Effects of Nuss procedure on thoracic scoliosis in patients with pectus excavatum
Introduction
Pectus excavatum (PE) is the most common congenital chest wall deformity (1). It is characterized by depression of the anterior chest wall and has been postulated to be a musculoskeletal disease (1,2). Previous studies have reported that deformities of the chest wall are related to deformities of the thoracic spine due to anatomical relationships (3-5); however, there have been few studies on the association between PE and scoliosis, and little is known about the subject (6-8). In addition, because the Nuss procedure forcibly corrects the deformed chest wall by insertion of metal bars and develops considerable stresses on the chest wall and the thorax, the Nuss procedure makes the anatomical changes in the thorax. We occasionally observe that body posture of the patients with PE improves after correction of PE. However, there is limited information about the effects of correction of PE on thoracic scoliosis (TS) (6,7,9-11). The purpose of the present study was to investigate the association between PE and TS and to analyze the effects of the Nuss procedure on the thoracic spinal curvature in patients with PE.
Methods
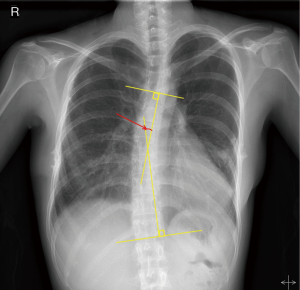
A total of 468 patients who underwent both the Nuss procedure and pectus bar removal for PE at the department of thoracic and cardiovascular surgery in a single tertiary hospital in Korea from March 2011 to January 2015 were retrospectively assessed and included into the present study. The inclusion criteria for the subjects were age 3 to 20 years, no major complication such as immediate reoperation after the Nuss procedure, no other combined congenital anomalies or diseases, no treatment for TS, and thoracic spine with rightward curvature. Simple chest radiograph and chest computed tomography (CT) were performed in all patients. Simple chest radiographs were routinely collected on a daily basis from admission to discharge and on every follow-up appointment as an outpatient. The Cobb angle (CA) is defined by the angle formed by the intersection of two lines drawn on a spinal radiograph of a patient suspected of having scoliosis. One line is drawn parallel to the lower surface of the lowest affected vertebral body, and the other is drawn parallel to the upper surface of the highest affected body (12) (Figure 1). CA was measured double- blindly by authors to quantify the magnitude of TS. CA in the thoracic spine was measured on simple chest radiography, and patients with a ≥10 degree coronal curvature in the thoracic spine were classified as having TS in the present study (8,12). We collected and compared these clinical parameters before the Nuss procedure (pre-correction) and after bar removal (post-correction) (pre-correction: data on admission for the Nuss procedure; post-correction: data on the last follow- up appointment as an outpatient within one month after bar removal). The patients were divided into two groups according to age at the time of correction (the early correction group, EG <10 years old, and the late correction group, LG 10 years old). The severity of PE was classified by the Haller index. Surgery, age, sex, body measurements (height, weight, and body mass index), severity, and morphology type were included in the parameters that influence CA and TS. The Nuss procedure using 1 to 3 pectus bars was performed to correct PE. The surgery for pectus bar removal was usually conducted 2 to 3 years after the Nuss procedure, according to patients’ age and postoperative status. In order to investigate the association between PE and TS and to analyze the effects of the Nuss procedure on TS in patients with PE, we performed (I) analyses of the post-corrective changes in CA and TS; (II) analyses of CA and TS with respect to age at the time of surgery, sex, morphology type, body measurements, and severity; and (III) analyses of the predictive factors of TS in patients with PE.
Statistical analysis
Comparisons between each group were analyzed with the Student’s t-test, the Paired t-test, or the age-adjusted ANCOVA (analysis of covariance) as appropriate. To investigate the relationship between two quantitative continuous variables, the Pearson analysis was conducted. The Chi-square test was used to compare the tallies or counts of categorical responses between two independent groups. Multivariate analysis was conducted using the logistic regression model to determine independent predictive factors of TS before and after correction of PE. The results were analyzed using the Statistical Package of Social Sciences version 22.0 (SPSS, Chicago, IL, USA), with a level of significance of 0.05.
