Perioperative factors associated with 1-year mortality after lung transplantation: a single-center experience in Korea
Introduction
Since the first lung transplantation was performed in 1963, this approach has become an effective treatment method for end-stage lung disease of various causes (1,2). The number of annual lung transplantations has rapidly increased compared to the past although the number of heart-lung transplantations is steady or somewhat declining worldwide. Most lung transplantations have been mainly conducted in North America and Europe (3). The survival rate associated with lung transplantation increased in the 2000s compared to the 1990s. And a large proportion of deaths after lung transplantation occurred within a year. The median survival of adult recipients is 4–6 years, and, especially, the median survival of recipients who survived for >1 year after transplantation is 7.9 years with good prognosis (3). Because the prognosis of recipients who survived for 1 year is very good, some researchers have reported the risk factors for predicting 1-year mortality after lung transplantation (4,5). Although the results were controversial, old age, application of preoperative extracorporeal membrane oxygenation (ECMO), decreased kidney function before the operation and preoperative diabetes mellitus were reported to affect the prognosis of 1-year morality (4-6). Furthermore, recent study showed that the age of lung transplant recipients is increasing recently and the 3-year survival rate is lower in advanced recipients, especially age 65 or older than in younger age group (7).
The first lung transplantation in Korea was performed in July 1996, and a total of 284 lung transplantations, including heart-lung transplantations, have been performed until October 2015 (8-10). Although only 1 or 2 procedures were conducted each year until 2003, currently >50 procedures are being performed each year (9). However, the lack of donated lungs and the low utilization rate of donor lungs from declared brain-dead patients are major problems associated with lung transplantation in Korea compared with other countries. In 2010, only 6.7% of donor lungs were used, which was low compared with kidney (93.3%) and liver (86.3%) (11). In the data of 2015 Korean Network of Organ Sharing (KONOS), utilization rate of donor lungs increased to 12.8% (64/500), it was still shortage for 120 patients waiting for transplantation. Therefore, selection of appropriate recipients and prediction of prognosis are important for lung transplantation in Korea.
Unfortunately, most studies about the risk factors of 1-year mortality after lung transplantation were performed on non-Asians (4-6). We supposed that the risk factors of 1-year mortality after lung transplantation in Korea might be different from those in North America and Europe, which have different circumstances and cultures (8,11). Accordingly, we reviewed the preoperative, perioperative, and postoperative risk factors of 1-year mortality after lung transplantation in Korea.
Methods
Study design and population
This was a retrospective cohort study on consecutive patients who underwent lung transplantation at a single center (Severance Hospital) in South Korea, from October 2012 to October 2015. During 3 years, 81 patients received lung transplantation surgery. Recipients who received ECMO before transplantation and those who underwent re-transplantation were excluded in order to analyze the risk factors in relatively stable patients.
All recipients received ECMO or cardiopulmonary bypass for cardiopulmonary support during transplantation surgery and were administered induction immunosuppression therapy with high dose corticosteroid using methylprednisolone 500 mg during operation and 0.5 mg/kg/day for 3 days after operation. Triple immunosuppression therapy, such as prednisolone, tacrolimus, and mycophenolate mofetil, was used for maintaining immunosuppression after transplantation. Mycophenolate mofetil were administered 1 g daily and tacrolimus concentration levels on blood were maintained from 8 to 12 ng/mL. Valganciclovir and itraconazole were used all recipients until 6 months after operation. Trimethoprim/sulfamethoxazole was used in all recipients for a lifetime to prevent pneumocystis jiroveci after operation.
All donor lungs from declared brain-dead patients were preserved in low-potassium dextran solution (Perfadex; Duraent Biologicals, Hyderabad, India). The study subjects were divided into two groups according to their 1-year survival status, and various factors were analyzed.
Data collection and definition
Data from all recipients were collected from the electronic medical records of the hospital, and donor data were collected from the Korean Network of Organ Sharing (KONOS). Recipient data including demographic characteristics, laboratory results, mortality, use of mechanical ventilator while waiting for transplantation, length of stay at the intensive care unit, and other clinical data were evaluated. Furthermore, donor data including demographic characteristics, ischemic time, and hospital stay duration were investigated.
