Microinvasive segmentectomy in a sculpting manner: a case of VATS left S1+2 segmentectomy
Introduction
Since Jensik et al. firstly reported the result of anatomic segmentectomy for treatment of small peripheral lung cancers (1), anatomic segmentectomy has gradually gained more and more attention. Several recent literatures have revealed equivalent outcomes for segmentectomy and lobectomy with stage I NSCLC (2-4). Anatomic segmentectomy can be a suitable operative procedure for treating early-stage non-small cell lung cancer (NSCLC) with ≥50% ground glass appearance on CT (5). With less trauma and less resected lung tissue, VATS anatomic segmentectomy can be more amenable for these patients. The precise anatomical understanding and perfect performance in this procedure can still be challenging.
In this case, we described a procedure of video-assisted thoracoscopic anatomic left S1+2 segmentectomy for a 64-year-old female patient. She was diagnosed with early lung cancer in her apical segment of left upper lobe.
Surgical technique
An 8 mm GGO lesion was discovered in a 64-year-old female’s apical segment of left upper lobe 1 year ago. A follow-up CT scan showed the lesion had increased to 11 mm in diameter. A three-dimensional reconstruction of the chest CT scan was facilitated to analyze the location of the lesion and the running pattern of the vessels and bronchus. We planned to perform a VATS left S1+2 segmentectomy in this patient (Figure 1).

After intubation, the patient was placed in the right lateral decubitus position. An observation port was made in the 8th intercostal space on the mid axillary line. Another incision of about 2 cm was made in the 4th intercostal space on the left anterior axillary line and an incision of about 1.5 cm was made in the 5th intercostal space on the right posterior axillary line.
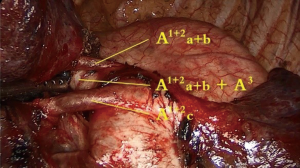
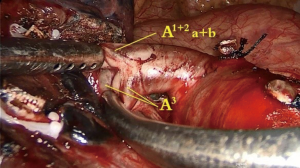
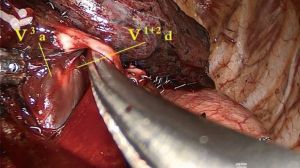
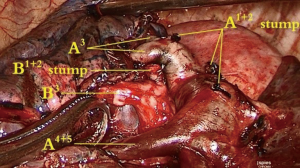
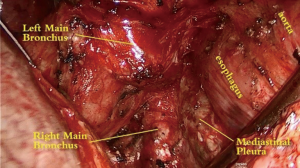
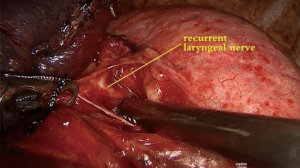
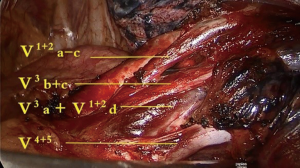
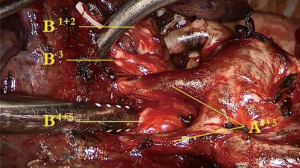
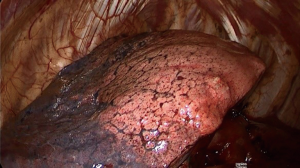
The left upper lobe was retracted ventrally. A1+2a+b and A1+2c were exposed along the left pulmonary trunk and were then skeletonized and cut (Figure 2). A1+2a+b and A3 were identified and skeletonized (Figure 3). The left upper lobe was then retracted dorsally to expose the hilum. The 5th level of lymph nodes were dissected and all branches of the superior pulmonary vein were exposed and identified, including V1+2a-c, V3b+c, V3a+V1+2d and V4+5. All the branches were skeletonized from surrounded lung parenchyma as long as possible. After the branch of V1+2a-c was cut, A1+2a+b and A3 were confirmed from the ventral side. A1+2a+b was then cut (Figure 4). The #12 and #13 lymph nodes were dissected. All the segmental bronchus of left upper lobe was exposed, including B1+2, B3 and B4+5 in order to make sure that B1+2 was cut and the other branches were preserved precisely (Figure 5). After B1+2 was identified and cut, V1+2d was expose. V3a was also exposed and preserved (Figure 6). The left upper lobe was inflated with pure oxygen and then deflated for 15 minutes. The inflation-deflation line was clear. S1+2 was cut along the line using an endostapler and removed. Intraoperative frozen sections revealed a microinvasive adenocarcinoma. A following systematic lymph node dissection was performed (Figure 7). The hilum of the S1+2 and the subcarinal area was exposed (Figure 8). The #7 lymph nodes were dissected (Figure 9). The left recurrent laryngeal nerve was exposed (Figure 10).
Discussion
We suggest the branching pattern of the bronchus and vessels should be identified precisely before every VATS anatomic segmentectomy procedure by 3D reconstruction based on CT images. Precise identification of the anatomical structure is fundamental to carry out the procedure smoothly. Careful dissection of the bronchus and vessels is vital to this technique since the branching characteristic of these structures can be highly variable in different patients. The habit of “identification before cut” cannot be over emphasized in surgeons who want to master this art. For precise anatomy of the structures, the vessels especially the branches of segmental veins should be skeletonized with cautious to prevent bleeding and to provide a clear vision.
Precise and gentle dissection in a sculpting manner of every segmental artery, vein and bronchus with the knowledge of their running pattern is the sole of the procedure. We should perform every case of VATS anatomic segmentectomy with the spirit of the craftsman.
Acknowledgements
Dr. Y Yuan was awarded “The Master of Thoracic Surgery” and was granted the Award of Excellence in the 2016 Masters of Thoracic Surgery—Uniportal VATS Lobectomy & VATS Segmentectomy Video Contest.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Informed consent was obtained from the patient.
References
- Jensik RJ, Faber LP, Milloy FJ, et al. Segmental resection for lung cancer. A fifteen-year experience. J Thorac Cardiovasc Surg 1973;66:563-72. [PubMed]
- Soukiasian HJ, Hong E, McKenna RJ Jr. Video-assisted thoracoscopic trisegmentectomy and left upper lobectomy provide equivalent survivals for stage IA and IB lung cancer. J Thorac Cardiovasc Surg 2012;144:S23-6. [Crossref] [PubMed]
- Tsutani Y, Miyata Y, Nakayama H, et al. Oncologic outcomes of segmentectomy compared with lobectomy for clinical stage IA lung adenocarcinoma: propensity score-matched analysis in a multicenter study. J Thorac Cardiovasc Surg 2013;146:358-64. [Crossref] [PubMed]
- Zhao X, Qian L, Luo Q, et al. Segmentectomy as a safe and equally effective surgical option under complete video-assisted thoracic surgery for patients of stage I non-small cell lung cancer. J Cardiothorac Surg 2013;8:116. [Crossref] [PubMed]
- Ettinger DS, Wood DE, Akerley W, et al. Non-Small Cell Lung Cancer, Version 6.2015. J Natl Compr Canc Netw 2015;13:515-24. [Crossref] [PubMed]
- Xue L, Yuan Y. VATS left S1+2 segmentectomy. Asvide 2017;4:411. Available online: http://www.asvide.com/articles/1727