Ethical committee
The present study was approved by the Institutional Review Board of Seoul St. Mary Hospital (KC16RISI0133). Written consent was obtained from the study subjects before participation. There are no conflicts of interest to declare.
Results
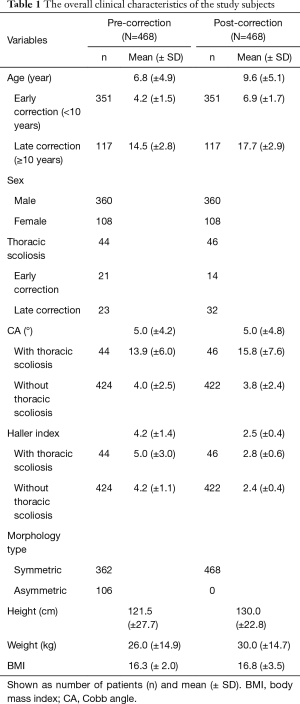
A total of 468 patients were assessed before and after correction of PE. The mean age of patients was 6.8 (±4.9) years pre-correctively and 9.6 (±5.1) years post-correctively. The mean Haller index was 4.2 (±1.4) pre-correctively and 2.5 (±0.4) post-correctively. The mean CA was 5.0 (±4.2)° pre-correctively and 5.0 (±4.8)° post-correctively. Regarding patients with TS, the number of patients with TS was 44 (9.4%) pre-correctively and 46 (9.8%) post-correctively. The mean age of patients with TS was 9.4 (±5.7) years pre-correctively and 13.4 (±4.8) years post-correctively. The mean CA of patients with TS was 13.9 (±5.9)° pre-correctively and 15.8 (±7.6)° post-correctively. The number of pectus type was 29 symmetric and 15 asymmetric types pre-correctively. The sex distribution was 30 males and 14 females pre-correctively and 27 males and 19 females post-correctively. In total, 22 of 44 patients with pre-corrective TS did not have TS after correction of PE, and 24 of 46 patients with post-corrective TS developed TS de novo after correction of PE. The mean observation period was 33.0 (±7.2) months. The overall clinical characteristics of the study subjects are summarized in Table 1.
Full table
Analysis of the post-corrective changes in CA and TS
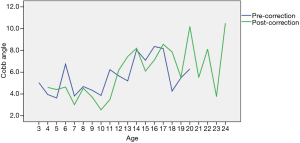
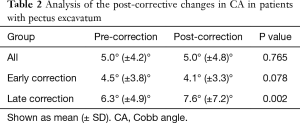
LG had a significantly higher CA and more frequent TS than EG (pre-correction: CA 6.3±4.9° vs. 4.5±3.8°, P<0.001, TS P<0.001; post-correction: 7.6±7.2° vs. 4.1±3.3°, P<0.001, TS P<0.001). There was a significant positive correlation between age and CA, both pre-correctively and post-correctively (both P<0.001) (Figure 2). The overall post-corrective CA was not significantly different from the overall pre-corrective one. However, the post-corrective changes in CA were different according to age at the time of correction (decreased in EG: 4.5°±3.8° vs. 4.1°±3.3°, P=0.078; increased in LG: 6.3°±4.9° vs. 7.6°±7.2°, P=0.002). Analysis of the post-corrective CA changes in patients with PE is summarized in Table 2.
Full table
Analysis of the post-corrective changes in CA in patients with TS
CA was decreased after correction of PE in the patients with pre-corrective TS (P=0.090). However, the post-corrective changes in CA were also different according to age at the time of correction. CA was significantly decreased in EG (P<0.001) and CA was increased in LG (P=0.053). Analysis of the post-corrective changes of CA in patients with preoperative TS is summarized in Table 3.
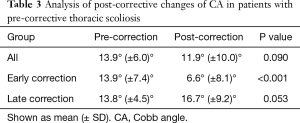
Full table
Comparison of the post-corrective changes in TS according to age at the time of correction
The number of patients with TS was decreased in EG (P=0.194) and significantly increased in LG (P=0.028). Comparison of the post-corrective changes in TS according to age at the time of correction is summarized in Table 4.