Smoking status was defined as either ever smoker or never smoker (smoked <100 cigarettes during the lifetime). Mean pulmonary artery pressure was measured by means of right heart catheterization before transplantation. Primary graft dysfunction (PGD) was defined by consensus according to the International Society for Heart and Lung Transplantation (ISHLT) (12). Acute kidney injury (AKI) was defined as increase in serum creatinine by ≥0.3 mg/dL within 48 h or increase in serum creatinine to 30% more than the baseline value during 1 month after lung transplantation (13). Delta neutrophil index (DNI) which reflects the fraction of circulating immature granulocytes and associate with sepsis was measured preoperatively and at 24–48 h by using an automatic cell analyzer (ADVIA 2120 Hematology System; Siemens Healthcare Diagnostics, Forchheim, Germany) (14-16). The change of DNI was defined as the difference between preoperative DNI value and the highest DNI value 48h after surgery. Bone marrow density was calculated by using dual-energy X-ray absorptiometry to screen for osteopenia. Osteopenia was defined a T score of −1.0 or lower in those aged ≥50 years and a Z score of −1.0 or lower in those aged <50 years. Use of immunosuppressive agents before transplantation was defined as taking any immunosuppressive medication, such as prednisolone, mycophenolate mofetil, or azathioprine, regardless of dose or type.
Statistical analysis
All data that were represented as continuous or categorical variables were analyzed with SPSS version 23 (IBM, Armonk, NY, USA). Continuous data were presented as median with range or interquartile range. These variables were evaluated by using the Mann-Whitney U test for the difference between two groups. The chi-square and Fisher’s exact tests were used to assess differences in categorical variables, presented as number and percentage, between the two groups. The cut-off value of change in DNI before and after surgery according to 1-year mortality was determined using receiver operating characteristic (ROC). The independent risk factors for 1-year mortality after lung transplantation were identified by using logistic regression modeling that included significant variables in univariate analysis or basic clinical characteristics (17). The Kaplan-Meier method was used to create survival curves of meaningful variables, and statistical analysis of survival curves was performed using the log-rank test (18). In all analysis results, a P value of <0.05 was considered statistically significant.
Results
A total of 81 patients underwent lung transplantation during the study period. Among them, 12 patients were excluded because they received ECMO support before surgery and 1 patient was excluded because of re-transplantation.
Baseline characteristics
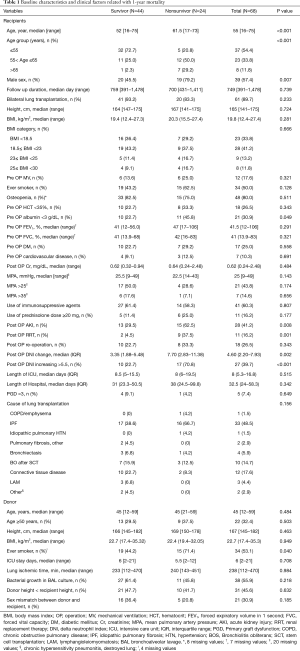
Table 1 describes the baseline characteristics of recipients and donors. A total of 68 subjects were enrolled and analyzed in this study. Forty-four patients (64.7%) lived for >1 year after lung transplantation. The median age of all patients was 55 years (range, 16–75 years), and male patients accounted for 57.4% of the total. The median follow-up duration was 749 days (range, 391–1,478 days). The major cause of lung transplantation was idiopathic pulmonary fibrosis (IPF) (48.5%); the other causes were interstitial lung disease related to connective tissue disease (17.6%) and bronchiolitis obliterans after stem cell transplantation (14.7%).
Full table
Perioperative factors associated with 1-year mortality
In the univariate analysis of clinical factors related to 1-year mortality, there was no difference between the survivor and nonsurvivor group except age, preoperative serum albumin level, AKI after surgery and change in DNI before and after surgery.
There was a high proportion of elderly recipients (P<0.001) and male recipients (P=0.007) in the nonsurvivor group. Preoperative blood sampling showed a high proportion of albumin level <3 g/dL in the nonsurvivor group (P=0.049). The occurrence of AKI after surgery was significantly high in the nonsurvivor group (P=0.008) and, especially, the need for renal replacement therapy (RRT) showed a more significant difference between the two groups (P=0.001). The change in DNI before and after surgery were more increased in the nonsurvivor group, and the proportion of recipients whose postoperative DNI increased by >5.5 which was derived through ROC (sensitivity, 70.8%; specificity, 77.3%) compared with the preoperative DNI was higher in the nonsurvivor group than in the survivor group (P<0.001). In the univariate analysis of donors, there was no difference between the two groups except the smoking status (P=0.04).
