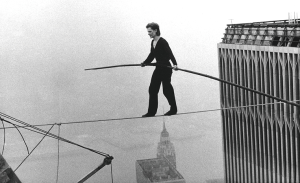
Awake minimal invasive carinal resection—tightrope walking in thoracic surgery?
On 7 August 1974, the 24-year-old French tightrope walker, Philippe Petit, captivated the world when he walked across a steel high wire suspended between the New York City's Twin Towers—without a safety net (Figure 1). More than four decades later this coup is still considered as one of the most extreme tightrope walks ever…
In their article “Non-intubated combined with video-assisted thoracoscopy in carinal reconstruction”, Peng et al. describe the feasibility of an awake, video-assisted thoracoscopic carinal resection and reconstruction in a 45-year-old patient with an adenoid cystic carcinoma of the carina (1). The work comes from a group, which is well known and respected in the thoracic community for their expertise in minimal invasive surgery and which has made major contributions to the expansion of indications for VATS from standard lobectomy/segmentectomy, to bronchial- and bronchovascular-sleeve resections. In a similar way, the technique of awake thoracic surgery has gained increasing attention worldwide in the recent past (2-4). This current publication is now the first report of a combination of both, minimal invasive carinal resection/reconstruction and awake anesthesia in a spontaneously breathing patient. Although the authors have to be complimented for their outstanding surgical performance, some words of caution have to be raised.
In medical history, first attempts of airway surgery in spontaneously breathing patients have already been reported in the late 19th century, by that time driven by the lack of adequate anesthesiological techniques. The British surgeon Stephen Paget identified five main insurmountable difficulties of awake airway surgery (5).
- Sufficient ventilation/pneumothorax. [“The collapse of the lung, when the chest is opened, is an exceedingly serious and dangerous element in the operation, adding greatly to the previous shock, and threatening at once to overpower the patient.” (5)];
- Approach. [“The difficulties of reaching the bronchus, especially upon the left side, are exceedingly great: and the risk of hemorrhage are enormous.” (5)];
- Airway reconstruction. [“Incision of the bronchus necessarily, after closure of the wound in the chest-wall, leads to increasing pneumothorax.” (5)];
- Patient movement. [“The delays in the operation from the collapse of the patient must necessarily be great. Rapid work is impossible, when the root of the lung is being dragged backward and forward at least half-an-inch in the efforts occasioned by air-hunger, and precision is almost impossible.” (5)];
- Exposure. [“To reach the bronchus is sometimes feasible: but to extract a foreign body from it, and to secure the patients recovery, is as yet highly problematical, and will require many advances in technique. The anatomical surroundings are the most essential to life.” (5)].
From this, Paget concluded that “[the] incision of a bronchus” in a spontaneously breathing patient “is an impossible operation” (5). Despite the manifold advances in thoracic surgery since that time, Paget’s principal reservations on awake airway surgery are still valid.
Precise surgical performance in combination with patients safety, are the main principles in airway surgery and especially in carinal resection. Failure to follow these principles can easily lead to catastrophic consequences and until it is proven in a reasonable large series, it must remain in discussion, whether both aspects are sufficiently guaranteed with a minimal invasive/awake technique. Today, the standard intra-operative management of patients undergoing carinal resection inheres general anesthesia, open thoracotomy and contra-lateral single-lung ventilation by cross-table intermittent conventional or jet ventilation. Results with this technique are well documented and in experienced hands, carinal resection has become a safe operation (6). Recently, the use of extracorporeal membrane oxygenation (ECMO) support for more difficult and extended resections has been proposed, since it provides maximal control over the surgical field, guarantees completely stable cardiorespiratory conditions and in this way facilitates precise surgical work (7). Again, excellent short- and long-term results have been reported with this technique by several groups (8-10). In fact, this approach represents the complete opposite strategy compared to the minimal invasive/awake procedure. Whereas the use of ECMO is only recommended for complex cases, minimal invasive/awake surgery can most likely be applied in ideal straight forward situations only. In the herein described case the tumor actually was located in the distal trachea, without reaching the carina itself and the resection obviously spared the full length of both main bronchi. One could therefore even discuss the indication, since a simple oblique tracheal resection with preservation of the carinal continuity might have been possible as well. What both approaches, ECMO for extended situations, as well as awake VATS have however in common, is the need for extensive experience of the surgeon with the particular technique.