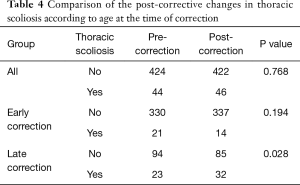
Full table
Analysis of TS and CA with respect to sex, severity, body measurement (height, weight, and BMI), morphology type, and number of bars
TS and CA according to sex
The pre-corrective and post-corrective incidence of TS in female patients were higher than in male patient (P=0.186 and P=0.003, respectively). The pre-corrective and post-corrective CA in female patients were also higher than in male patient (P=0.288 and P=0.048, respectively). The incidence of TS and CA according to sex is summarized in Tables 5 and 6.
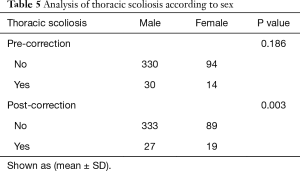
Full table
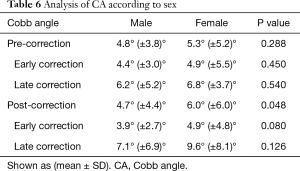
Full table
TS and CA according to severity
The severity of PE was classified by the Haller index. There was a significant positive association between the pre-corrective severity and CA (P<0.001). When patients were divided into two groups (the low and the high severity group) by the mean value of the Haller index (4.2), the high severity group had more frequent TS than the low severity group (P=0.076). The high severity group also had a significantly higher CA than the low severity group (5.4°±4.2° vs. 4.6°±4.1°, P=0.039).
TS and CA according to body measurements (height, weight, and BMI)
CA had a positive association with body measurements (pre-correction: height P=0.002, weight P=0.009, and BMI P=0.719; post-correction: height P<0.001, weight P<0.001, and BMI P=0.940). However, only the pre-corrective BMI in patients without TS was significantly higher than in patients with TS (P=0.010).
TS and CA according to the morphology of PE (symmetric vs. asymmetric type)
The asymmetric group had a significantly higher the pre-corrective CA than the symmetric group (6.0°±5.5° vs. 4.7°±3.7°, P=0.004). The asymmetric group had more frequently TS than the symmetric group. However, there was no statistical significance (P=0.061).
TS and CA according to number of bars used (single vs. multiple)
The Nuss procedure was performed using one to three pectus bars. There was significant difference in CA according to the number of bars used (pre-correction: single bar 4.7°±4.1° vs. multiple bar 5.9°±4.2°, P=0.012; post-correction: single bar 4.5°±4.0° vs. multiple bar 6.8°±6.9°, P=0.002). The patients with TS undergoing the Nuss procedure also required significantly more bars than the patients without TS (P=0.035).
Analysis of predictive factors of TS in patients with PE
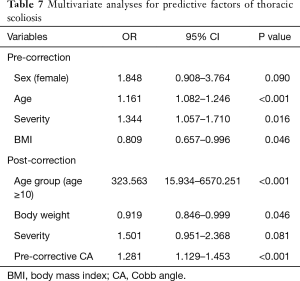
In order to investigate the independent predictive factors of TS in patients with PE, multivariate analysis was conducted using the logistic regression model (Backward, stepwise approach). TS was defined as an event. Age, sex, severity, morphological type, and body measurements were included as covariates for the multivariate analysis of pre-corrective predictive factors. Accordingly, age, severity, and BMI were identified as independent predictive factors of TS. In addition, age at the time of correction (EG and LG), sex, severity (the Haller index), morphological type, body measurements, number of bars (single and multiple), and pre-corrective CA and TS were included as covariates for the multivariate analysis of post-corrective predictive factors. Accordingly, age at the time of correction (EG and LG), weight, and pre-corrective CA were identified as independent predictive factors of TS. The results of the multivariate analysis of predictive factors are shown in Table 7.