Independent risk factors were evaluated through multivariate analysis of variables that showed meaningful results in the univariate analysis and baseline variables (Table 2). The results of the analysis revealed that age 55–65 years [odds ratio (OR), 9.69; 95% confidence interval (CI), 1.68–55.77], age >65 years (OR, 146.02; 95% CI, 7.95–2,681.47), postoperative DNI >5.5 higher than preoperative DNI (OR, 11.66; 95% CI, 1.94–70.12), and need for RRT after surgery (OR, 14.01; 95% CI, 1.44–136.67) were the independent perioperative risk factors for 1-year mortality after lung transplantation.
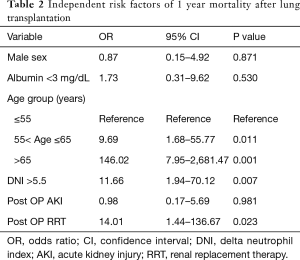
Full table
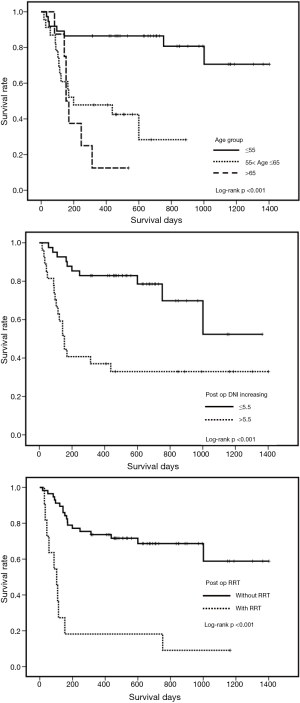
Figure 1 presents the Kaplan-Meier survival estimates of groups classified according to age, postoperative DNI >5.5 higher than preoperative DNI, and need for RRT after surgery. All graphs reached statistical significance in the log-rank test (P<0.001).
Subgroup analysis of lung transplantation in patients
We conducted subgroup analysis according to age because there might be differences in the baseline characteristics between age groups. Between patients aged ≤65 years (n=60) and those aged >65 years (n=8), we did not find a difference other than proportion of bilateral lung transplantations (96.7% vs. 37.5%, P<0.001) and the prevalence of diabetes mellitus (20% vs. 62.5%, P=0.02).
Figure 1 showed the biggest survival difference between >55 and ≤55 years age groups, therefore, we further analyzed the characteristics of subjects between >55 and ≤55 years age groups (Table 3). Bilateral lung transplantations were performed more frequently in the ≤55 years age group than in the >55 years age group (P=0.041), and the prevalence of diabetes mellitus was higher in the >55 years age group (P=0.003). Predicted forced vital capacity and forced expiratory volume in 1 second before transplantation were higher in the >55 years age group.

Full table
Subgroup analysis of the perioperative risk factors for 1-year mortality after lung transplantation in patients according to age groups in the >55 and ≤55 years age groups was performed.
In >55 years age group, 31 patients were >55 years old and 12 patients (38.7%) survived for >1 year after transplantation. Need for RRT (0% vs. 36.8% P=0.026), and postoperative DNI >5.5 higher than preoperative DNI (25% vs. 63.2%, P=0.038) were significantly related to 1-year mortality after lung transplantation in patients >55 years old.
In ≤55 years age groups, 37 patients were ≤55 years old and 32 patients (86.5%) survived for >1 year after transplantation. The occurrence of AKI after surgery (28.1% vs. 80%, P=0.042), need for reoperation (21.9% vs. 80%, P=0.021) and postoperative DNI >5.5 higher than preoperative DNI (21.9% vs. 100%, P=0.002) were significantly related to 1-year mortality after lung transplantation in patients ≤55 years old. Meanwhile, there was no significant difference in other variables including sex, height or body mass index of recipients, use of mechanical ventilation while waiting for transplantation, smoking experience, preoperative lung function, mean pulmonary artery pressure before transplantation, use of immunosuppressive agents before transplantation, and development of PGD grade 3.
Outcome
The median survival of nonsurvivors was 111.5 days (interquartile range, 62.5–161.3). The most common cause of death was infection (n=14, 58.3%), followed by cardiac arrest (n=3, 12.5%) and thrombotic microangiopathy (n=3, 12.5%). Some patients died in association with hemophagocytic lymphohistiocytosis, ischemic cholangiopathy, or bleeding. The number of recipients who were >65 years old was 8, and only 1 recipient among them survived for >1 year after lung transplantation and sepsis was major cause of death (n=5, 71.4%).
