation or mitral stenosis, as well as asymptomatic severe aortic stenosis, there is abundant evidence supporting the use of echocardiographic Doppler-derived SPAP at determining the decision for surgery or follow-up frequency (6-10,17,19,20).
All in all, the work by van Riel et al. is commendable. It is a well thought-out and elegantly executed study that adds to the confidence of PHT diagnosis using echocardiography. It calls for further, larger studies, preferably in a wider spectrum of patients with confirmed or suspected PHT.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Rich S, Dantzker DR, Ayres SM, et al. Primary pulmonary hypertension. A national prospective study. Ann Intern Med 1987;107:216-23. [Crossref] [PubMed]
- Badesch DB, Champion HC, Sanchez MA, et al. Diagnosis and assessment of pulmonary arterial hypertension. J Am Coll Cardiol 2009;54:S55-66. [Crossref] [PubMed]
- Lancellotti P, Martinez C, Bernard A. Pulmonary Pressures and Outcome in Primary Mitral Regurgitation: Paradigm Shift From Rung to Ladder. J Am Coll Cardiol 2016;67:2962-4. [Crossref] [PubMed]
- Naeije R, Vanderpool R, Dhakal BP, et al. Exercise-induced pulmonary hypertension: physiological basis and methodological concerns. Am J Respir Crit Care Med 2013;187:576-83. [Crossref] [PubMed]
- Tolle JJ, Waxman AB, Van Horn TL, et al. Exercise-induced pulmonary arterial hypertension. Circulation 2008;118:2183-9. [Crossref] [PubMed]
- Lancellotti P, Magne J. Stress echocardiography in regurgitant valve disease. Circ Cardiovasc Imaging 2013;6:840-9. [Crossref] [PubMed]
- Lancellotti P, Magne J, Donal E, et al. Determinants and prognostic significance of exercise pulmonary hypertension in asymptomatic severe aortic stenosis. Circulation 2012;126:851-9. [Crossref] [PubMed]
- Magne J, Donal E, Mahjoub H, et al. Impact of exercise pulmonary hypertension on postoperative outcome in primary mitral regurgitation. Heart 2015;101:391-6. [Crossref] [PubMed]
- Magne J, Lancellotti P, Piérard LA. Exercise-induced changes in degenerative mitral regurgitation. J Am Coll Cardiol 2010;56:300-9. [Crossref] [PubMed]
- Piérard LA, Lancellotti P. The role of ischemic mitral regurgitation in the pathogenesis of acute pulmonary edema. N Engl J Med 2004;351:1627-34. [Crossref] [PubMed]
- van Riel AC, Opotowsky AR, Santos M, et al. Accuracy of Echocardiography to Estimate Pulmonary Artery Pressures With Exercise: A Simultaneous Invasive-Noninvasive Comparison. Circ Cardiovasc Imaging 2017;10. [Crossref] [PubMed]
- Claessen G, La Gerche A, Voigt JU, et al. Accuracy of Echocardiography to Evaluate Pulmonary Vascular and RV Function During Exercise. JACC Cardiovasc Imaging 2016;9:532-43. [Crossref] [PubMed]
- Kovacs G, Maier R, Aberer E, et al. Assessment of pulmonary arterial pressure during exercise in collagen vascular disease: echocardiography vs right-sided heart catheterization. Chest 2010;138:270-8. [Crossref] [PubMed]
- Herve P, Lau EM, Sitbon O, et al. Criteria for diagnosis of exercise pulmonary hypertension. Eur Respir J 2015;46:728-37. [Crossref] [PubMed]
- Naeije R, Vonk Noordegraaf A, Kovacs G. Exercise-induced pulmonary hypertension: at last! Eur Respir J 2015;46:583-6. [Crossref] [PubMed]
- Lewis GD, Bossone E, Naeije R, et al. Pulmonary vascular hemodynamic response to exercise in cardiopulmonary diseases. Circulation 2013;128:1470-9. [Crossref] [PubMed]
- Garbi M, Chambers J, Vannan MA, et al. Valve Stress Echocardiography: A Practical Guide for Referral, Procedure, Reporting, and Clinical Implementation of Results From the HAVEC Group. JACC Cardiovasc Imaging 2015;8:724-36. [Crossref] [PubMed]
- Galiè N, Humbert M, Vachiery JL, et al. 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension: The Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT). Eur Respir J 2015;46:903-75. [Crossref] [PubMed]
- Lancellotti P, Magne J, Dulgheru R, et al. Clinical significance of exercise pulmonary hypertension in secondary mitral regurgitation. Am J Cardiol 2015;115:1454-61. [Crossref] [PubMed]
- Magne J, Pibarot P, Sengupta PP, et al. Pulmonary hypertension in valvular disease: a comprehensive review on pathophysiology to therapy from the HAVEC Group. JACC Cardiovasc Imaging 2015;8:83-99. [Crossref] [PubMed]