Full table
Discussion
PE is among the most common congenital chest wall deformities (1). It has been postulated that PE is a musculoskeletal disease, but its cause or pathogenesis remains unclear (1,2). Previous studies have reported a high incidence of scoliosis among patients with PE due to anatomical relationships (3-7). However, there have been few comprehensive studies on the association between PE and scoliosis, and little is known about the subject (3,8). In addition, because the Nuss procedure forcibly corrects the deformed chest wall by insertion of metal bars and develops considerable stresses on the chest wall and the thorax, the Nuss procedure makes the anatomical changes in the thorax (11,13). However, the effects of the Nuss procedure on TS remain unclear (2,7,9-11). In the present study, we investigated the association between PE and TS and analyzed the effects of the Nuss procedure on TS in patients with PE. To the best of our knowledge, this study is the first to systematically investigate the association between PE and TS and to assess the effects of the Nuss procedure on TS in patients with PE.
Like previous studies, we found that the prevalence of TS in patients with PE was 9.4%, considerably higher than the normal prevalence of scoliosis (0.5% to 3%) (4-7). We also showed a positive association between age and CA as well as higher CA and more frequent TS in LG, both pre-correctively and post-correctively. From these findings, we assumed that TS was aggravated with age in patients with PE. We found that there were no significant post-corrective changes in CA and the number of patients with TS was increased after correction of PE. In addition, a previous study reported that correction of asymmetric PE with TS can sometimes exacerbate TS (11). The Nuss procedure might be misunderstood as exacerbating TS. However, the post-corrective changes in CA and the incidence of TS were different according to age at the time of correction. In particular, in patients with TS, CA was decreased in EG, and the incidence of TS was decreased in EG and increased in LG. From these findings, it can be assumed that the progression of TS can be reduced by early correction of PE. However, we do not know the exact reason why CA and TS were increased in LG. The reasons are probably due to combination of less effect of the Nuss procedure in LG, a simple time- related phenomenon, and the disease characteristics (i.e., progression with age).
We assumed that TS in patients with PE before correction of PE might be associated with age, sex, severity of the pectus deformity, pectus morphology type, and body measurements. In addition, we assumed that TS after correction of PE might be associated with age at the time of correction, sex, severity of PE, morphology type, body measurements, and pre-corrective TS and CA. The present study showed a higher CA and a higher incidence of TS in female patients, a higher CA and incidence of TS in the high severity group, a positive association between CA and body measurements, and a higher CA in asymmetric-type PE. To determine the independent predictive factors of TS in patients with PE, multivariate analysis using the logistic regression analysis was conducted. Accordingly, risk factors of TS included age and severity, and BMI was a protective factor of TS before correction of PE. In addition, risk factors of TS included age at the time of correction (LG) and pre-corrective CA, and body weight was a protective factor of TS after correction of PE.
Based on above findings, PE is associated with TS, and there are several predictive factors of TS in patients with PE. In addition, correction of PE had some significant effects on TS. The optimal age for the correction of the deformity is a controversial issue (14-17). However, these findings suggest that early correction of PE can reduce TS in patients with PE (11,13).
Surgeons should consider the association between PE and TS and the effect of the Nuss procedure on TS when deciding upon treatment in patients with PE and TS. With the caveat that more research is needed, we suggest that TS can be reduced by early correction of PE.
The present study has several limitations. First, it is small sample sized, retrospective and vulnerable to selection bias, especially toward early correction of PE. The retrospective nature of the present study might have an influence on the results. Second, there might have been some measurement errors of CA due to position, respiration, and other unknown factors. Third, the observation period is relatively short, limiting the statistical significance of some findings. In addition, because the follow-up appointments were completed before the mean age of TS in a considerable number of patients, it is unclear whether TS would eventually develop. Further long-term studies are needed.
Conclusions
There are associations between PE and TS. The Nuss procedure has some effects on TS and early correction of PE can reduce TS in patients with PE. There are both pre-corrective and post-corrective factors that are predictive of TS. Long-term and prospective studies in patients with PE and TS are required to confirm these observations.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the Institutional Review Board of Seoul St. Mary Hospital (KC16RISI0133). Written consent was obtained from the study subjects before participation.