Among nonsurvivors, only 2 patients died within 30 days after transplantation due to sepsis without evidence of primary graft failure. Bacteria such as Methicillin-resistant Staphylococcus aureus, Enterococcus faecium, Pseudomonas aeruginosa or multidrug-resistant Acinetobacter baumannii grew in blood culture of 9 patients among infection patients. Four patients died due to pneumonia which occurred at least 5 months after transplantation except 1 patient. The same bacteria as results of BAL of donor lung were cultured in blood of 3 patients, which were considered donor-acquired infection.
Discussion
In this study, we investigated the independent risk factors for 1-year mortality after lung transplantation. Old age was identified as the only preoperative predictive factor for 1-year mortality. Postoperative DNI >5.5 higher than preoperative DNI and the need for RRT after surgery were revealed as postoperative predictive factors of 1-year mortality.
Several studies have reported on the risk factors or predictors of mortality after lung transplantation (4-6,19-22). However, most of those studies were performed in North America and Europe, and the environment and causes of lung transplantation in Korea are slightly different. Such differences could affect the predictors and risk factors of mortality after lung transplantation. For example, the major causes of lung transplantation in the ISHLT registry were chronic obstructive pulmonary disease/emphysema (32.1%), IPF (24.1%), and cystic fibrosis (16.2%). On the other hand, IPF (48.5%), interstitial lung disease related to connective tissue disease (17.6%), and bronchiolitis obliterans after stem cell transplantation (14.7%) were the main causes of lung transplantation in our hospital (3). In Korea, there are very few patients with cystic fibrosis compared to other countries and only one patient with cystic fibrosis received lung transplant from 2010 to 2014 (9,23). Furthermore, the registration in KONOS for patients waiting for transplantation was relatively late, and the mortality rate while waiting for lung transplantation in Korea was higher than in other countries. We supposed that late referral may be due to a pessimistic attitude of patients and physicians regarding its high mortality of early transplantation era. And priority of transplantation is given patients with ventilator or ECMO support in Korea (24-26). Therefore, IPF patients with acute exacerbation who needed for ventilator or ECMO support have a higher priority than waiting patients with stable condition.
An upper age limit for recipient selection has not been established. However, age >65 years has been considered a relative contraindication for lung transplantation (27,28). Nevertheless, as the elderly population increased, lung transplantation in elderly patients also increased (3). Tomaszek et al. reported that patients aged >60 years did not seem to show significantly poor outcome during short-term and long-term follow-up (19). However, Weiss et al. reported that lung transplantation might be performed with caution in patients older than 60 years but not in those older than 70 years (22). Our study showed that elderly recipients of lung transplantation in Korea had a worse prognosis than those in other countries. Because there might be differences in the baseline characteristics between age groups, we conducted an analysis. As a result, we did not find a difference other than in the type of transplantation, the prevalence of diabetes mellitus and major cause of transplantation. Generally, recipients of bilateral lung transplantation revealed a better median survival than those with single lung transplantation (3), and the mortality of patients with IPF and those with diabetes mellitus was reported to be higher than that of patients with other underlying lung diseases (3,6). Therefore, we supposed that these factors could be associated with high mortality in the old-age group.
AKI after lung transplantation developed in 37%, and the incidence of RRT was 5.51% in some previous studies (29,30). The prevalence of AKI and RRT in our data were higher than in previous reports (41.2% and 16.2%, respectively), the finding in our study that the need for RRT after lung transplantation increased mortality was similar to previous reports (29,30). Several studies have shown the reasons for the high risk of AKI in recipients of lung transplantation; for example, lung injury could induce inflammatory mediators of the renal epithelium, nephrotoxic agents including calcineurin inhibitors could induce direct injury, and efforts to maintain negative balance might cause kidney injury after transplantation. Furthermore, some studies suggested that patients with AKI, particularly those requiring RRT, were at an increased risk of mortality (29-32). However, the reason for increased mortality with the need for RRT is unclear. Importantly, the need for RRT after surgery could be considered a state of critical illness.
Increased DNI is known to be associated with sepsis and disseminated intravascular coagulation (33,34). However, the relationship between DNI and the prognosis after surgery is not well known. Our data showed that the changes in DNI before and after transplantation were different between the two groups, and that increasing of DNI values >5.5 especially could predict the 1-year mortality after lung transplantation. The standard DNI value of 5.5 was derived through ROC and this value was similar to those of previous studies associated with sepsis and DNI (33,34). Our data showed that the cause of death for 14 of 24 recipients (58.3%) who died within 1 year after transplantation was infection. And increasing of DNI values >5.5 was found in 11 of 14 (78.6%) patients who died within 1 year after transplantation. We hypothesized that patients with increased DNI are likely to be vulnerable to infection. An environment that promotes exposure to various pathogens and the increased proportion of elderly patients with lower physical ability among candidates for lung transplantation may be factors affecting this result.
