Challenging decision: ICU admission of critically ill elderly solid tumor patients
Cancer remains a major public health problem and a leading cause of mortality worldwide (1). Success in prevention, early detection and treatment of cancer has resulted in a continuous decline in cancer death rates with an overall drop of 25% over the last two decades. Introduction of smart molecules and development of new therapeutic armamentarium enabled advanced cancer patients to live longer in recent years. In accordance with these developments, intensive care unit (ICU) admissions have been steadily increasing in patients with solid tumors (2,3). Acute medical problems necessitate ICU admissions in approximately 5% of patients with solid tumors. Estimated every sixth to eight patient in European ICUs has underlying cancer (4).
Outcomes of critically ill patients with cancer admitted to the ICU have improved over the recent years thanks to the advances in cancer care and improvements in the management of organ dysfunctions, complications and infections (5,6). However, general reluctance with concept of futility remains to accept critically ill solid tumor patients to the ICU. Debate continues whether patients with metastatic cancer should be offered intensive care or end-of-life support. Moreover, data remains limited on the outcomes of solid tumor patients admitted to the ICU. The problem worsens in elderly patients with cancer.
On the other hand, debate continues as to whether age should be criteria in admission to the ICU (7). Mortality rises with advancing age, but selected elderly patients in the ICU do as well as younger patients. Frailty and comorbidities rather than chronological age should have priority in assessing patients requiring intensive care (7,8). Age alone should not preclude ICU admissions of critically ill geriatric patients. This should also apply to cancer patients as well as patients without cancer.
Auclin and colleagues have nicely studied outcomes of critically ill elderly patients in a recent report in Annals of Intensive Care (9). A total of 262 patients (11.3%) with solid tumors were analyzed among 2,327 elderly patients admitted to the ICU between 2009 and 2014. Indications for ICU admissions were usually not related to cancer. These patients were extremely ill with Simplified Acute Physiology Score (SAPS 2) of 61.9±22.5 compared to 56.9±22.4 in non-cancer patients (P<0.0001). Gastrointestinal, lung and genitourinary cancers were the most common cancer types and 60.3% of the patients had advanced metastatic cancer. Among those patients, 51.5% required mechanical ventilation, 48.1% inotropes and 12.6% dialysis. The ICU mortality was 32.5% for all elderly patients with no difference between those with and without cancer (33.6 vs. 32.7%; P=0.78). Cancer had no effect on ICU survival (OR: 0.96; 95% CI, 0.73–1.26; P=0.78). The 90-day mortality was 51.9% with 14 patients lost to follow up, indicating a possibly higher rate. Among ICU survivors, 52.7% of patients with advanced cancer went on to receive anti-cancer therapy. In multivariate analysis, elevated SAPS 2 score (HR: 1.05; 95% CI, 1.03–1.06, P<0.0001) and primary tumor site (P=0.001) were significantly associated with 90-day mortality. Patients with lung cancer (HR: 1.11; 95% CI, 0.59–2.08) and head and neck cancer (HR: 2.69; 95% CI, 1.25–5.79) had a higher risk of mortality among others. Patients with breast cancer had the lowest death risk (HR: 0.38; 95% CI, 0.11–1.27). However, previous cancer therapies, metastatic status and performance status were not associated with outcome. Prognostic factors predicting 90-day mortality were summarized in Table 1.