References
- Park HJ, Jeong JY, Jo WM, et al. Minimally invasive repair of pectus excavatum: a novel morphology-tailored, patient-specific approach. J Thorac Cardiovasc Surg 2010;139:379-86. [Crossref] [PubMed]
- Niedbala A, Adams M, Boswell WC, Considine JM. Acquired thoracic scoliosis following minimally invasive repair of pectus excavatum. Am Surg 2003;69:530-3. [PubMed]
- Grivas TB, Burwell GR, Vasiliadis ES, et al. A segmental radiological study of the spine and rib--cage in children with progressive infantile idiopathic scoliosis. Scoliosis 2006;1:17. [Crossref] [PubMed]
- Bafus BT, Chiravuri D, van der Velde ME, et al. Severe hypotension associated with the prone position in a child with scoliosis and pectus excavatum undergoing posterior spinal fusion. J Spinal Disord Tech 2008;21:451-4. [Crossref] [PubMed]
- Hong JY, Suh SW, Park HJ, et al. Correlations of adolescent idiopathic scoliosis and pectus excavatum. J Pediatr Orthop 2011;31:870-4. [Crossref] [PubMed]
- Waters P, Welch K, Micheli LJ, et al. Scoliosis in children with pectus excavatum and pectus carinatum. J Pediatr Orthop 1989;9:551-6. [Crossref] [PubMed]
- Frick SL. Scoliosis in children with anterior chest wall deformities. Chest Surg Clin N Am 2000;10:427-36. [PubMed]
- Gurnett CA, Alaee F, Bowcock A, et al. Genetic linkage localizes an adolescent idiopathic scoliosis and pectus excavatum gene to chromosome 18 q. Spine (Phila Pa 1976) 2009;34:E94-100. [Crossref] [PubMed]
- Nagasao T, Miyamoto J, Tamaki T, et al. Stress distribution on the thorax after the Nuss procedure for pectus excavatum results in different patterns between adult and child patients. J Thorac Cardiovasc Surg 2007;134:1502-7. [Crossref] [PubMed]
- Chang PY, Hsu ZY, Chen DP, et al. Preliminary analysis of the forces on the thoracic cage of patients with pectus excavatum after the Nuss procedure. Clin Biomech (Bristol, Avon) 2008;23:881-5. [Crossref] [PubMed]
- Nagasao T, Noguchi M, Miyamoto J, et al. Dynamic effects of the Nuss procedure on the spine in asymmetric pectus excavatum. J Thorac Cardiovasc Surg 2010;140:1294-9.e1. [Crossref] [PubMed]
- Kim H, Kim HS, Moon ES, et al. Scoliosis Imaging: What Radiologists Should Know—Erratum. Radiographics 2015;35:1316. [Crossref] [PubMed]
- Wang Y, Chen G, Xie L, et al. Mechanical factors play an important role in pectus excavatum with thoracic scoliosis. J Cardiothorac Surg 2012;7:118. [Crossref] [PubMed]
- Park HJ, Sung SW, Park JK, et al. How early can we repair pectus excavatum: the earlier the better? Eur J Cardiothorac Surg 2012;42:667-72. [Crossref] [PubMed]
- Pawlak K, Gąsiorowski Ł, Gabryel P, et al. Early and Late Results of the Nuss Procedure in Surgical Treatment of Pectus Excavatum in Different Age Groups. Ann Thorac Surg 2016;102:1711-6. [Crossref] [PubMed]
- Kuru P, Cakiroglu A, Er A, et al. Pectus Excavatum and Pectus Carinatum: Associated Conditions, Family History, and Postoperative Patient Satisfaction. Korean J Thorac Cardiovasc Surg 2016;49:29-34. [Crossref] [PubMed]
- Zhang DK, Tang JM, Ben XS, et al. Surgical correction of 639 pectus excavatum cases via the Nuss procedure. J Thorac Dis 2015;7:1595-605. [PubMed]


