An interview between a pulmonologist and a thoracic surgeon—Pleuroscopy: the reappearance of an old definition
As we all know, in 1910 Hans Christian Jakobaeus was the first to use ‘cystoscopy’ for the examination of serus cavities (1). This method was used for the tuberculosis treatment and was abandoned after few years. Since 1945 many other researchers used this technique to explore the thoracic cavity and to perform interventions in pleura and lung. Accordingly, this technique was named after Jakobaeus and called “Jakobaeus operation” (2). However, throughout the years other definitions emerged to describe the technique. From 1923 ‘pleuroscopy’ was the most common used definition (3). In later years, pulmonologists and interventional pulmonologists adopted the term ‘medical thoracoscopy’. Another term that abandons in literature is ‘Surgical or therapeutic thoracoscopy’ (4,5) and of course there is the video-assisted thoracic surgery (VATS) technique. In this interview, we will clarify a few important questions concerning pleuroscopy.
Which is the most appropriate definition for this technique? In other words, what are the characteristics of this procedure and how can I name it?
We are reading for five different definitions (Jakobaeus operation, pleuroscopy, medical thoracoscopy, Surgical or therapeutic thoracoscopy and VATS technique) which might have something in common. Generally when we perform a procedure we need an operator, which might be a surgeon or an interventional pulmonologists. Also we need a place like an operation theatre or a sterilized room with the appropriate tools. In any case we need some kind of anesthesia, which might be local or sedation. General endotracheal, epidural or general non endotracheal with spontaneous breathing makes the presence of the anesthesiologist necessary. The operator even in mild sedation must attend only to the procedure which means that it is not necessary to hear to the patient’s agony or to have in mind the anesthesia effect. Finally, the procedure might be diagnostic or therapeutic. The use of sedation to one or two ports and the use of rigid instruments to see the pleura cavity were the actions that defined the Jakobaeus technique.
Are these enough to characterize our technique? Which is the difference from our practice nowadays?
In recent years, ‘medical thoracoscopy’ performed by interventional pulmonologists, needs a room equipped with a cardiac monitor, a pulse oxymeter, a blood pressure cuff, IV lines, drapes and propofol sedation.
What is the difference between a place like this and an operation theatre?
According to literature (1,6), medical thoracoscopy uses rigid instruments or semi-flexible. There are also reports for flexible tools even though they are not widely used (7). Pulmonologists use trocars camera and biopsy forceps. They perform sites from the 4th to the 7th intercostal space in middle to anterior axillary line.
How this technique differs from the VATS according to instrumentation?
By the ‘medical thoracoscopy’, we help the diagnosis in case of malignancy TB or non-specific inflammation cases. Also we can treat some cases of pneumothorax and empyema. As you can understand, these procedures do not differ from VATS.
Why this technique is named medical?
At this point we would like to present a case of a 75-year-old male patient with recurrent right pleura effusion. The patient had undergone thoracocentesis many times before he was referred to us for pleurodesis. We performed the operation in the theatre, and we used propofol to keep the patient in mild sedation. We used two trocars, the first in the 6th intercostal space in the anterior axillary line and the second in the 8th intercostal space in the posterior axillary line. We inserted the camera in the pleura cavity, we suctioned for cytological examination, we took pleura biopsies and after talc pleurodesis we drained by tubes the thoracic cavity. And of course the patient is not intubated. A literature review (8,9) reveals many references to ‘surgical thoracoscopy’. This technique is performed almost exclusively by a thoracic surgeon. The patient is not intubated; he/she is mild sedated or under general non- endotracheal anesthesia. We use VATS instruments.
So, why this technique is defined ‘surgical’? Because of the surgeon?
Another helpful reference is to an 82-year-old male patient extremely fragile who suffers from a loculated pleura effusion, probably empyema. The patient was operated in theatre under sedation. He underwent a mini thoracotomy and two additional ports in right hemi-thorax. The procedure was as follows: we found pus and suctioned it; we removed the calcified pleura, cleaned the entire cavity with Betadine 2% solution and finally drained the thoracic cavity with two tubes. Here again arises the same question ‘why we define this technique surgical?’. Finally, as we mentioned before, we included VATS in the definitions of our technique and we was not wrong. According to the literature (10,11), many surgeons use VATS in awaken patients under local anesthesia and sedation. Researchers conclude that VATS technique has similar results and equivalent outcomes as in procedures performed under general anesthesia.