Naturally, every new development has to compete with the outcomes of an existing strategy. Potential advantages of an awake/minimal invasive procedure could be less surgical trauma, and eventually an accelerated postoperative recovery. Given the almost 4 hours operation time for this procedure, the all together three incisions, as well as the 12 days of postoperative fixation of the chin, it has to be questioned what the real benefit is that the method can provide. In addition, there is no clear evidence that the technique itself results in more precise surgical performance, enhanced oncological radicality or improved bronchial healing. Importantly, it also remains unanswered how much of tension between the tracheal and bronchial stump in a long distance carinal resection could still be handled with this technique.
On the other hand, the procedure owns clear and relevant risks, since ventilation is limited to the delivery of high-flow oxygen through a laryngeal mask. The surgical team is inevitably confronted with a significant problem if this ventilation strategy is insufficient, especially during the opened airway-phase. Obviously, an orotracheal intubation in lateral position would be very difficult. In addition, the insertion of a cross-table tube through a port is also challenging– if required urgently. A second major limitation is that blood and secretions collecting in the airways cannot be suctioned in an awake patient due to a strong vagal stimulation.
These examples lead to the important question of a safety net “if something goes wrong”. What is the exit strategy if the patient suddenly desaturates due to spilling of blood into the open airway? Although not frequently, relevant bleeding still occurs even in standard VATS procedures, something that could easily become deleterious in the minimal invasive/awake carina resection setting. What to do if continuous hypoventilation leads to profound hypercapnia? And where are the functional limits (lung function, BMI etc.) up to which this technique can still be safely applied?
This case report on the first non-intubated VATS carinal resection highlights the surgical skills of one of the leading institution of minimal invasive thoracic surgery. The authors should be congratulated on this outstanding and impressive surgical performance, which once more pushes the limits of contemporary thoracic surgery. However, it reminds of a tightrope walk between two skyscrapers without a safety net. Although such a stunt is fascinating to watch, at least for the time being, most of us would consider it more reasonable to take the elevator and walk to the other building…
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Peng G, Cui F, Ang KL, et al. Non-intubated combined with video-assisted thoracoscopic in carinal reconstruction. J Thorac Dis 2016;8:586-93. [Crossref] [PubMed]
- Mineo TC, Ambrogi V. Efficacy of awake thoracic surgery. J Thorac Cardiovasc Surg 2012;143:249-50; author reply 250-1. [Crossref] [PubMed]
- Shao W, Phan K, Guo X, et al. Non-intubated complete thoracoscopic bronchial sleeve resection for central lung cancer. J Thorac Dis 2014;6:1485-8. [PubMed]
- Guo Z, Yin W, Pan H, et al. Video-assisted thoracoscopic surgery segmentectomy by non-intubated or intubated anesthesia: a comparative analysis of short-term outcome. J Thorac Dis 2016;8:359-68. [Crossref] [PubMed]
- Paget S. The surgery of the chest. Bristol Eng.: Wright; 1896.
- Mitchell JD, Mathisen DJ, Wright CD, et al. Clinical experience with carinal resection. J Thorac Cardiovasc Surg 1999;117:39-52; discussion 52-3. [Crossref] [PubMed]
- Hoetzenecker K, Klepetko W, Keshavjee S, et al. Extracorporeal support in airway surgery. J Thorac Dis 2017;9:2108-17. [Crossref] [PubMed]
- Lang G, Ghanim B, Hotzenecker K, et al. Extracorporeal membrane oxygenation support for complex tracheo-bronchial proceduresdagger. Eur J Cardiothorac Surg 2015;47:250-5; discussion 256. [Crossref] [PubMed]
- Lei J, Su K, Li XF, et al. ECMO-assisted carinal resection and reconstruction after left pneumonectomy. J Cardiothorac Surg 2010;5:89. [Crossref] [PubMed]
- Rinieri P, Peillon C, Bessou JP, et al. National review of use of extracorporeal membrane oxygenation as respiratory support in thoracic surgery excluding lung transplantation. Eur J Cardiothorac Surg 2015;47:87-94. [Crossref] [PubMed]