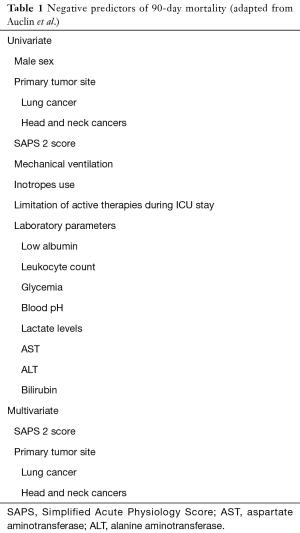
Full table
The study by Auclin et al. is one of the largest studies (n=262) reported to date assessing prognosis and long-term outcome of elderly cancer patients. One of the strengths of this study was inclusion of solid tumor patients only. Hematologic cancers were excluded from the analysis. Patients with short ICU stay <24 h and early limitation of therapies were also excluded to have a more focused study population. Detailed description of the underlying cancer including primary tumor, metastatic sites, and previous treatment modalities enabled analysis of their influence on patient outcomes. Ability to resume cancer therapy following ICU discharge was another important parameter as a potential endpoint for future studies. However, mortality rate of 32.5% was better than most of the studies published to date. Therefore, this study might not reflect real world experience because of focused selection of patients who would be expected to fare better with possible exclusion of patients not referred by oncologists or refused admission by the intensivists.
Studies of critically ill cancer patients admitted to the ICU have revealed that age alone was not a predictor of mortality (10-14). Severity of clinical condition as assessed by SAPS 2, Sequential Organ Failure Assessment (SOFA), Acute Physiology, Chronic Health Evaluation II (APACHE) or similar methods at ICU admission was of utmost importance rather than age. Uncontrolled or metastatic disease (11-13), sepsis or septic shock (11,12), organ dysfunction (11,12), performance status (12,13), use of mechanical ventilation (12-14), and type of solid tumor (14) were other factors associated with hospital mortality.
We have reviewed prognostic factors in critically ill cancer patients admitted to the intensive care unit in our center (12). ICU mortality rate in solid tumor patients was 53.8%. Age was not a prognostic factor between survivors and non-survivors. Rather, remission status, APACHE II score, sepsis and vasopressor requirement were independent predictors of ICU mortality.
Delayed ICU admission is another risk factor for death in cancer patients (3,10,12,15,16). Earlier evaluation and ICU trial could save some of the critically ill cancer patients when they are in better condition with less organ failure (3,12,17,18). Re-evaluation of treatment goals in days 3–5 of ICU stay may enable better prediction of individual course and outcome of critically ill cancer patients.
Oncologists’ and intensivists’ attitudes toward the care of critically ill cancer patients differ (19). Oncologists tend to focus more on the cancer characteristics, while intensivists mainly care about organ failure when assessing critical cancer patients. Intensivists are more pessimistic regarding clinical outcome of patients with cancer while using life support measures. Oncologists, on the other hand, tend to overestimate patient survival (20). Conflicts may arise during the care of critically ill cancer patients in the management of the same situation. Different perception of the disease may lead to underestimation of the risks and overestimation of the survival expectation. Therefore, multidisciplinary approach with frequent meetings and case discussions may help reduce misperceptions and conflicts among intensivists and other specialties (21). Mortality rates are reduced in medical ICU patients receiving care by a multidisciplinary team. Furthermore, it is of paramount importance to inform and share decisions with the patients and caregivers for optimal patient outcomes (22).
In conclusion, critically ill elderly cancer patients benefit equally from intensive care compared to non-cancer patients with similar mortality rates. Age and diagnosis of cancer should not be contraindications for ICU admission. Because severity of clinical condition was more important in terms of outcome prediction, early ICU admission should be considered in all critically ill cancer patients, regardless of age. Both oncologists and intensivists need a better-defined, evidence-based guideline to predict prognosis for critically ill patients with cancer for decision making. Comprehensive care with close involvement of oncologists, intensivists, and palliative care specialists is necessary for appropriate medical management.