Our study has several limitations. This was a relatively small study performed at a single center. However, this was the first study on the mortality of lung transplantation in Korea. Most previous studies were performed in North America and Europe, and their results are difficult to generalize on account of racial and environmental differences. Therefore, this study will be helpful in understanding lung transplantation in Asians. Second, this study had a retrospective design; thus, we could not systemically analyze multiple laboratory test results, perioperative factors, and preoperative performances. However, we believe that because lung transplantation is increasingly being conducted in Korea, this problem will be overcome through further studies in the future.
Conclusions
Advanced age in recipients of lung transplantation is associated with 1-year mortality after lung transplantation. Therefore, candidates for lung transplantation with advanced age should be carefully selected. The need for RRT and increased DNI after transplantation are also associated with 1-year mortality after lung transplantation; therefore, attention should be paid to patients with a possibility of having AKI and increased DNI, to improve their survival.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study protocol was approved by the institutional review board of Severance Hospital (approval no. 2013-0522-019). In addition, this study was conducted in compliance with the principles set forth in the Declaration of Helsinki.
References
- Hardy JD, Webb WR, Dalton ML Jr, et al. Lung Homotransplantation in Man. JAMA 1963;186:1065-74. [Crossref] [PubMed]
- Christie JD, Edwards LB, Kucheryavaya AY, et al. The Registry of the International Society for Heart and Lung Transplantation: 29th adult lung and heart-lung transplant report-2012. J Heart Lung Transplant 2012;31:1073-86. [Crossref] [PubMed]
- Yusen RD, Edwards LB, Kucheryavaya AY, et al. The Registry of the International Society for Heart and Lung Transplantation: Thirty-second Official Adult Lung and Heart-Lung Transplantation Report--2015; Focus Theme: Early Graft Failure. J Heart Lung Transplant 2015;34:1264-77. [Crossref] [PubMed]
- Grimm JC, Valero V 3rd, Magruder JT, et al. A novel risk score that incorporates recipient and donor variables to predict 1-year mortality in the current era of lung transplantation. J Heart Lung Transplant 2015;34:1449-54. [Crossref] [PubMed]
- Sabashnikov A, Weymann A, Mohite PN, et al. Risk factors predictive of one-year mortality after lung transplantation. Eur J Cardiothorac Surg 2014;46:e82-8. [Crossref] [PubMed]
- Hackman KL, Bailey MJ, Snell GI, et al. Diabetes is a major risk factor for mortality after lung transplantation. Am J Transplant 2014;14:438-45. [Crossref] [PubMed]
- Wigfield CH, Buie V, Onsager D. "Age" in lung transplantation: factors related to outcomes and other considerations. Curr Pulmonol Rep 2016;5:152-8. [Crossref] [PubMed]
- Haam SJ, Lee DY, Paik HC. An overview of lung transplantation in Korea. Transplant Proc 2008;40:2620-2. [Crossref] [PubMed]
- Paik HC. Current perspective of lung transplantation. J Korean Med Assoc 2016;59:119-24. [Crossref]
- Cho EN, Haam SJ, Kim SY, et al. Anastomotic Airway Complications after Lung Transplantation. Yonsei Med J 2015;56:1372-8. [Crossref] [PubMed]
- Paik HC, Haam SJ, Lee DY, et al. Donor evaluation for lung transplantation in Korea. Transplant Proc 2012;44:870-4. [Crossref] [PubMed]
- Christie JD, Carby M, Bag R, et al. Report of the ISHLT Working Group on Primary Lung Graft Dysfunction part II: definition. A consensus statement of the International Society for Heart and Lung Transplantation. J Heart Lung Transplant 2005;24:1454-9. [Crossref] [PubMed]
- Kidney Disease; Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group. KDIGO Clinical Practice Guideline for Acute Kidney Injury. Section 2: AKI definition. Kidney Int Suppl 2012;2:19-36.