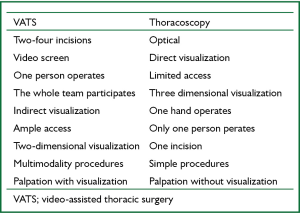
In 1996, R.Lewis (12) published in Annals of Thoracic Surgery the difference between ‘thoracoscopy’ and VATS, concluding that they are two very different procedures to each other.
However, as we can notice in this table carefully, there are no borderlines between these procedures. Nowadays we can perform thoracoscopy with video assistant so it’s rather the same with VATS. Particularly, we can have panoramic visualization cause of the use of the camera; ample access performing to three sites; palpate the lung and the pleura. We can use both our hands to operate, while our colleagues participate to the procedure. Finally, the procedure can correspond to the complexity of its case. Jakobaeus was the first to perform this technique and his name is rightly used to describe this procedure. An etymological approach to the definition of either medical or surgical thoracoscopy is helpful to further clarify the technique. ‘Thoracoscopy’ has the second component ‘scopy’ which comes from the Greek word ‘scope’ that is ‘The area covered by a given activity or subject or an area in which something acts or operates or has power or control’. VATS as we have already described can be performed under local anesthesia. So, to our understanding, the linchpin of all these techniques is ‘pleuroscopy’, which is the most appropriate definition to describe this technique. In our opinion, while independent of the operator, who as we have seen can be either an interventional pulmonologists or a surgeon, the instruments we use, the place that the operation is performed and the therapeutic or diagnostic nature of the procedure, pleuroscopy must have the following characteristics:
- The patient is not be intubated;
- The procedure refers to three actions cut - see and finally act in pleura or lung according to the operator’s skills.
I’d like to question anew ‘What do all five definitions have in common?’. They have: the not intubated patient and nothing more. This is the common point of all these (Figure 1).
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Dhanya TS, Ravindran C. Medical Thoracoscopy-Minimally invasive diagnostic tool for a trained Pulmonologist. Calicut Medical J 2009;7:e4.
- Tassi GF, Tschopp JM. The centenary of medical thoracoscopy. Eur Respir J 2010;36:1229-31. [PubMed]
- Piquet A, Giraud A. La pleuroscopie et la section des adherencesintrapleural au cours du Pneumothorax therapeutique. Presse Med 1923;23.
- Inderbitzi R, Althaus U. Therapeutic thoracoscopy, a new surgical technique. Thorac Cardiovasc Surg 1991;39:89. [PubMed]
- Miller JI Jr. Therapeutic thoracoscopy: new horizons for an established procedure Ann Thorac Surg 1991;52:1036-7. [PubMed]
- Tassi GF, Davies RJ, Noppen M. Advanced techniques in medical thoracoscopy. Eur Respir J 2006;28:1051-9. [PubMed]
- Lee P, Colt HG. Rigid and semirigid pleuroscopy: the future is bright. Respirology 2005;10:418-25. [PubMed]
- Kaiser LR, Daniel TM. eds. Thoracoscopic Surgery. Bosten: Little, Brown,1993.
- Inderbitzi R. eds. Chirurgische Thorakoskopie. Berlin: Springer,1993.
- Katlic MR, Facktor MA. Video-assisted thoracic surgery utilizing local anesthesia and sedation: 384 consecutive cases. Ann Thorac Surg 2010;90:240-5. [PubMed]
- Pompeo E, Tacconi F, Mineo D, et al. The role of awake video-assisted thoracoscopic surgery in spontaneous pneumothorax. J Thorac Cardiovasc Surg 2007;133:786-90. [PubMed]
- Lewis RJ. VATS is not thoracoscopy. Ann Thorac Surg 1996;62:631-2. [PubMed]