Acknowledgements
None.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2017. CA Cancer J Clin 2017;67:7-30. [Crossref] [PubMed]
- Puxty K, McLoone P, Quasim T, et al. Risk of critical illness among patients with solid cancers: a population-based observational study. JAMA Oncol 2015;1:1078-85. [Crossref] [PubMed]
- Schellongowski P, Sperr WR, Wohlfarth P, et al. Critically ill patients with cancer: chances and limitations of intensive care medicine - a narrative review. ESMO Open 2016;1:e000018. [Crossref] [PubMed]
- Taccone FS, Artigas AA, Sprung CL, et al. Characteristics and outcomes of cancer patients in European ICUs. Crit Care 2009;13:R15. [Crossref] [PubMed]
- Shimabukuro-Vornhagen A, Boll B, Kochanek M, et al. Critical Care of Patients With Cancer. CA Cancer J Clin 2016;66:496-517. [Crossref] [PubMed]
- Biskup E, Cai F, Vetter M, et al. Oncological patients in the intensive care unit: prognosis, decision-making, therapies and end-of-life care. Swiss Med Wkly 2017;147:w14481. [PubMed]
- Nathanson BH, Higgins TL, Brennan MJ, et al. Do elderly patients fare well in the ICU? Chest 2011;139:825-31. [Crossref] [PubMed]
- Kizilarslanoglu MC, Civelek R, Kilic MK, et al. Is frailty a prognostic factor for critically ill elderly patients? Aging Clin Exp Res 2017;29:247-55. [Crossref] [PubMed]
- Auclin E, Charles-Nelson A, Abbar B, et al. Outcomes in elderly patients admitted to the intensive care unit with solid tumors. Ann Intensive Care 2017;7:26. [Crossref] [PubMed]
- Soares M, Silva UV, Teles JM, et al. Validation of four prognostic scores in patients with cancer admitted to Brazilian intensive care units: results from prospective multicentre study. Intensive Care Med 2010;36:1188-95. [Crossref] [PubMed]
- Fisher R, Dangoisse C, Crichton S, et al. Short-term and medium-term survival of critically ill patients with solid tumours admitted to the intensive care unit: a retrospective analysis. BMJ Open 2016;6:e011363. [Crossref] [PubMed]
- Aygencel G, Turkoglu M, Turkoz Sucak G, et al. Prognostic factors in critically ill cancer patients admitted to the intensive care unit. J Crit Care 2014;29:618-26. [Crossref] [PubMed]
- Azevedo LCP, Caruso P, Silva UV, et al. Outcomes for patients with cancer admitted to the ICU requiring ventilatory support: results from a prospective multicenter study. Chest 2014;146:257-66. [Crossref] [PubMed]
- Xia R, Wang D. Intensive care unit prognostic factors in critically ill patients with advanced solid tumours: a 3-year retrospective study. BMC Cancer 2016;16:188. [Crossref] [PubMed]
- Azoulay E. A new standard of care for critically ill patients with cancer. Chest 2014;146:241-4. [Crossref] [PubMed]
- Mokart D, Lambert J, Schnell D, et al. Delayed intensive care unit admission is associated with increased mortality in patients with cancer with acute respiratory failure. Leuk Lymphoma 2013;54:1724-9. [Crossref] [PubMed]
- Lecuyer L, Chevret S, Thiery G, et al. The ICU trial: a new admission policy for cancer patients requiring mechanical ventilation. Crit Care Med 2007;35:808-14. [Crossref] [PubMed]
- Ñamendys-Silva SA, Plata-Menchaca EP, Rivero-Sigarroa E, et al. Opening the doors of the intensive care unit to cancer patients: a current perspective. World J Crit Care Med 2015;4:159-62. [PubMed]
- Nassar AP Jr, Dettino AL, Amendola CP, et al. Oncologists' and intensivists' attitudes toward the care of critically ill patients with cancer. J Intensive Care Med 2017.885066617716105. [PubMed]
- Clément-Duchêne C, Carnin C, Guillemin F, Martinet Y. How accurate are physicians in the prediction of patient survival in advanced lung cancer? Oncologist 2010;15:782-9. [Crossref] [PubMed]
- Kim MM, Barnato AE, Angus DC, et al. The effect of multidisciplinary care teams on intensive care unit mortality. Arch Intern Med 2010;170:369-76. [Crossref] [PubMed]
- Von Roenn JH. Critically ill patients' preferences regarding aggressive medical interventions: Can we hear the patient's voice? JAMA Oncol 2016;2:83-4. [Crossref] [PubMed]