- Nahm CH, Choi JW, Lee J. Delta neutrophil index in automated immature granulocyte counts for assessing disease severity of patients with sepsis. Ann Clin Lab Sci 2008;38:241-6. [PubMed]
- Harris N, Kunicka J, Kratz A. The ADVIA 2120 hematology system: flow cytometry-based analysis of blood and body fluids in the routine hematology laboratory. Lab Hematol 2005;11:47-61. [Crossref] [PubMed]
- Harris N, Jou JM, Devoto G, et al. Performance evaluation of the ADVIA 2120 hematology analyzer: an international multicenter clinical trial. Lab Hematol 2005;11:62-70. [Crossref] [PubMed]
- Steyerberg EW, Eijkemans MJ, Harrell FE Jr, et al. Prognostic modeling with logistic regression analysis: in search of a sensible strategy in small data sets. Med Decis Making 2001;21:45-56. [Crossref] [PubMed]
- Goel MK, Khanna P, Kishore J. Understanding survival analysis: Kaplan-Meier estimate. Int J Ayurveda Res 2010;1:274-8. [Crossref] [PubMed]
- Tomaszek SC, Fibla JJ, Dierkhising RA, et al. Outcome of lung transplantation in elderly recipients. Eur J Cardiothorac Surg 2011;39:726-31. [Crossref] [PubMed]
- Russo MJ, Davies RR, Hong KN, et al. Who is the high-risk recipient? Predicting mortality after lung transplantation using pretransplant risk factors. J Thorac Cardiovasc Surg 2009;138:1234-1238.e1. [Crossref] [PubMed]
- Grimm JC, Valero V 3rd, Kilic A, et al. Preoperative performance status impacts perioperative morbidity and mortality after lung transplantation. Ann Thorac Surg 2015;99:482-9. [Crossref] [PubMed]
- Weiss ES, Merlo CA, Shah AS. Impact of advanced age in lung transplantation: an analysis of United Network for Organ Sharing data. J Am Coll Surg 2009;208:400-9. [Crossref] [PubMed]
- Koh WJ, Ki CS, Kim JW, et al. Report of a Korean Patient with Cystic Fibrosis, Carrying Q98R and Q220X Mutations in the CFTR Gene. J Korean Med Sci 2006;21:563-6. [Crossref] [PubMed]
- Glanville AR, Estenne M. Indications, patient selection and timing of referral for lung transplantation. Eur Respir J 2003;22:845-52. [Crossref] [PubMed]
- Paik HC, Haam SJ, Lee DY, et al. The fate of patients on the waiting list for lung transplantation in Korea. Transplant Proc 2012;44:865-9. [Crossref] [PubMed]
- Orens JB, Estenne M, Arcasoy S, et al. International guidelines for the selection of lung transplant candidates: 2006 update--a consensus report from the Pulmonary Scientific Council of the International Society for Heart and Lung Transplantation. J Heart Lung Transplant 2006;25:745-55. [Crossref] [PubMed]
- Weill D, Benden C, Corris PA, et al. A consensus document for the selection of lung transplant candidates: 2014--an update from the Pulmonary Transplantation Council of the International Society for Heart and Lung Transplantation. J Heart Lung Transplant 2015;34:1-15. [Crossref] [PubMed]
- Hayanga AJ, Aboagye JK, Hayanga HE, et al. Contemporary analysis of early outcomes after lung transplantation in the elderly using a national registry. J Heart Lung Transplant 2015;34:182-8. [Crossref] [PubMed]
- Jacques F, El-Hamamsy I, Fortier A, et al. Acute renal failure following lung transplantation: risk factors, mortality, and long-term consequences. Eur J Cardiothorac Surg 2012;41:193-9. [PubMed]
- George TJ, Arnaoutakis GJ, Beaty CA, et al. Acute kidney injury increases mortality after lung transplantation. Ann Thorac Surg 2012;94:185-92. [Crossref] [PubMed]
- Arnaoutakis GJ, George TJ, Robinson CW, et al. Severe acute kidney injury according to the RIFLE (risk, injury, failure, loss, end stage) criteria affects mortality in lung transplantation. J Heart Lung Transplant 2011;30:1161-8. [Crossref] [PubMed]
- Al-Naamani N, Maarouf OH, Wilt JS, et al. The modification of diet in renal disease (MDRD) and the prediction of kidney outcomes after lung transplantation. J Heart Lung Transplant 2008;27:1191-7. [Crossref] [PubMed]
- Seok Y, Choi JR, Kim J, et al. Delta neutrophil index: a promising diagnostic and prognostic marker for sepsis. Shock 2012;37:242-6. [Crossref] [PubMed]
- Park BH, Kang YA, Park MS, et al. Delta neutrophil index as an early marker of disease severity in critically ill patients with sepsis. BMC Infect Dis 2011;11:299. [Crossref] [PubMed]


